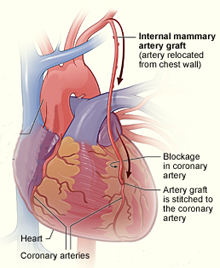
Hybrid revascularization is a minimally invasive blend of coronary bypass surgery and stenting. Surgeons avoid opening the patient’s sternum, which facilitates recovery, while keeping the durability of bypass surgery for the most important of the blocked coronary arteries.
Image courtesy of NHLBI.
The first multicenter study of hybrid revascularization shows that the emerging procedure for treating coronary artery disease has a similar rate of major adverse events in the first year, compared with percutaneous intervention (stenting).
Hybrid revascularization is a minimally invasive blend of coronary bypass surgery and stenting. It has been described as a “best of both worlds” strategy for treating multi-vessel coronary artery disease. Surgeons avoid opening the patient’s sternum, which facilitates recovery, while keeping the durability of bypass surgery for the most important of the blocked coronary arteries.
John Puskas, MD, professor of surgery and associate chief of cardiothoracic surgery at Emory University School of Medicine, was national principal Investigator of the study and presented the results on Sunday at the American College of Cardiology meeting in San Francisco.
Participating institutions included: Brigham and Women’s, Columbia, Duke, Emory, Lankenau Hospital (Pennsylvania), Montefiore-Einstein Heart Center, Ohio State, University of Maryland, University of Pennsylvania, University of Virginia and Vanderbilt. The data coordinating center was housed in the Department of Health Evidence & Policy at the Icahn School of Medicine at Mount Sinai in New York. The study was funded by a Challenge grant (RC1 HL100951) -- part of the 2009 American Recovery & Reinvestment Act -- from the National Institute of Health’s National Heart, Lung, and Blood Institute (NHLBI), and was conducted in association with the NHLBI Cardiothoracic Surgery Trials Network.
The prospective cohort study enrolled 200 patients in the hybrid group and 98 who would have been eligible for a hybrid procedure, but had multi-vessel percutaneous intervention (PCI) instead.
“We started by taking a snapshot of each participating center’s catheterization lab over three months,” Puskas says. “That was more than 6,500 patients, but only a fraction were eligible. They had to have a pattern of coronary artery disease that could be reasonably treated with either hybrid techniques or multivessel percutaneous intervention: both an LAD (left anterior descending) lesion and a significant stenosis in at least one other non-LAD coronary artery. This was a group of patients with low to medium complexity coronary artery disease.”
The primary measure of safety was the rate of major adverse coronary and cerebrovascular events (MACCE: includes death, heart attack, stroke or repeat revascularization procedure). During the first year, hybrid patients had a MACCE rate of 11 percent (0.143 events per patient-year) while PCI patients had a rate of 10 percent (0.119 events per patient year), with hybrid revascularization displaying a trend toward a MACCE rate lower than PCI after the first year. Patients were followed for up to an average of 17.5 months and during that time, the MACCE rate for hybrid revascularization patients was 0.868 times that for PCI patients, adjusted for baseline risk.
“A question this study starts to address is, whether short-term outcomes and complications over the first year are comparable between these two alternative therapies,” Puskas says. “These results suggest that hybrid revascularization is as safe in the first year, with a trend to benefit over the longer term. It would be a challenge to markedly out-perform PCI over the first year. We expect that, if hybrid revascularization has an advantage, it will come out over the next few years.”
He explains that multivessel coronary bypass surgery usually includes a left internal mammary artery (LIMA) graft for the blockage in the left anterior descending coronary artery (LAD), along with veins from the legs for the other blocked vessel(s). The LIMA graft has several advantages: most importantly, the LIMA graft stays open longer than vein grafts, because the LIMA is conditioned to higher blood pressures.
“We know the left internal mammary artery graft is the most durable treatment for that [LAD] blockage, so we expect there will be fewer repeat revascularizations in the hybrid group of patients,” he says.
Hybrid revascularization keeps the LIMA graft for the LAD while using coronary stents for other non-LAD blockages, allowing a minimally invasive approach and avoiding use of the heart-lung machine.
“In light of the growing adoption of this treatment paradigm, a randomized trial of hybrid revascularization is now needed to rigorously evaluate its safety and efficacy relative to PCI,” says Deborah D. Ascheim, MD, associate professor of health evidence & policy and cardiology at the Icahn School of Medicine at Mount Sinai, and principal investigator of the study’s data coordinating center.
Puskas agrees that the results of the current observational study supports investigators' plans to conduct a randomized trial of hybrid revascularization in comparison with PCI.
---
On Saturday at the ACC meeting, multicenter study co-author Michael Halkos, MD, assistant professor of surgery at Emory University School of Medicine, presented data on outcomes following 300 hybrid revascularization procedures performed at Emory starting in 2003.
Summary of results: Of the 300 patients undergoing planned hybrid coronary revascularization, 10 underwent conversion to sternotomy for multivessel coronary bypass surgery. In the remaining 290 patients, hybrid revascularization was performed with surgery first in 228, PCI first in 43 and as a concomitant procedure in 19. For all 300 patients, 30-day mortality, stroke, and non-fatal myocardial infarction occurred in 4, 1, and 6 patients, respectively. Repeat revascularization was required in 10 patients.
Authors' conclusions: Hybrid coronary revascularization represents an alternative approach for patients with multivessel coronary disease with excellent short-term angiographic and clinical outcomes. HCR provides a minimally-invasive alternative to traditional coronary artery bypass surgery and may provide a more durable alternative to multivessel PCI.
