Thriving Health Care, Inventing Cures: ‘Serving in unparalleled ways’
By Leigh DeLozier March 23, 2023Each week, Emory Report is featuring one of the six focus areas of One Emory: Ambition and Heart, the reimagined strategic framework announced by President Fenves during the Feb. 7 Charter Week gathering.
The nation is facing a range of tough issues in health care, from rising costs and barriers to access, to labor force shortages — especially in nursing — along with a multitude of financial challenges. And we will rise to meet the moment.
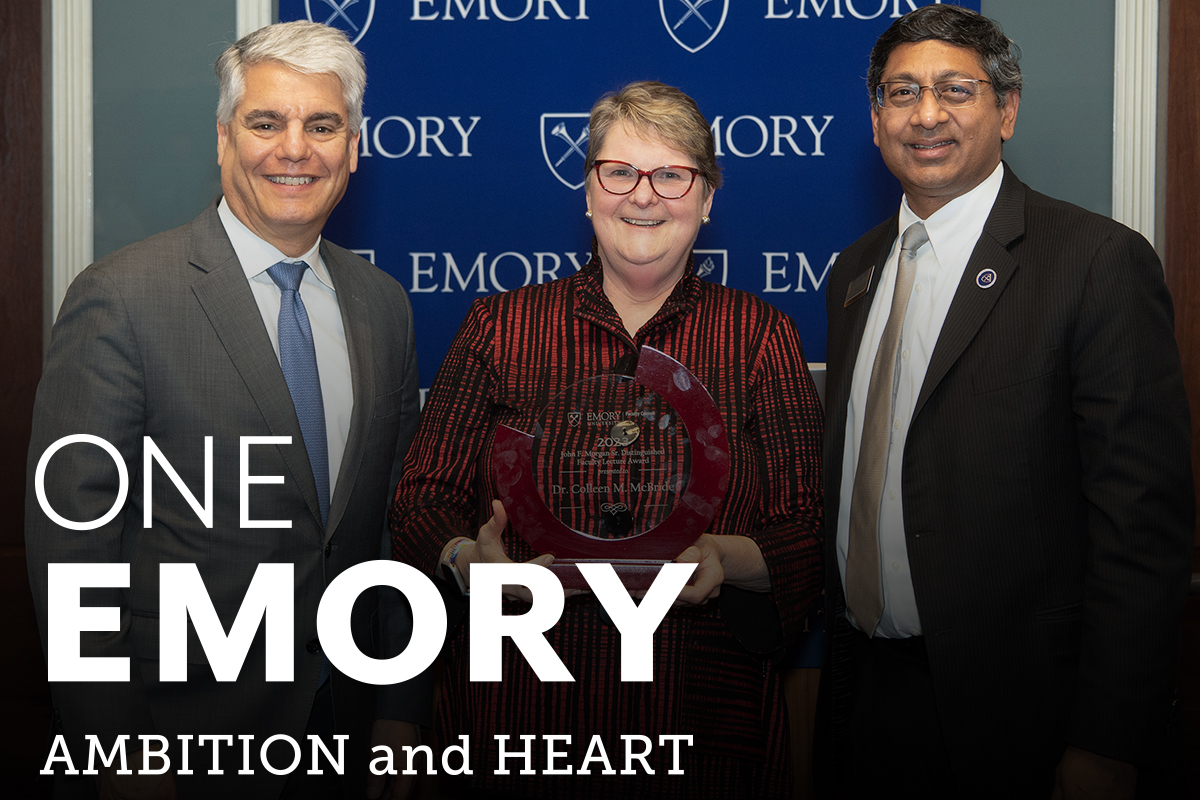
As Emory President Gregory L. Fenves introduced the renewed One Emory strategic framework, he included a new focus area recognizing Emory’s work in health sciences: Thriving Health Care, Inventing Cures.
The foundation of this work at Emory is through the entities of the Woodruff Health Sciences Center (WHSC): three schools, a national primate research center, a cancer institute, a global health institute, and the most comprehensive health care system in the state. The WHSC’s mission of education, research and clinical care undergirds all they do.
