Jonathan Sybert seemed like any other man in his mid-30s. Ordinary in every way. He was healthy, active and an Army veteran. He enjoyed hobbies like playing the competitive Pokémon Trading Card Game and had recently begun to build a family, blending his life with his now wife Natalie and their four children.
That sense of normalcy and growth was suddenly disrupted last year, when Jon landed in the hospital with what doctors believed was pneumonia. He would wind up staying in the hospital fighting for his life for 203 days, supported by Natalie, their family and the team of Emory Healthcare providers who worked around the clock to save his life.
In April 2023, Jon, Natalie and daughters Layla (5), Zoey (7) Lorelei (9) and Gabbrielle (15) all came down with what they believed was just the common cold. After testing negative for COVID-19, and after their doctor said it likely wasn’t the flu, Natalie and the girls recovered within three to four days from the mysterious bug. Jon, on the other hand, got progressively worse.

Jon and Natalie with their daughters.
On April 24, 2023, Jon made his first visit to urgent care near their home in Warner Robins, looking for answers and relief. He was experiencing shortness of breath, which prompted a worried Natalie to insist that her sweetheart see a doctor to find out what was really going on with him.
During that visit, the doctor captured x-rays of Jon’s lungs and told him he might have pneumonia. They gave him an antibiotic and sent him home to keep an eye on things. Over the next few days, Jon showed some improvement and began to return to a normal routine, believing the unusual illness was finally over.
The moment of relief was short-lived.
Just a week later, while at church, Jon’s shortness of breath returned with a vengeance, accompanied by a troubling new side effect: bluish lips from lack of oxygen.
As a nurse, Natalie knew something was seriously wrong. They raced home to drop the girls off and rushed to their local hospital, still thinking that it was a persistent pneumonia.
When Jon and Natalie arrived at the Emergency Room (ER), Jon’s oxygen levels were dangerously low. Normal, healthy oxygen levels are between 90 to 100, with anything below 80 percent considered life threatening — and Jon’s oxygen levels were in the 60s.
The fact that he was still up and walking, despite gasping for air, was both astonishing and deeply alarming to Natalie and the intake team. He was immediately whisked to the pulmonary unit for swift intervention.
Days went by as doctors worked to determine what was going on. The news was bad. Jon’s condition was deteriorating, and he required higher oxygen levels to improve. On May 8, he was admitted to the Intensive Care Unit (ICU) and then three days later, the medical team informed Natalie — who was celebrating Mother’s Day weekend with her kids at the time — that Jon would need to be placed on a ventilator.
Preparing for the worst, Jon designated Natalie his power of attorney.
“It was a scary thought. I didn't know when or if I would come off the ventilator,” he says. Having Natalie there by his side to share words of encouragement and love helped him stay positive through the time of uncertainty.

Jon and Natalie reminiscing on the time they spent in Emory University Hospital.
When Jon and Natalie found out that he was going to need serious treatment and even, possibly, a lung transplant, Natalie remembers firmly saying, “Then let’s send him to Emory.”
Because the local hospital lacked the facilities to initiate or manage the treatment that he needed, they had to coordinate to dispatch a cardiothoracic team from Emory to his location to begin treatment. Teams at both hospitals would need to work closely together to plan everything out, to ensure that Jon stayed stable and received continuous care during the two-hour ride from Warner Robins to Atlanta. Transferring Jon to Emory University Hospital (EUH) was like preparing for a big move.
Once Jon arrived at Emory, he was going to need to begin something called extracorporeal membrane oxygenation (ECMO), which is a long term “by-pass machine” that supports the heart and or/lungs by taking blood out of the body, oxygenating it via an artificial lung and pumping it back into the body.
The first step in ECMO treatment is cannulation — doctors carefully insert thin tubes called cannulas into major blood vessels. These tubes connect to the ECMO machine, which then takes over the job of pumping and oxygenating the blood.
Once Jon arrived at EUH, his care team got to work figuring out the deeper issues going on with his health.
Sagar Dave, DO, remembers first hearing about Jon’s case. Dave is the associate medical director of Emory’s ECMO program and associate medical director of EUH’s cardiovascular ICU (CVICU). Dave recalls first being introduced to this young man whose illness, initially was suspected to be pneumonia, now had him cycling in and out of emergency care.

