Emory University received a National Institutes of Health grant, for a total of $883,000 over two years, to develop a sensor capable of detecting SARS-CoV-2, the virus that causes COVID-19, in the air of indoor spaces. The grant is part of the NIH RADx Radical initiative, which aims to support new, non-traditional approaches for rapid detection devices that address current gaps in testing for the presence of SARS-CoV-2, as well as potential future pandemic viruses.
“Our goal is to create a fully automated electronic sensor that continually measures for the presence of SARS-CoV-2 in the environment in real time,” says Khalid Salaita, principal investigator of the grant and an Emory professor of chemistry. “The sensor could be used in schools, airports or any high-traffic indoor areas.”
The new sensor will potentially have the flexibility to be re-programmed to detect other dangerous strains of viruses that may emerge, he adds. “Even after we get the COVID-19 pandemic under control, the demand for viral sensing will remain,” Salaita says, noting that the new sensor will take at least two years to develop.
Salaita, a leader in biophysics and nanotechnology, is also on the faculty of the Wallace H. Coulter Department of Biomedical Engineering, a joint program of Georgia Tech and Emory.
Co-investigators of the grant include Gregory Melikian, a professor at Emory School of Medicine, in the Department of Pediatrics’ Division of Infectious Disease; and Yonggang Ke, assistant professor at Emory’s School of Medicine and the Wallace H. Coulter Department of Biomedical Engineering.
The project will work to adapt the technology of a DNA micromotor, developed in 2015 by the Salaita Lab and further enhanced through collaboration with the Ke Lab. The Milikian Lab will generate harmless, engineered viral particles that mimic the real virus, and its potential mutants, to allow the team to test and validate the technology.
Emory graduate Kevin Yehl (now on the faculty of Miami University) developed the micromotor with Salaita while he was a PhD student in the Salaita Lab. It is the first rolling DNA motor, and is capable of sensing, leading the researchers to dub it the “Rolosensor.” It won a bronze medal in the 2016 Collegiate Inventors Competition, the foremost program in the country encouraging invention and creativity in undergraduate and graduate students.
The Rolosensor, about the size of a human red blood cell, consists of hundreds of synthetic DNA strands, or “legs,” bound to a sphere. The DNA legs are placed on a glass slide coated with the reactant: RNA. The DNA legs are drawn to the RNA, but as soon as they set foot on it they destroy it through the activity of an enzyme called RNase H. As the legs bind and then release from the substrate, they guide the sphere along, allowing more of the DNA legs to keep binding and pulling.
“When we first developed the motor it was initially out of pure curiosity,” Salaita says. “We wondered if we could convert chemical energy into mechanical work and make something move.”
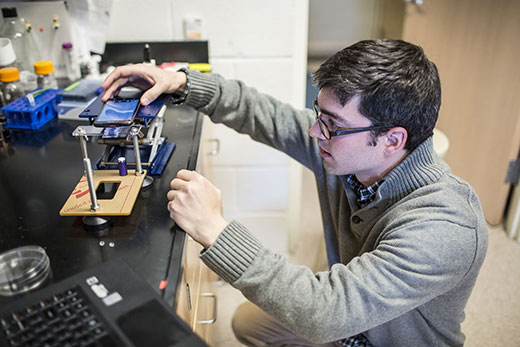
The researchers soon realized that anything that resists the motion of the rolling motor slows its speed. The speed of the motor can be monitored by attaching a clip-on microscope lens to the camera of a smart phone. They showed that the Rolosensor can detect a single DNA mutation by capturing videos of the particle motion to measure particle displacement. The team was awarded a patent in 2020 to use the simple, low-tech method for doing diagnostic sensing in the field, or anywhere with limited resources.
Even during the few months early in the COVID-19 pandemic that his lab was temporarily shut down, Salaita began to think about how the Rolosensor might be adapted to detect SARS-CoV-2.
He began discussing the idea with Melikian, a virologist who worked on HIV and other viruses but had also pivoted to take on the challenge of SARS-CoV-2. The Melikian Lab figured out a way to make “pseudo” viral particles with spikey proteins that mimic those of SARS-CoV-2.
“These pseudo viruses, which are harmless and do not replicate, will provide a way for us to test and optimize the assay as we try to adapt our rolling motor to detect SARS-CoV-2,” Salaita explains.
The plan calls for the Ke Lab to help make the body of the rolling motor “sticky” to the SARS-CoV-2 viruses, but not to any other virus or material, by using DNA structures that function like Velcro. The Rolosensor will be embedded into a microchip, where it will roll across the surface unless it encounters viral particles that cause it to stick. A camera will continuously record the speed of the motors. If a motor stalls, it will trigger an electronic alarm signal at a central monitoring station.
“Imagine an unobtrusive, encased device, similar to a smoke detector, that continuously samples the air,” Salaita says. “A central server on a cloud could collect data from numerous devices, in an airport, for example, and send out an alert for a SARS-CoV-2 detection event, including the GPS coordinates, whenever a motor stopped.”
An additional key collaborator is Primordia Biosystems, Inc., a company that specializes in building microfluidic chips that can sample virus-containing aerosols in the air.
The motors can run for up to 24 hours, allowing for fully automatic viral sensing, without the need for sample processing or other human intervention.
Three Emory PhD chemistry students in the Salaita Lab have collected preliminary data and will conduct the experiments and tests needed to complete the project: Alisina Bazrafshan, Selma Piranej and Yuxin Duan.
Many hurdles remain to develop a prototype for an indoor air sensor for SARS-CoV-2, Salaita says, including concerns such as sensitivity of the device and whether it would generate false positives. The longer-range goal is to adapt the rolling motor device so that it could be programmed to effectively detect high levels of any virus of concern in an indoor air space.
“One thing is for certain, there is a need for viral-detecting devices for public indoor air spaces and many researchers are working to try to meet this challenge,” Salaita says. “We hope our project will yield another important air-monitoring tool as we enter an era when pandemics will likely become more common.”