A novel technique to test platelet function within a person’s blood sample is faster, easier and more precise than methods currently in use, an experimental study shows.
Nature Biomedical Engineering published the research, led by scientists at Emory University.
The researchers demonstrated the proof-of-concept for the technique, which provides the first detailed look at the molecular forces generated by activated platelets in patient blood samples.
The study results show that the technology holds the potential to assess the effects of antiplatelet drugs on individuals and to gain a clearer picture of bleeding risks for patients undergoing cardiopulmonary bypass surgery.
The technique requires only about a drop of blood to run tests, compared to the tablespoon needed for current assays. This ultrasensitivity may make the technology a valuable tool for the diagnosis of babies suffering from rare, congenital platelet disorders.
The breakthrough is based on synthetic-DNA tension probes developed more than a decade ago in the laboratory of Khalid Salaita, professor in Emory’s Department of Chemistry and in the Wallace H. Coulter Department of Biomedical Engineering at Emory and Georgia Tech.
‘A scientist’s dream’
The tension probes can detect cellular forces on the magnitude of just a few piconewtons, or about a billion times less than the weight of a paper clip. The researchers found a way to amplify the signal of the probes by tapping the power of an enzyme known as CRISPR-associated 12a. The mechanical signal is then detected using a plate-reader, a tool already routinely used in clinical testing.
“This project started out of basic curiosity,” says Salaita, co-corresponding author. “We wanted to know whether we could measure the tiniest forces exerted by cells. It’s exciting that we are now building on this basic curiosity to develop diagnostic tools to help patients. It’s a scientist’s dream.”
First author of the paper is Yuxin Duan, an American Heart Association postdoctoral fellow in the Salaita lab.
Roman Sniecinski, a professor in Emory School of Medicine’s Department of Anesthesiology and a leading expert in the field of perioperative coagulation, is co-corresponding author of the paper.
“Platelet function in general is important and yet the current tools that we have to measure it are relatively primitive,” Sniecinski says. “This new technique offers an easier, faster and cheaper way to measure platelet function, while also providing us with key information that we didn’t have before.”
Co-authors include: Fania Szlam, a senior associate in the Sniecinski lab; Yuesong Hu, a graduate student in the Salaita lab; Renhao Li, a professor in Emory School of Medicine’s Department of Pediatrics, Hematology/Oncology; Wenchun Chen, a postdoctoral fellow in Emory School of Medicine; and Yonggang Ke, an associate professor in the Coulter Department of Biomedical Engineering at Emory and Georgia Tech.
The importance of platelets
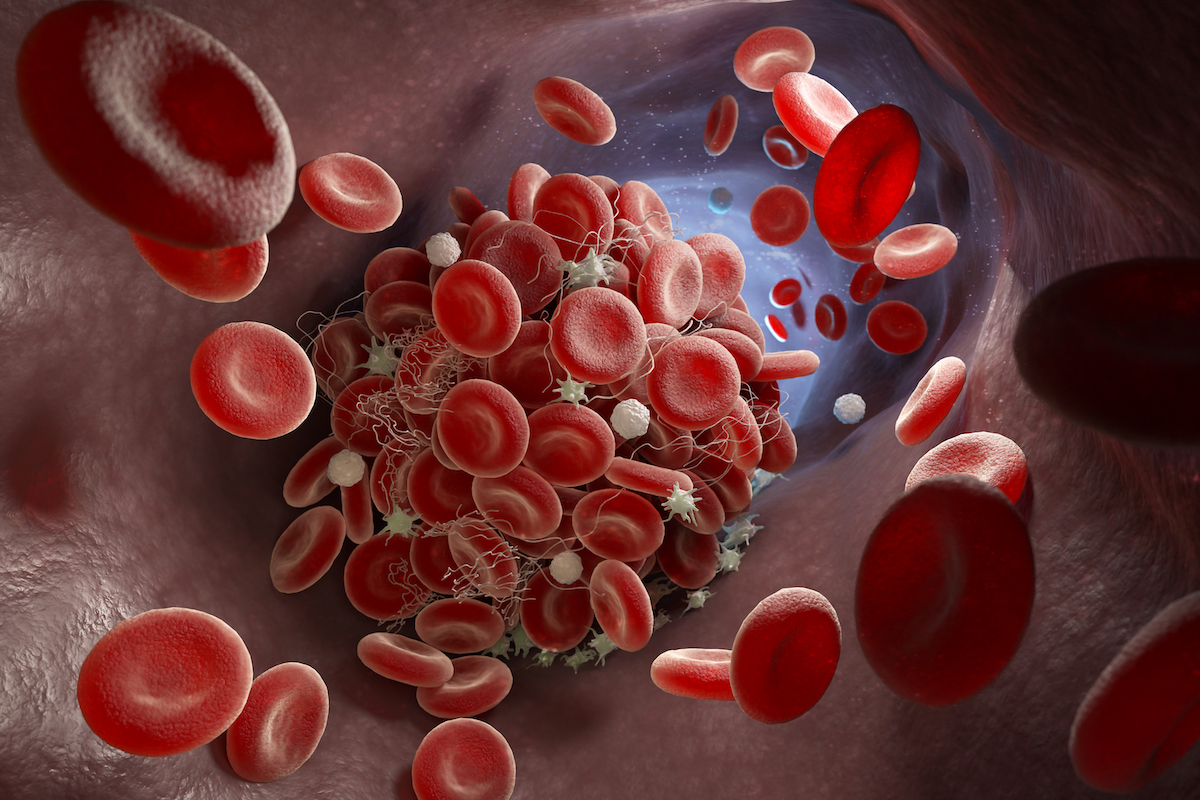
Platelets are colorless, disc-shaped blood-cell fragments whose job is to bind at the site of an injured blood vessel to stop the bleeding. In some cases, however, platelets may not function optimally. When platelets are weak, or less active than optimal, the blood may not clot properly, leading to uncontrolled bleeding. But if platelets are “hyperactive” they may become too sticky and cause spontaneous blood clots that can lead to heart attack or stroke.
