In a paper published August 9 in Cell Reports Medicine, Todd E. Golde and Yona Levites explain how the amyloid beta deposits long known to build up in the brains of Alzheimer’s patients serve as a kind of scaffold for the accumulation of other proteins. Because many of these proteins have known signaling functions, their presence around the amyloid accumulations, known as plaques, could be the culprit causing brain cell damage rather than the amyloid itself.
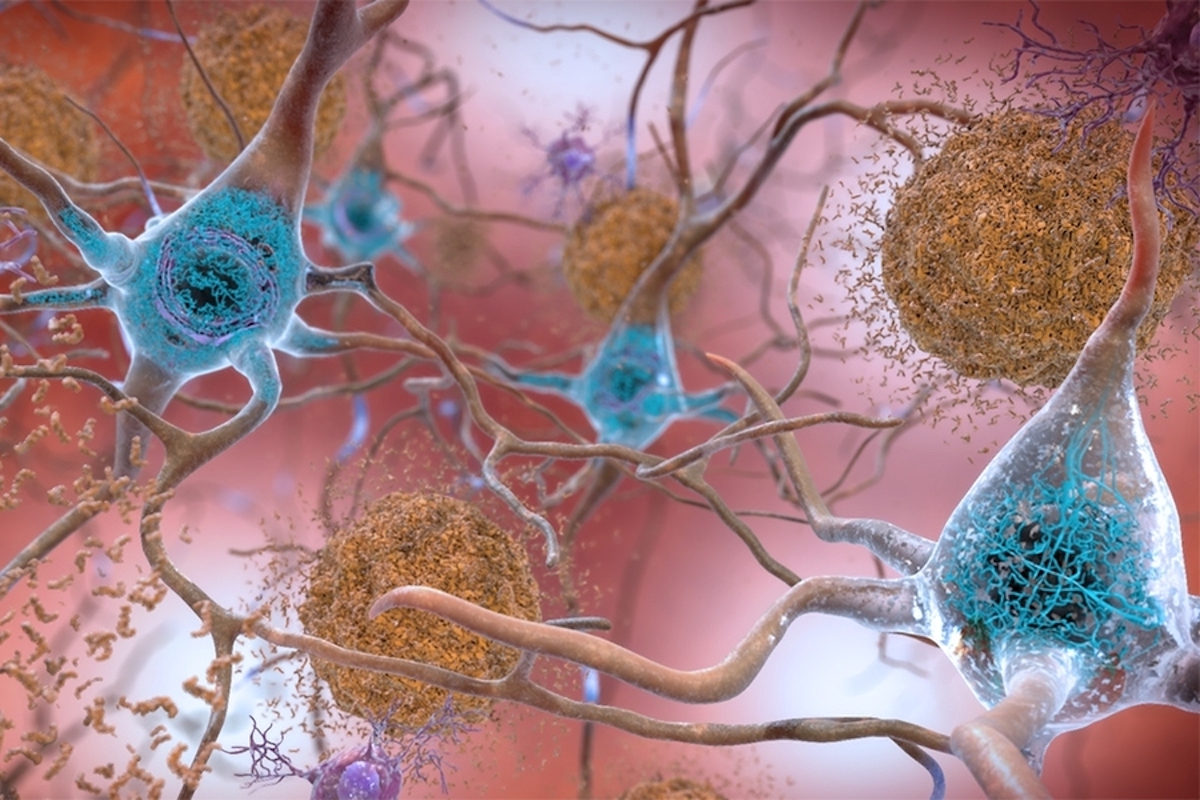
In the brains of those who suffer from Alzheimer’s, amyloids accumulate and build up into sticky plaque that disrupts brain functions and causes cognitive decline. The big unknown has been exactly how that occurs. According to the most widely adopted hypothesis, the amyloid beta buildup disrupts cell-to-cell communication and activates immune cells in a process that eventually destroys brain cells.
In the study, Golde, director of the Emory Center for Neurodegenerative Disease in the Goizueta Institute, Levites, associate professor in Emory University’s School of Medicine, and their colleagues presented a new hypothesis, emphasizing a different role for amyloid beta, a simple protein that forms in all brains but normally dissolves out by natural processes. In experiments, they used cutting-edge analytical technologies to identify and measure the level of more than 8,000 proteins in human brains with Alzheimer’s, as well as similar proteins in mice. Focusing on proteins whose levels increased most dramatically, they identified more than 20 proteins that co-accumulate with amyloid beta in both the human brains with Alzheimer’s and the mice. As the research continues, they suspect they’ll find more.
What the researchers say
“Once we identified these new proteins, we wanted to know whether they were merely markers of Alzheimer’s or if they could actually alter the disease’s deadly pathology,” says Golde. “To answer that, we focused on two proteins, midkine and pleiotrophin. Our research showed they accelerated amyloid aggregation both in the test tube and in mice. In other words, these additional proteins may play an important role in the process that leads to brain damage rather than the amyloid itself. This suggests they might be a basis for new therapies for this terrible brain affliction that’s been frustratingly resistant to treatment over the years.”Why it matters
While the basics of Alzheimer’s have been understood for more than a century, the search for a cure has been slow, often marked by repeated cycles of initially promising treatments that didn’t work in trials, as well as continuing controversy over competing theories to best explain how the disease damages the brain. As the researchers put it, “The initial notion of a purely linear amyloid cascade is now recognized as simplistic. Studies have unveiled the vast complexity of changes occurring over decades in the brains of individuals as Alzheimer’s pathologies emerge.”Significantly, multiple kinds of amyloid buildup, besides amyloid beta, have been implicated in more than 30 human disorders affecting tissues and organs throughout the body. Because this new research proposes a novel process by which Alzheimer’s develops, it may allow for fresh approaches to discovering treatment targets for other diseases as well.
Citation: Levites et al. (2024). Integrative proteomics identifies a conserved Aβ amyloid responsome, novel plaque proteins, and pathology modifiers in Alzheimer’s disease. Cell Reports Medicine 5, 101669.
DOI: https://doi.org/10.1016/j.xcrm.2024.101669
Funding: This research was supported in part by the National Institutes of Health.