An unprecedented technique to peer into the workings of a brain tumor has won a Winship Cancer Institute of Emory University investigator and her team a $4 million grant from the National Cancer Institute.
Glioblastoma is the most aggressive form of primary brain tumors. While doctors have strived for years to develop new therapies for this disease, only incremental progress has been made. Standard imaging modalities such as MRI and CT scans do not accurately depict what is happening within the brain and within the tumor of a person being treated with chemotherapy and radiation.
“Right now, I have a patient who is doing great and exercising a lot, but the recent MRI has demonstrated possible progression,” said William Read, a medical neuro-oncologist at Winship.
That is one reason why work headed by Winship investigator Hyunsuk Shim and her colleagues, neurosurgeon Jeffrey Olson and radiation oncologist Hui-Kuo Shu, recently attracted a five-year grant from the National Cancer Institute (NCI). This team of brain tumor researchers has been using a unique way to peer into the brain to determine whether a certain drug therapy may be effective at treating these notoriously resistant brain tumors.
“This is huge,” says Olson. “It lets us see something we otherwise couldn’t see, something that can help us make best decisions for our patients. Glioblastoma is just an awful disease, and anything that can lighten the burden is tremendously important. No one else is doing anything close to this.”
The U01 grant from the NCI also places Winship into an elite network of NCI-designated cancer centers that studies quantitative imaging methods to measure tumor response to therapies in clinical trial settings. The Quantitative Imaging Network, which now includes 16 cancer centers with the addition of Winship into its ranks, is awarded through a highly-selective NIH peer review process.
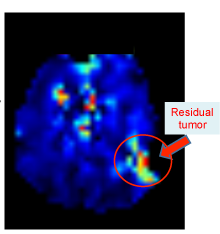
The imaging technique that the Winship team is developing to quantitatively assess how glioblastoma patients are responding to therapies is magnetic resonance spectroscopic imaging, or MRSI. Unlike the standard MRI which only gives structural information on the tumor and surrounding brain, MRSI can peer further into the tumor to detect changes in its metabolism, which may indicate how fast a tumor is growing, shrinking or dying.
Shu adds, “We are just not making enough progress in this disease. I think many new therapies have been disappointing when tested on trials because there is no selection for patients that are more likely to benefit. The use of MRSI in this project is our attempt at finding a way to better tailor therapy for individual patients depending on their treatment response.”
Their study focuses specifically on vorinostat, a histone deacetylase (HDAC) inhibitor, which has the ability to alter the structure of tumor DNA and change cancer metabolism. This drug is FDA-approved for use in cutaneous T-cell lymphomas but has not been shown, to date, to be effective at treating glioblastomas. Aided by MRSI, investigators will be able to measure the levels of eight different, potentially important metabolites within the tumor and surrounding brain, which they believe, in turn, will let them know whether vorinostat is working.
While MRSI is not necessarily new, the technology used on this study represents the latest advance in the field and will allow clinically useful whole brain scanning at resolutions that are not achievable by commercially available systems. In addition, their project will utilize Velocity AI, an imaging archival and registration system that was developed by Tim Fox and Ian Crocker of Emory’s Department of Radiation Oncology, co-investigators on this study. This Emory-developed system will permit quantitative assessment of MRSI in the context of standard MRIs that will also be obtained as part of the standard follow-up for these glioblastoma patients.
“While we are testing whether MRSI can predict response to vorinostat, our hope is that this technique could be used to assess response to other drugs besides vorinistat,” Shim says. “It is better to figure out as early as possible which patients a given drug is working for.”
While having the ability to utilize more advanced imaging technologies is important, this will not make a significant difference in patient care unless these techniques can be readily transferred across institutions. Therefore, another important part of their study is to be able to demonstrate that MRSI can be reproducibly obtained across sites. The Emory team has therefore recruited researchers from Johns Hopkins University to participate in this study. Through this collaboration, they hope to demonstrate that this imaging technology can be effectively disseminated for use at other sites.
