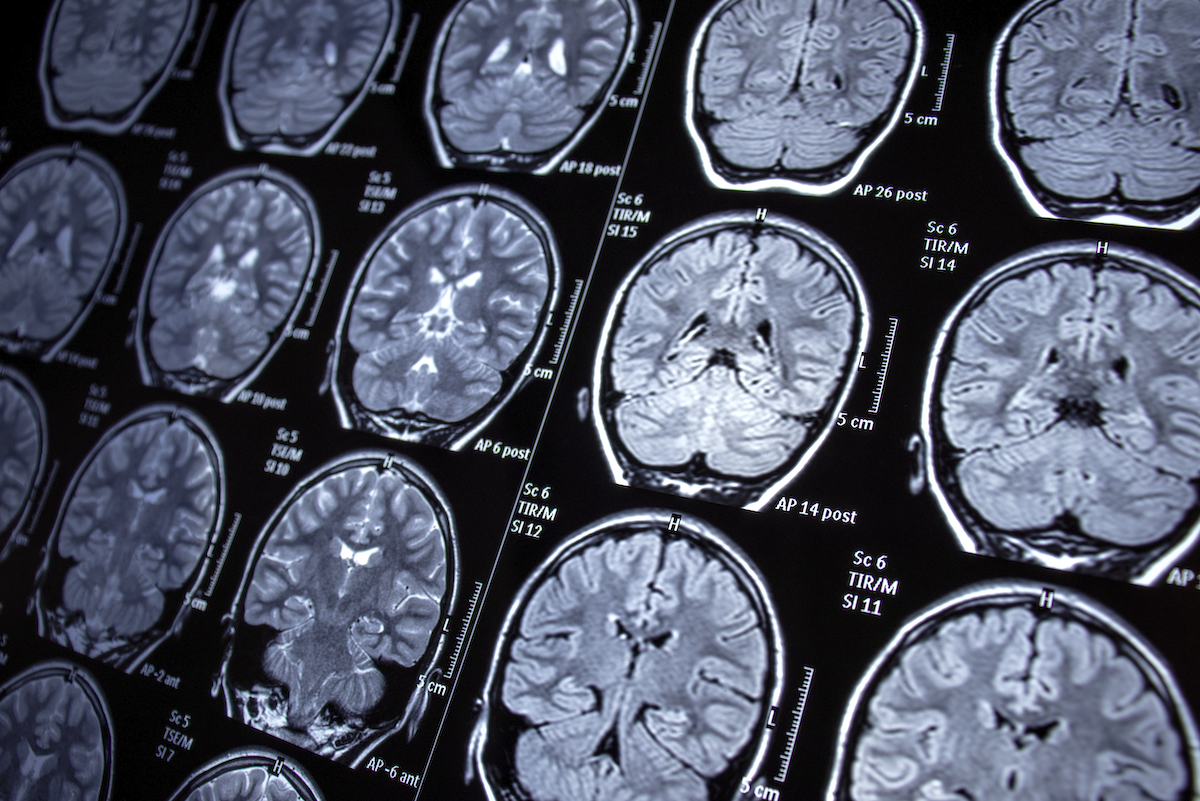
Epilepsy is a persistent brain disorder that produces hard to control seizures and cognitive impariments in 1.2% of the U.S. population. It can be treated and sometimes controlled but never cured. Now, Emory University researchers have discovered genetic pathways to address the stubbornly difficult challenge of alleviating epileptic seizures.
The researchers were part of a multi-institution team studying the chemical pathways that control entire networks of genes in mice to find patterns of gene activation associated with epileptic attacks. Armed with this knowledge, they used the existing drug tofacitinib to suppress seizures in the mice for weeks at a time.
Prof. Nicholas Varvel
Varvel adds that many brain situations, such as head injuries and brain tumors, can switch a normal brain to a brain subject to seizures. Processes like inflammation and neuronal death are known to be part of the process too, but it’s been unclear which ones, singly or together, eventually result in the development of an epileptic brain.
Searching for patterns of genetic control
Looking for answers, the team examined more than 6,000 genes that were active in epileptic mice, then used a custom-built program called MAGIC (Mining Algorithm for Genetic Controllers) to determine the transcriptional signaling pathways—the chemical processes that turn genes off and on, that were most frequently associated with epilepsy.
“We wanted to do mass data mining and ask which signaling mechanisms are engaged after the initial seizure,” Varvel says. “With the rationale that one of these was responsible for the development of epilepsy.”
The team found certain clusters of genes were repressed after epileptic attacks while other groups increased their expression. The group that stood out was switched on by one set of genetic signaling proteins that were later repressed by a different protein. Then they got a surprise.
“The real peculiar thing here was that this pathway was engaged after the initial seizure,” Varvel says. “And then it was re-engaged in the time when the brain had epilepsy. So it seems there's a sort of two-fold engagement.”
Using an existing drug for treatment
The researchers turned to tofacitinib, an existing drug formulated to inhibit the JAK/STAT gene activation process as a treatment for rheumatoid arthritis. When they administered the drug to epileptic mice, the first wave of epileptic attacks continued. Unexpectedly, though, they found that using the same drug to target the second wave of attacks produced strong results: an 80% reduction in severity and frequency of seizures. Eight out of 10 mice were seizure free a month after they stopped administering the drug. There was also a strong cognitive improvement. Varvel says these results work differently from most epilepsy drugs which treat only symptoms.
“With some fairly intricate experimental design,” Varvel says, “we were able to show that if you remove the drug for up to two months for the seizures and for up to two weeks for the behavioral impairments, you remain disease free.”
Seeking to confirm the drug’s performance, the team repeated their experiments in other labs around the country, with similarly strong results. They still don’t know the exact biochemical process at the cellular level that enables the drug to block seizures, but plan to study that as the next step. In the near term, Varvel believes tofacitinib may have an easier path to clinical applications in humans because it’s already on the market for rheumatoid arthritis. Before clinical trials, he wants to study a human population already using tofacitinib to see if they exhibit a lower incidence of epilepsy.
“This is a drug that has already been on the market for many years,” he says. “You can perform a retrospective epidemiological study for people taking tofacitinib for rheumatoid arthritis by asking, what is the incidence of epilepsy in that population? Is it suppressed more so than in the general population? That would provide some evidence that it could be working in humans in the same fashion.”
Varvel believes a positive result from that study could provide a path to clinical tests on people. “Anytime you already have a drug that is FDA approved, it's an easier road to start looking at this in humans,” he says. “One third of individuals with epilepsy aren’t treatable with current drugs. The next step would be to initiate a clinical trial where you have individuals with epilepsy, but they're not responsive to the available drugs, to ask this exact question.”