In a retrospective study, a team of researchers from several health care systems and universities, including Emory University, has discovered a new artificial intelligence (AI)-derived biomarker that uses routine imaging scans to help predict which patients with lung cancer will respond to immunotherapy. The findings, which were published in a recent article in the journal Science Advances, not only offer guidance for patients and their physicians making treatment decisions, but can also curtail the financial burden associated with immunotherapy.
“The ability to predict response to immunotherapy merely from a baseline CT scan would be a game changer because if we find out which patients will and will not respond to therapy, we can offer different therapeutic modalities,” says Mohammadhadi Khorrami, PhD, first author on the study and postdoctoral fellow in the Wallace H. Coulter Department of Biomedical Engineering at Emory University School of Medicine and Georgia Institute of Technology College of Engineering. “Moreover, with the staggering costs of immunotherapy — around $200,000 a year per patient — the need to non-invasively determine this response before initiating therapy becomes crucial.”
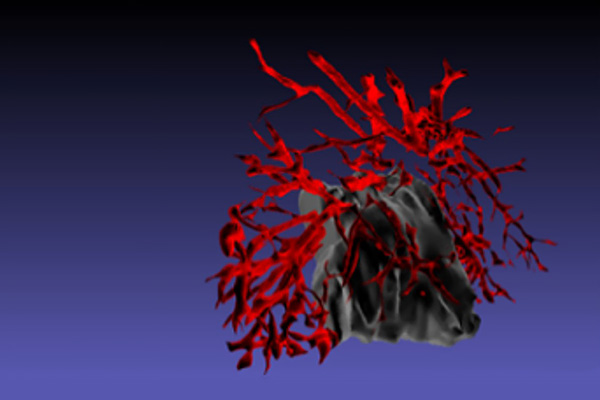
The new biomarker, quantitative vessel tortuosity (QVT), examines features of blood vessels surrounding tumors, which can influence tumor behavior and therapeutic resistance. Tumors appropriate the body’s machinery for building new blood vessels and redirect as much blood as possible to the tumors so they can grow faster and spread throughout the body. Compared to normal blood vessels, tumor-associated vasculature is chaotically arranged and twisted.
Khorrami and his colleagues used AI tools to evaluate different aspects of QVT biomarkers in more than 500 cases of patients with non-small cell lung cancer before and after they were treated with immune checkpoint inhibitor (ICI) therapies, a type of immunotherapy. The researchers discovered that the tumor vasculature of patients who do not respond to ICI therapies is more twisted compared to those who do respond. They hypothesize that blood vessel twistedness causes antitumor cells to accumulate at the tumor site but fail to efficiently infiltrate the tumor, diminishing the effectiveness of immunotherapy.
“Our imaging biomarker is validated in genomic, molecular and cellular scales and could potentially serve as a tool for better identification of non-small cell lung cancer patients who are likely to benefit from immunotherapy,” says Mehdi Alilou, PhD, study co-first author while at Case Western Reserve University and now senior AI engineer at the VW Innovation and Engineering Center.
These findings are important because immunotherapy is often the first line of treatment for patients with non-small cell lung cancer, which represents 84% of all lung cancers, according to the American Cancer Society. However, most patients don’t achieve durable results from ICI therapies.

Anant Madabhushi, PhD
“Immunotherapy only tends to benefit approximately 30% of patients. With the high expense of treatments and a 70% failure rate, we have to find better ways to predict and monitor responses to therapy,” says Anant Madabhushi, PhD, study author and professor in the Wallace H. Coulter Department of Biomedical Engineering at Emory University School of Medicine and Georgia Institute of Technology College of Engineering, and member of the Cancer Immunology research program at Winship Cancer Institute of Emory University. “When making decisions on who to treat and how to treat them, clinicians really need interpretable features. Vessel tortuosity is a novel radiomics method that uses an interpretable and intuitive AI approach to evaluate whether the tumor is responding to therapy even before more obvious changes like tumor size become apparent.”
Study collaborators included Case Western Reserve University, Cleveland Clinic, NYU Langone Health, Stony Brook University, University Hospitals in Cleveland and Weill Cornell Medicine Physicians.
“Our approach to quantitatively measure abnormal growth of blood vessels can help develop a dynamic way to measure and monitor these changes prior to and in response to treatments,” says Vamsi Velcheti, MD, FACP, FCCP, medical director of the thoracic oncology program at NYU Langone’s Perlmutter Cancer Center and co-author on the study. “This could pave the way to a novel diagnostic approach for combination strategies with immunotherapy.”
In future work, the researchers will seek to validate QVT biomarkers in prospective clinical trials.