Weathering the COVID-19 pandemic reinforced how Emory’s health sciences professionals serve in unparalleled ways, Fenves said, “from frontline medical staff, physicians and nurses to the scientists who developed new treatments and evaluated everything from the vaccines to the COVID tests we use today.”
Despite the challenges, Fenves also shared his excitement about the future with Ravi I. Thadhani at the helm as executive vice president for health affairs, executive director of the Woodruff Health Sciences Center, and vice chair of the Emory Healthcare Board of Directors.
Fenves cited several goals Thadhani has established for health and health care at Emory:
- Emory Healthcare will provide the best standard of care in Georgia and the Southeast as well as the best experimental care medicine has to offer, led by our innovative physicians.
- Medical advances at Winship Cancer Institute, which is a national leader in cancer care and research, will be accelerated by the opening of the state-of-the-art Winship tower at Emory Midtown later this year.
- Emory will continue to be a trailblazer for brain health through the research and care of patients in the Emory Brain Health Center.
- Emory will continue to be among the most innovative academic centers for its development of life-saving drugs, from basic research and increasing clinical trials to translating discoveries into treatments.
“These are just a few of our health and health care goals,” Fenves said. “And as you can see, we are going to set the bar even higher in the years to come.”
Thriving Health Care, Inventing Cures: Three questions with Anant Madabhushi, professor in the School of Medicine and the Department of Biomedical Engineering
Anant Madabhushi, professor in the School of Medicine and the Department of Biomedical Engineering
“Growing up in India, I knew I would either become an engineer or a doctor,” Madabhushi says. “I continued to be passionate about medicine even when I didn’t get into medical school and knew that I wanted to be involved with medicine in some shape or form.”
Madabhushi’s uncle was a biomedical engineer with General Electric in New York. He assured his nephew there were ways to impact people through medicine, even if he wasn’t a physician.
Madabushi’s first foray into biomedical engineering was during his studies in Bombay. “I really liked programming and liked writing code,” he says. “I also was fascinated by medical imaging — MRIs, CTs. I wasn’t quite sure how to meld medical imaging with coding and programming, but was hopeful I could find a way.”
His interests solidified during his graduate and postgraduate studies. He was introduced to the world of digital pathology in the early 2000s, when pathologists were first creating high-resolution digital images of tissue slides. Madabhushi began to train an algorithm to see cancer cells on slides at earlier stages than the human eye could detect — and his passions converged into a career.
Now a global leader in developing AI to improve outcomes for individuals with cancer and other diseases, Madabhushi joined Emory in July 2022 as part of the university’s growing research community focused on advancing AI to serve humanity.
“There’s no question that health plays a major role in the AI.Humanity initiative,” he says.
Three questions with Anant Madabhushi
Q: How do you define “thriving health care”?
To me, thriving health care is about precision health care. That means we’re doing our absolute best by our patients and for our patients. We acquire so much data about every patient. Precision health care means you’re taking advantage of the totality of information about a patient to reach the most complete diagnosis and most accurate risk assessment and outcome prediction.
Q: AI is integral to the field of precision medicine. How do you explain that connection?
AI allows you to look at subvisual hallmarks or attributes, things that are beyond what even radiology or pathology can visualize. AI can see things that humans simply can’t — and that leads to better treatments.
Our goal is to drive cures. As much as we’ve learned about diagnosing and treating patients, there’s still not a good way to determine who will respond to treatment. As I’m working with clinical colleagues, my question is, “How can we do better?” For example, immunotherapy has changed the landscape of cancer treatment, but overall response rates to immunotherapy are still abysmal at approximately 25% success.
We have to do better for our patients. We can apply algorithms to what we know and use that information to help rectify imbalances. If we can determine that a patient isn’t going to respond to a particular treatment, what are the alternatives? AI can help answer that question. Physicians can use AI algorithms to modulate treatment regimens so the best therapeutic strategies are used for each patient.
