Live Ebola virus can persist within the eyes for months after a patient recovers from acute Ebola viral disease (EVD), according to a case report published in the New England Journal of Medicine and presented at the ARVO 2015 Annual Meeting in Denver, Colorado (Association for Research in Vision and Ophthalmology).
Despite the presence of Ebola virus within one patient’s eye, samples from his tears and conjunctiva (outer eye membrane) tested negative for virus, indicating that casual contact with Ebola survivors carries no risk.
The finding points to a need for infection control precautions when Ebola virus disease survivors undergo invasive procedures involving the eyes. It also highlights the need for follow-up care for patients who have recovered from Ebola virus disease.
The case report describes a 43-year-old physician who was working in an Ebola treatment unit in Sierra Leone who became infected with Ebola virus. He was transported to the United States and treated at Emory University Hospital’s Serious Communicable Disease Unit for 40 days, including 12 days of mechanical ventilation and 24 days of renal replacement therapy.
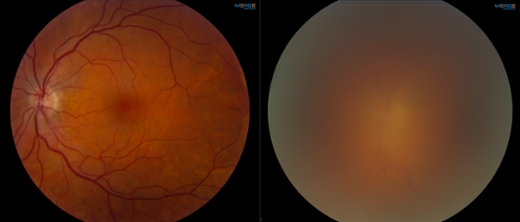
Two months after his discharge from the hospital, the patient was evaluated at the Emory Eye Center following the development of acute anterior uveitis and severe hypertension in one eye.
Uveitis, an inflammation of the middle layer of the eye, can include redness, blurred vision, spots in the visual field, eye pain, headaches, and/or sensitivity to light. Hypertension in the eye can lead to glaucoma.
"The current outbreak has resulted in the largest number of EVD survivors in history. EVD survivors require ongoing medical care to manage complications from the infection that may develop during recovery," says Jay Varkey, MD, assistant professor of medicine (infectious disease) in Emory University School of Medicine.
"Following recovery from Ebola virus disease, patients should be followed for the development of eye symptoms including pain, redness, light sensitivity and blurred vision, which may be signs of uveitis," says Steven Yeh, MD, associate professor of ophthalmology in Emory University School of Medicine.
The patient was treated with topical corticosteroids and medications to decrease the elevated pressure within the eye. Removal of fluid from the eye in a procedure called an ‘anterior chamber paracentesis’ demonstrated live Ebola virus. The virus was found as a result of this invasive procedure.
"To safely evaluate and treat EVD survivors who develop complications in the eye and other ‘immune-privileged’ sites of the body, healthcare providers who perform invasive procedures should develop standard operating protocols for: 1. Safely donning and doffing PPE; 2. Handling laboratory specimens, and 3. Managing medical waste," states Varkey.
The patient has experienced visual recovery following therapy for the uveitis and has ongoing ophthalmic follow-up. These findings have implications for the thousands of Ebola virus disease survivors in West Africa and also for health care providers who have been evacuated to their home countries for ongoing care. Surveillance for the development of eye disease in the post Ebola period is needed.
Despite the presence of Ebola virus within one patient’s eye, samples from his tears and conjunctiva (outer eye membrane) tested negative for virus, indicating that casual contact with Ebola survivors carries no risk.
The finding points to a need for infection control precautions when Ebola virus disease survivors undergo invasive procedures involving the eyes. It also highlights the need for follow-up care for patients who have recovered from Ebola virus disease.
The case report describes a 43-year-old physician who was working in an Ebola treatment unit in Sierra Leone who became infected with Ebola virus. He was transported to the United States and treated at Emory University Hospital’s Serious Communicable Disease Unit for 40 days, including 12 days of mechanical ventilation and 24 days of renal replacement therapy.
Two months after his discharge from the hospital, the patient was evaluated at the Emory Eye Center following the development of acute anterior uveitis and severe hypertension in one eye.
Uveitis, an inflammation of the middle layer of the eye, can include redness, blurred vision, spots in the visual field, eye pain, headaches, and/or sensitivity to light. Hypertension in the eye can lead to glaucoma.
"The current outbreak has resulted in the largest number of EVD survivors in history. EVD survivors require ongoing medical care to manage complications from the infection that may develop during recovery," says Jay Varkey, MD, assistant professor of medicine (infectious disease) in Emory University School of Medicine.
"Following recovery from Ebola virus disease, patients should be followed for the development of eye symptoms including pain, redness, light sensitivity and blurred vision, which may be signs of uveitis," says Steven Yeh, MD, associate professor of ophthalmology in Emory University School of Medicine.
The patient was treated with topical corticosteroids and medications to decrease the elevated pressure within the eye. Removal of fluid from the eye in a procedure called an ‘anterior chamber paracentesis’ demonstrated live Ebola virus. The virus was found as a result of this invasive procedure.
"To safely evaluate and treat EVD survivors who develop complications in the eye and other ‘immune-privileged’ sites of the body, healthcare providers who perform invasive procedures should develop standard operating protocols for: 1. Safely donning and doffing PPE; 2. Handling laboratory specimens, and 3. Managing medical waste," states Varkey.
The patient has experienced visual recovery following therapy for the uveitis and has ongoing ophthalmic follow-up. These findings have implications for the thousands of Ebola virus disease survivors in West Africa and also for health care providers who have been evacuated to their home countries for ongoing care. Surveillance for the development of eye disease in the post Ebola period is needed.