Chunhui Xu was on hand at Cape Canaveral when the International Space Station’s SpaceX Crew-8 mission launched in March 2024, but her excitement was less about the rocketry and more about the rocket’s special cargo of beating heart cells.
“The idea behind cell therapy is to regenerate new muscle,” Xu says. “But survival is the issue. For the heart muscle specifically, once it’s damaged, it cannot regrow. After you inject new cells into the injured area, many of them are lost.”
Following earlier research on cancer cells that grew faster in space, Xu’s team first tried to simulate microgravity by placing heart cells in a random positioning machine, which constantly shifted the cells so they never got used to a single direction being up or down. The increased survival rates of these cells led them to ask whether the special environment of space might trigger molecular changes in heart cells that would make them more likely to survive once injected into a patient on earth. “In space, the cells can actually sense that new environment and make changes,” Xu says.
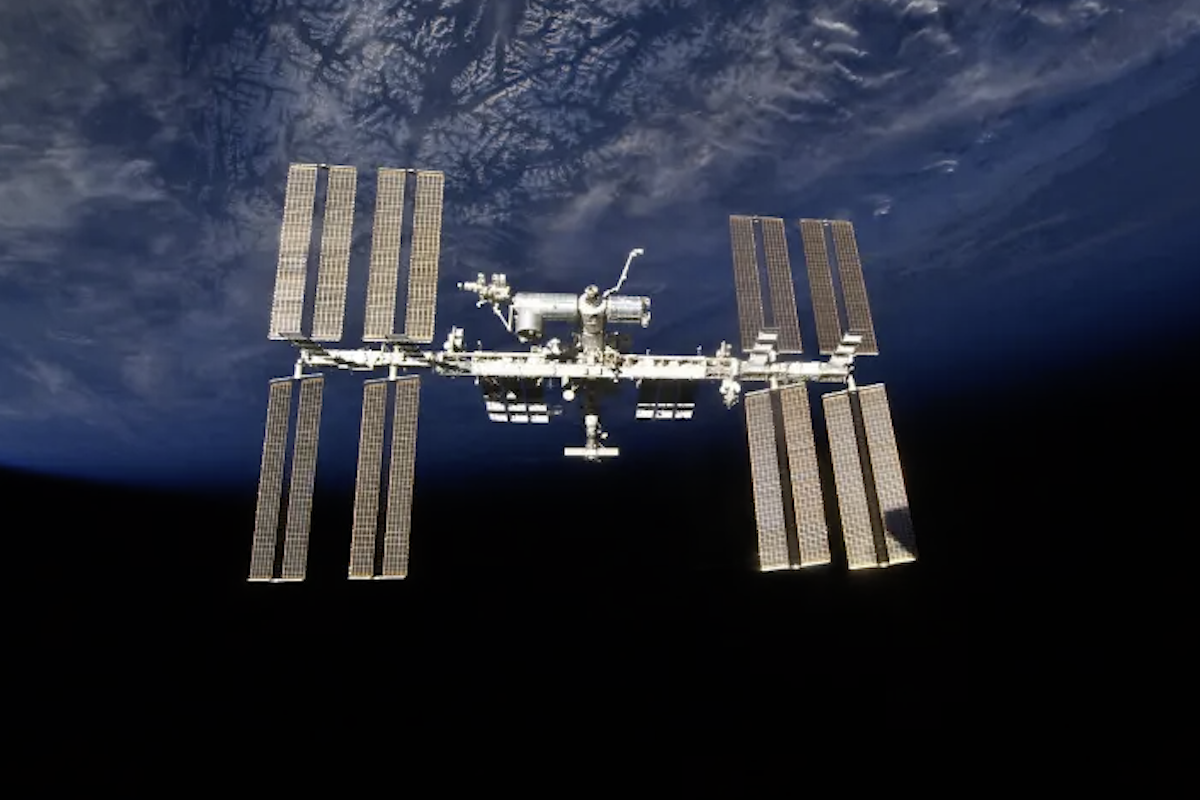
The journey from the lab to the space station
Xu’s research, published in Biomaterials, used special heart muscle cells that contract at regular intervals and, working together, cause the cells to beat like a normal heart. The cells were produced from generic human stem cells that could be turned into multiple different cell types. Similar groups of cells had previously been shown to prevent heart failure in preclinical experiments. This led many researchers to conclude that if they could find a way to make the cells survive longer in cell-based heart therapy, there could be an inexhaustible supply of new cells for human heart repair. The challenge was to find ways to improve the survival rate of the transplanted cells.

Flight Engineer Jasmin Moghbeli works aboard the International Space Station in March 2024 to retrieve bags containing heart cells for Prof. Chunhui Xu's experiment
NASA
They then returned live cell cultures to earth after the cells had been in space for eight days. When spaceflight was completed, both the earthbound and the space-traveling cells were characterized to study which molecular changes had taken place that were unique to the cells that had experienced microgravity. The results were complex but pointed to a pattern of increased production of proteins involved in cell survival.
Understanding how the microgravity environment changes the molecular activity of heart cells to make them more survivable could be a big step in using those cells to effectively repair damaged hearts. It will require a systematic understanding of all the processes of cell survival and growth for heart muscle cells under stress conditions. This may help lead to ways to create heart cells on earth with improved survival rates.
“Rather than sending cells to space,” Xu says, “We basically have to work out new ways to understand the molecular changes that push the cells to improve their survival, so we can manipulate these changes in the cells when we prepare them on earth. Then we hope to generate a new strategy to make better cells for cell therapy.
This study was conducted in collaboration with BioServe Space Technologies and Georgia Institute of Technology with funding from National Science Foundation and sponsored by the ISS National Laboratory.
Citation: Forghani, P., et al. (2025). Spaceflight alters protein levels and gene expression associated with stress response and metabolic characteristics in human cardiac spheroids. Biomaterials, 123080.