Q: How do you believe Emory is poised to be a global leader in precision medicine?
Oftentimes, the translational aspect is what’s missing from research. Emory has deep expertise in biomedical research and a commitment to patient health and providing the best treatments possible.
Our providers cater to the needs of highly diverse populations. We have the ability to deploy innovative treatments to patients within the clinical workflow, and AI is part of that. Integrating AI in health care shouldn’t result in a gulf. Instead, we need to be very intentional about ways AI can improve health equity — how tools can positively impact all populations, not just select ones. Considering Emory’s involvement in global health, we can scale up what we learn and help lead the application of AI to health and medicine worldwide.
Thriving Health Care, Inventing Cures: Three questions with Zanthia Wiley, associate professor of medicine, Division of Infectious Diseases

Zanthia Wiley, associate professor of medicine, Division of Infectious Diseases
“The two strongest influences in my life are my mother and my grandmother,” says Wiley, an infectious diseases physician researcher. “These two women taught me the importance of really, really hard work and dedication to your loved ones and your community.”
Wiley first came to Emory as a medical resident; she stayed because of the opportunities she found in treating patients and training future physicians. Working as a physician during the COVID-19 pandemic further solidified those commitments.
“I realized I couldn’t stay in the safety net of taking care of individual patients,” she says. “I had to start thinking about the big picture and bigger populations. Who were the people being admitted with COVID? Where were they coming from? What were some of the factors that were increasing the likelihood of them contracting COVID?”
Those questions led Wiley to focus her primary research on attempting to describe factors that might increase the chances of Black and Hispanic persons contracting COVID-19 — and the factors that contribute to their rehospitalization.
“I’ve always been proud to be a physician. Whatever I can do, directly or indirectly, to save another life, I’ll do it.”
Three questions with Zanthia Wiley
Q: You’re a physician and researcher who specializes in infectious diseases, but will say that for you, science has never been about the lab — it’s always been about people. How do you connect the two?
I was an academic hospitalist at Emory University Hospital Midtown for ten years before pursuing a career in infectious diseases. I had the honor of caring for thousands of patients during that decade. To this day, my passion is caring for patients.
When the pandemic began, the first patient I saw with COVID was Black. The second patient I took care of was Black; the third was Black. So it didn’t take long for me to recognize that COVID seemed to be disproportionately affecting racial and ethnic minority communities. I wanted to do what I could to help them.
Q: You played an integral role in Emory’s research related to COVID-19. What are a few things you’ve learned through that work?
COVID-19 has ravaged marginalized populations, including Black and Hispanic groups. Not surprisingly, we are also seeing the disproportionate effect of long COVID on similar populations. Much of my research now focuses on long COVID, and the many questions surrounding it. What are the symptoms of long COVID? How do they affect different populations? What is the effect on mental health? How can we develop treatment options? And, one aspect that is extremely important to me: How can I help ensure that patients who look like me and who come from communities similar to where I was raised receive equitable long COVID care?
Q: What do you most love about research, and how do you hope your work — and Emory’s — can have a positive impact on humanity?
I love having the opportunity to contribute to interventions, medications and vaccinations that will save millions of lives. I now not only contribute to the care of individual patients; my research contributes to the health of entire populations.
My infectious diseases colleagues and teammates are definitely making a positive impact on humanity. The Hope Clinic, where my clinical research is based, was integral in COVID-19 vaccine research. I was an investigator in studies that resulted in COVID-19 therapeutics, including remdesivir. Emory is a major contributor to the NIH RECOVER (long COVID study), where I serve as a Hope Clinic principal investigator, and we are extremely proud that we are enrolling and studying a diverse group of research participants.
“Thriving health care” means equitable health care. It means having clinicians and researchers who mirror the communities that we serve. I want Black patients to have the opportunity to be cared for by a Black doctor. I want Hispanic patients to have the benefit of communicating in Spanish with their clinicians and seeing health care workers who remind them of themselves. Our research subjects reflect the fabric of our community. This makes me proud.