Marianne Swanson remembers well when the diagnosis of HIV was a death sentence. The virus killed most of her young family.
It was 1987, and the wife and mother of two sons was beside herself as her youngest, two-year-old Joshua Paul, grew sicker and sicker. He developed a host of scary and confusing symptoms, including swollen lymph nodes that turned out to be cancerous. Two weeks before he died, he was tested for HIV.
"No kids were being tested for HIV then, but because of my husband’s past and his risk factors, we asked for the test," says Swanson, a nurse, who was pregnant with her third child at the time. (Her husband had told her that he had struggled with his sexuality in the past and had had an affair with a man.)
"Joshua Paul died in July, and in August I got a call from the doctor that he had tested HIV positive and that the whole family needed to be checked," she says.
Those tests brought more devastating news: Swanson and her husband both had HIV. Only three-year-old Jonathan was spared.
Their third child, a girl they named Annalisa, was born with full-blown AIDS, a medically fragile child who spent half of her short life in the hospital. She was 17 months old when she died.
"We tried everything to save her, even enrolled her in a National Institutes of Health study, but she lost her battle with HIV in May 1989, when there was really no therapy for anyone, let alone children," Swanson says.
HIV combination antiretroviral therapy was introduced in the summer of 1996—too late for Swanson’s husband, who died two days before the Olympics opening ceremony in Atlanta.
"I never blamed him, to be honest, because I saw the way he suffered. He saw the two kids die. He did not need the burden of a wife blaming him. He didn’t need me to say it," she told CNN, in a previous article about her experiences.
Swanson, whose life was saved due to the new therapeutic drugs and who now works with HIV patients at Atlanta’s Ponce de Leon Center, decided to speak publicly about her experiences to battle the stigma that can still accompany the disease.
"It’s quite sad but a miraculous kind of story because I survived through all that and I’m living a totally different life now," she says. "I have suffered my losses, but I not only survived, I thrived in the setting of HIV."
It is strange and wondrous to her, even now, to be thinking about aging. "A lot of people who have survived as long as I have remember the time when we were literally dying or waiting to die, and we are now living and aging just like everyone else. Getting older is a good problem to have—I’m overjoyed to be aging," she says.
When her surviving son graduated from high school and enrolled in Georgia Tech, Swanson took a job with the Grady Hospital Infectious Disease Program, at the women’s clinic, then transfered to the main clinic. She first visited Grady Health System’s Ponce Center as a patient. Now a senior staff nurse, Swanson has spent more than a decade talking to HIV-positive men and women about how to live with the disease.
Sometimes she bridges the gap between herself, a 58-year-old Italian woman, and her younger patients, many of them African American men, by sharing her own experience.
"HIV is the great equalizer, no matter your age or background," says Swanson.
Swanson's story continues >>
Aging with HIV: Richard Rhodes
Richard Rhodes: AIDS Activist, Navy veteran, AARP member Richard Rhodes's birthday present to himself the year he turned 65 was an HIV test at AID Atlanta. He'd been getting the test every year on his birthday since the organization was founded some 15 years earlier. This time, he was HIV positive. Now 77, since then Rhodes has been publicly sharing his experiences with HIV and promoting the need for everyone to be tested. |
Emory doctors working on the Frontier
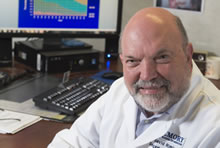
Jeff Lennox, HIV/AIDS researcher "We see patients with heart disease, strokes, thinning of bones, hip fractures, and cancers at a younger age than they would otherwise expect," says HIV researcher Jeff Lennox, professor of medicine at Emory, and associate chair for Grady affairs. More about Lennox's work at Grady Health System's Ponce de Leon Center >> | ||
David Rimland, Chief of infectious diseases at the Atlanta VAMC and Emory professor of medicine. The Atlanta Veterans Affairs Medical Center (VAMC), which serves 1,600 HIV-positive patients, has the largest HIV patient population of any VAMC in the country, and the median age of these patients is 52. |