If it wasn’t for the heart transplant, there’s a good chance William Sanders wouldn’t have gotten married this fall.
Back in 2018, Sanders had been referred to Mahmoud H. Abdou, MD, an Emory cardiologist, by his primary physician. Over the next few years, Abdou was frank — Sanders’ heart wasn’t functioning as it should be, but they would try all available treatments. Interventions ranged from medication to an implantable cardioverter-defibrillator to a pacemaker and beyond.
When none of those could keep heart failure at bay, Abdou continued to be candid, and told Sanders he needed a heart transplant.
“It didn’t really resonate with me until I got home,” Sanders remembers about that visit, “and after a while I started to tell myself that I had to deal with these issues, that they weren’t going away.”
Not long after that conversation, Sanders, who was 67 at the time, also started to notice changes. He couldn’t exercise or swim anymore, he had to sleep upright, and he was “back and forth to the hospital” every few months.
During his extended stay in the hospital, Sanders stayed active, mentally and physically, and even rallied other cardiac patients to join him on short walks around the nursing station.
At the end of March, Sanders had his son drive him to the hospital.
Upon arriving, they quickly discovered that his heart was functioning at roughly 10%, so Sanders was put on a temporary mechanical pump – Impella, a device designed to give more support to the heart to allow it to pump more blood with each contraction and the blood to flow more easily.
Based on his condition, Sanders was moved up higher on the transplant list.
“Wow. It was a fight,” he says. “I was told by my nurses that every patient has to be physically ready and test well to receive a transplant. So, I walked around the nurses’ station every morning because I knew a heart was coming for me.”
It wasn’t just his own stamina he was building, either. Sanders got other cardiac patients to join him on those walks by stopping into their rooms — and eventually, the spouses and partners of fellow patients were coming to him for help.
“I told [the other patients], ‘Listen, you don’t know me, but I’m going to tell you something. You can lay in that bed all you want, but nothing is going to happen until you start getting up to walk. Until you move your body. I’ll come back and walk with you.’”
And wouldn’t you know it — it worked every time. The walks had dual benefits: physical stamina and a mental reprieve during a lengthy stay.
But Sanders’ heart was still very sick. On March 31, his condition deteriorated further, and he was placed on ECMO (extracorporeal membrane oxygenation), a long-term “bypass machine” that supports the heart and/or lungs by taking blood out of the body, oxygenating it via an artificial lung, and pumping it back in. Sanders’ priority status was also moved to the top spot on the transplant list.
When patients are on ECMO support, more and serious complications tend to occur, and if a suitable heart is not available after about a week, some difficult decisions need to be made on to how to proceed.
On April 6, after nearly 10 days in the hospital, Sanders got some tough news from his doctor, Abdou. If a heart wasn’t available in the next few days, Sanders would have to choose whether to get an LVAD, a left ventricular assist device, a surgically implanted pump used for patients with end-stage heart failure.
Sanders asked for a few days to think it over.
“After we talked, I was in my room, talking to myself and having a conversation with God, and an hour later, I’m told that they had a heart available,” he remembers. Things happened quickly after that, and the next thing Sanders remembers is waking back up in his room, with his loved ones standing over him, congratulating him on a successful transplant by Emory cardiothoracic surgeon Tamer Attia, MD, PhD.
Every step of the way, Sanders was surrounded by community he could lean on. Along with his fiancée (now wife), Bernice “Bernie” Ward, and his sister, Vera Gainey, he says he was taken care of around the clock by a host of loved ones.
Sanders said he was surrounded by family the entire time he was in the hospital waiting on a new heart. This included sister Vera Gainey, who came down from Philadelphia to be with her brother during his health battle. Photo courtesy of William Sanders.
“This experience brought people in my life that I’d been pushing out closer to me,” Sanders says, “and made me see things from a different perspective.”
Sanders’ heart problems had taken Gainey by surprise. The brother and sister are a mere 11 months apart, with Gainey being older, and have always been close — particularly since they’ve lost their other siblings and parents over the years. The two grew up in Philadelphia, where Gainey still lives, but Sanders moved to Atlanta in 1981. That distance made it easier to play his health concerns close to the vest, and she surprised him by being in the hospital less than 48 hours after he was admitted, thanks to a phone call from his son.
Gainey was struck by the number of machines in the room when she first arrived. “We went through some terrible moments, but he came back up and he persevered and was determined,” she says. “He always says this was his second birth, and that he’d do everything he could to make sure he wouldn’t leave me.”
Originally, Sanders hadn’t been forthcoming with his fiancée, Ward, either. “When I started getting sick, I started avoiding her,” Sanders says, “but she never would go away.” Ward kept bringing food over and checking in — after 28 years of friendship, she knew something was wrong.
While the two had been on a few dates years ago, Sanders said it wasn’t serious, as he hadn’t planned to ever remarry after his divorce. But when he was sick, Ward was there every step of the way, and he started to see things from a new perspective.
“Bernie is magnificent. I don’t know how I almost let her get away, but I’m holding on tight this time,” he says. The two tied the knot on Nov. 18.