Sagar Dave and Casey Miller with the Syberts.
Dave tried to be as optimistic as possible, while remaining realistic. Jon’s situation was serious, but the entire medical team was going to work as hard as they could to help get him better.
Three days after arriving at EUH, Jon was extubated, meaning that they removed his breathing tube. Jon remembers how clouded his mind was during that time. He still cannot recall much from those days.
After removing the tube, doctors tried every possible treatment, including high dosages of steroids, but the lungs still showed no improvement. At that point, there was only one option left: A lung transplant.
To be physically stable enough for transplant surgery, Jon would now need to go through intense physical therapy. These therapy sessions, as important as they were, could be difficult and frustrating — and it began to take a toll on Jon mentally. But he knew he had to push through. At times, he needed support and encouragement from his team, while other times he needed to be pushed like he was in the Army, with his medical care team acting like his drill sergeants.
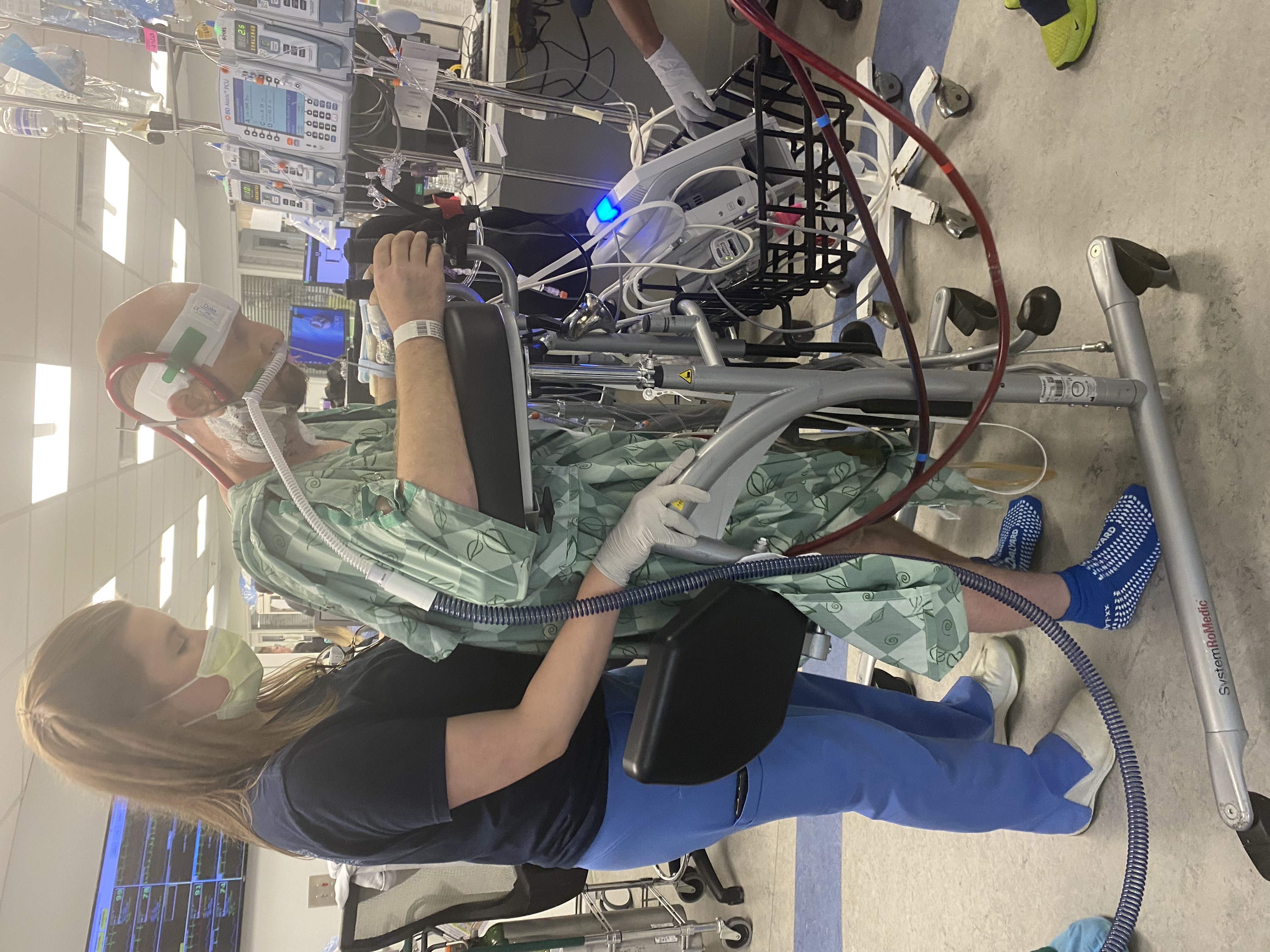
Jon and Keeley Collins, DPT during a physical therapy session.
A major requirement for Jon to receive a lung transplant was walking regularly, which he said could feel “like you just took a marathon run when all you did was take 20 or 30 steps.”
Miller and Keely Collins, DPT, Jon’s lead physical therapist, set goals for Jon. He needed to walk at least three to five laps around the unit, a baseline that would ensure he was healthy enough to go on the operating table.
Over the weeks and months that followed, the nurses and staff at EUH became like family to Jon and Natalie. They celebrated holidays and even Natalie’s birthday together, with Jon coordinating efforts with the care team to make Natalie feel appreciated beyond the four hospital walls.
The team ensured that Jon had a chance to get fresh air from time to time, even while hooked up on ECMO, and arranged special visits for their daughters, who weren’t quite old enough to be regular hospital fixtures at the time.
Dave often engaged Jon in conversations about basketball, Pokémon and anime. They would watch movies together to make Jon feel as comfortable and normal as possible. These shared moments of warmth provided a sense of belonging and support during the most challenging period of his hospital stay.
Because Jon and Natalie’s wedding had been postponed, and because the future was uncertain until Jon could get a transplant, the two decided to go ahead and get married right there in the hospital. And the team at EUH was more than happy to assist.
Natalie acquired the marriage license while Miller and Sarrah Pitman, another APP in the ICU, dove into planning the party, from picking out decorations and a cake to finding the perfect location where Jon, who was still hooked up ECMO, could comfortably say his vows.
On July 1, 2023, overlooking the Atlanta skyline on a fifth-floor balcony of the EUH Tower, surrounded by the providers who had become chosen family over the last few months, Jon and Natalie said, “I do.”

