Glioblastomas, the deadliest type of brain tumor in adults, attract “turncoats.” These are macrophages, a type of immune cell, which promote tumor progression and mask tumors from the immune system’s scrutiny. To better understand the cells that brain tumors recruit, scientists led by Dolores Hambardzumyan, PhD, developed advanced imaging techniques to visualize macrophages found in the brain tumors of living mice.
The results were published Monday, June 24 in PNAS.
The researchers demonstrated that depending on where these macrophages originated, their appearance and behavior vary significantly. Hambardzumyan and her colleagues say their results provide support for a strategy that would block macrophage infiltration into brain tumors as part of cancer treatment.
“This research provides the scientific community with a novel mouse model to study the populations of glioblastoma-associated macrophages both separately and together,” Hambardzumyan says. “Our results also demonstrate the efficacy of blocking macrophage infiltration and calls for the use of combination therapies to enhance patient survival.”
Hambardzumyan is associate professor of pediatrics at Winship Cancer Institute of Emory University and Aflac Cancer and Blood Disorders Center at Emory and Children’s Healthcare of Atlanta.
Tumor-associated macrophages come from two distinct sources. They can come from the peripheral blood supply, or they can be microglia: cells that are already resident within brain tissue. The Hambardzumyan lab has previously demonstrated macrophages coming from the blood are much more prevalent in number and aggressive in behavior, compared to macrophages coming from the brain.
“In order to develop more effective immunotherapies to treat glioblastoma, we must first understand the properties of each of these macrophage populations individually rather than treating them as one homogenous entity,” says Zhihong (“Z”) Chen, PhD, a postdoctoral instructor and the co-first author of the paper.
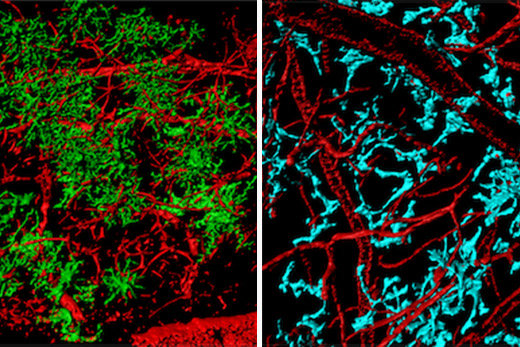
The researchers developed a mouse model which allows them to observe infiltrating macrophages in real time inside the tumor. The mice are genetically modified (also, some received bone marrow transplants) so that only particular groups of macrophage cells produce fluorescent proteins, making peripheral blood-derived macrophages or brain microglia visible under a microscope.
The team installed a clear imaging window made of thin glass over the brain tumor and utilized advanced techniques including two-photon imaging to observe macrophages over time as they move through and interact with the tumor. They were able to image cells as deep as 500 micrometers in the tumor and up to several hours at a time.
“We were very excited with these unprecedented observations we were able to make by leveraging these technical advancements,” says Cancer Biology graduate student James Ross, who is co-first author.
They found clear morphological and behavioral differences between macrophages coming from the blood and brain resident macrophages. They show blood derived macrophages are smaller, more motile cells that zip around the tumor along blood vessels. On the contrary, they found brain-resident macrophages to be large, highly branched, and immobile cells that have minimal migratory behavior.
To test the efficacy of blocking the infiltration of the blood derived macrophages, they treated mice with a drug (anti-VEGF antibody or bevacizumab) that normalizes the irregular vasculature of glioblastomas. This drug has been used in the clinic to treat glioblastoma and improve quality of life in patients. The research team observed fewer macrophages in the tumors that were treated, and they observed an increase in survival in these mice. They also observed a morphological switch in the macrophages, indicating that not only can the infiltration of these cells be inhibited but their state of differentiation may also be affected.
Despite aggressive therapeutic strategies, the average survival for patients with glioblastoma is only 12 months. One reason for this dismal outcome is that current therapeutic strategies fail to effectively target properties of other cell types within the tumor, such as tumor-associated macrophages. The Hambardzumyan lab is now actively seeking to find new therapeutic approaches, such as blocking macrophage infiltration in combination with immune checkpoint inhibitors to treat these deadly brain tumors.
The research was supported by the National Cancer Institute (F31CA232531) and the National Institute of Neurological Disorders and Stroke. (R21NS106554-01).