After the transplant, Gainey and Ward worked together to get Sanders comfortable with his medication routine — which often changed, in the beginning — and orchestrated follow-up visits, including to rehab. In fact, a support system is so critical that it’s one of the considerations for transplant eligibility.
Emory cardiothoracic surgeon Tamer Attia, MD, at left, performed the successful heart transplantation surgery on Sanders. Photo courtesy of William Sanders.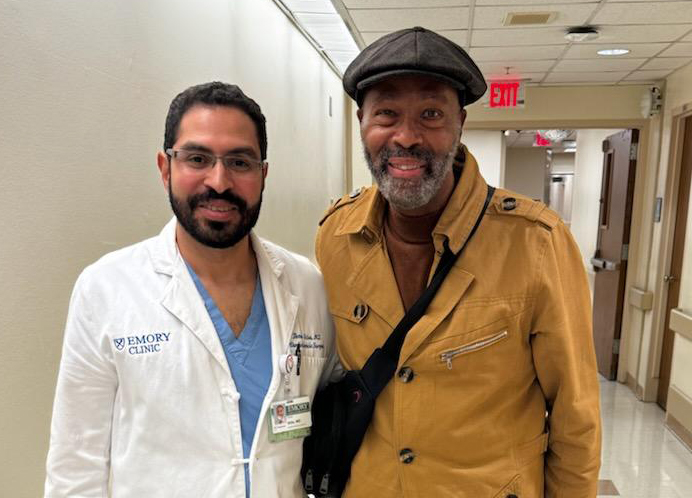
One of Meredith Hardie’s favorite things about Emory Decatur Hospital’s Cardiac Rehabilitation program being offered in the Wellness Center is that it allows the family to get involved, too.
As cardiac and pulmonary rehabilitation manager, Hardie has seen the impact of accountability buddies first-hand, whether that’s for regular exercise or at nutrition classes, and says, “We definitely encourage the family members, spouses and caregivers to come along.”
Erin Hill, cardiac rehab RN, explains that rehab patients often come in with a fair amount of anxiety — and plenty of questions.
When Sanders started rehab on July 31, he had questions, but he was enthusiastic, too.
“He’s been a star patient, and I wish we could clone him,” laughs Hill. During his rehab intake, Sanders shared his concerns and goals with Hill, who walked him through the treatment plan and allayed any fears.
“He’s always positive when he comes in and receptive to what we have to say,” says Hill. “Organ transplant is a huge deal, and it involves frequent follow-ups and monthly biopsies, where patients have to return to the lab and have tests done to make sure there’s no organ rejection. There is also a huge number of medications they have to take, so the fact that he’s been able to maintain his positivity through all of it is incredible.”
Organ transplant patients also start on a different care plan compared to cardiac event patients. Most notably, transplant patients have more restrictions around driving and heavy lifting in order to let their sternums heal. And, because transplanted hearts are not connected to the brain via nerves, it requires longer warm-up and cool-down periods, along with lower-intensity workouts.
Exercise physiologist Marcus Meadows has seen Sanders make significant progress. “Will was coming in with a completely different heart, trying to do anything to build himself back up,” Meadows says. “He was struggling to do three laps around the track, and his heart rate was really elevated — which is a normal response with a transplant. Now, he’s able to go six laps without shortness of breath.”
Cardiac output is closely monitored throughout rehab exercises so that potential problems can be stopped before they begin. Meadows explains that being able to look at reports with patients is essential to those patients feeling comfortable enough to exercise at home.
Gainey has also seen significant progress in her brother. Originally challenged to walk around his car in the driveway, Sanders is now going to physical therapy, doing water aerobics, walking his dogs and traveling with friends. Knowing her brother was in the clear, she was comfortable going back home to Pennsylvania.
“The care team was phenomenal,” Gainey says. “The therapists couldn’t believe the energy he has, but it’s really because of all the love he’s gotten from them throughout this process.”
Since his surgery, Sanders has become a star patient at Emory Decatur's cardiac rehab facility — and the outlook is sunny.
Because patients go to cardiac rehab up to three times per week for two- to four months, they develop deeply personal relationships with the providers. Hill and Meadows both love building rapport and helping patients reach their goals, literally building back up after a life-altering event.
For Meadows, this case turned out to have even deeper personal ties.
“Will brought it up to me that I met him when I was about five years old,” Meadows says. Turns out, Sanders had worked with Meadows’ father in the Atlanta Police Department and the two have stayed friends throughout career changes.
“Once I told him my last name, he pieced it together and called my dad right on the spot,” Meadows laughs. “Having that connection with him and being able to help him through this process was really cool for me. It all comes full circle.”
Full circle, indeed, as even one of Sanders’ first visits was back to the hospital. This time, to say thank you. Sanders is also looking forward to volunteering in the future — no surprise from a patient who was encouraging others to walk while waiting on his own surgery.
“I wouldn’t go to any other hospital because the level of care that Emory had rendered to me is second to none,” Sanders says. “It wasn’t only the doctors that made me feel good, but it’s the people who weren’t the doctors, from nurses to therapists to custodians and beyond. You can’t put a price tag on that.”