Jon and Natalie on their wedding day
As the sun sank on what had been such a happy celebration, Dave remembers how quickly the mood shifted when the overnight ICU shift began. Jon still had a long way to go before he and Natalie would be able to start their married life together.
On Aug. 28, Jon had officially been added to the lung transplant list, but he was still struggling to get his oxygen levels up to where they needed to be for an operation — so his surgery was once more put on hold. Natalie remembers thinking that “the world ended right then and there.”
It was time for Jon to once again walk the laps he had been practicing and to demonstrate the strength necessary to make it through the transplant safely.
As further motivation, Dave struck a deal with Jon. Dave would get Jon, ever the avid Pokémon player and collector, a pack of Pokémon cards for each additional lap he walked beyond his usual routine.

What a difference a year makes: Jon and Natalie return to the exact spot where they wed a year prior.
By Sept. 6, about six and a half months since his health ordeal began, Jon had a successful lung transplant. This triumph was more than just a medical win but a testament to the collective strength and unwavering hope that buoyed him along the way.
Fast forward to today, and Jon continues to enjoy a strong and steady recovery. Best of all, he and Natalie have been able to observe milestones they never would have without the ECMO care and transplantation expertise of their care team at Emory.

Finding bliss in the once overlooked simplicity of everyday moments, Jon said, he now loves simply being bored. As a reminder of where he was a year ago, a beautiful hand-crafted sign gifted to them by the ICU nurses now hangs proudly in their living room. The sign features their names, their wedding date, and the names of their children, all intertwined with a braided cross. Beneath that are the words, “A threefold cord is not quickly broken.”