Regulating platelet function is especially critical to people at higher risk for some conditions. Antiplatelet drugs, such as clopidogrel, ticagrelor and even aspirin, are among the most commonly prescribed medications in the United States. In some patients, however, these drugs may not work well and adjustments in doses or changing to another drug might better help prevent heart attacks.
During cardiac surgery, platelet function becomes even more dysregulated. The operating-room team must perform a balancing act of making blood not clot during cardiopulmonary bypass, then using procoagulant interventions, including transfusions of platelets, to stop the bleeding when the surgical procedure is finished. This can be difficult because the use of the cardiopulmonary bypass machine can stress and weaken blood platelets.
“For decades, people have written in the scientific literature about this problem of platelet dysfunction during cardiac surgery,” Sniecinski says, “but it’s really difficult to measure it with the tools that we’ve been using. And since we haven’t been able to measure platelet function well, that’s made it difficult to study it in effective ways.”
‘A small part of the picture’
Aggregometry is a standard tool currently used to assess platelet function. It measures the speed and degree at which platelets in a blood sample clump together, or aggregate.
“This data provides only a small part of the picture of platelet function and it’s not the most interesting part,” Sniecinski says.
When a platelet gets activated, he explains, it changes its morphology and grows tiny pseudo “arms.” Platelets use these arms to grip onto chains of proteins in the blood called fibrinogen to form clots.
“Aggregometry tells you that platelets are clumping together,” Sniecinski says. “But it doesn’t tell you about their level of activation — the amount of force they’re using to hold on to other coagulation proteins, as well as each other.”
Amplifying the signal
The Salaita lab is a leader in visualizing and measuring the mechanical forces applied by cells using tension probes made from synthetic strands of double-stranded DNA tethered to a surface.
The double-strands of DNA can be programmed to bind to platelet cells. When the cells bind and apply force to the anchored DNA, the DNA splits into two strands, leaving one strand stuck to the surface. The resulting physical tug is converted into a fluorescent signal.
A major challenge to reading this signal, however, is that these physical tugs are faint, fleeting and infrequent. They require a microscope to detect them.
During the COVID-19 pandemic , the enzyme CRISPR 12a, or Cas12a, came to the fore as a diagnostic tool for SARS-CoV-2 virus. Bacteria use Cas12a to defend against phages, or viruses that attack bacteria. The Cas12a enzyme can be loaded with single-stranded “guide” RNA that is programmed to bind to a complementary single-stranded DNA. The enzyme then reacts to the single-stranded DNA by destroying other single-stranded DNA surrounding it.
The Salaita lab decided to combine Cas12a with its tension probes to see if the enzyme would amplify the signal for the mechanical forces exerted by blood platelets. The lab developed what it calls the Mechano-Cas12a Assisted Tension Sensor, or MCATS.
“It worked like gangbusters,” Salaita says.
“Cas12a is quiet and inactive if it doesn’t see its target,” he explains. “But as soon as it sees a specific single-strand DNA, it goes bananas and starts destroying any single-stranded DNA it comes across. This activation generates a massive fluorescence signal output.”
MCATS is precise and ultrasensitive, able to measure cellular traction forces generated by as few as 2,000 platelets within a sample. And the resulting signal is robust enough to measure via a conventional fluorometer — a tool commonly used in routine blood tests.
MCATS also works with a plate reader, an instrument designed to handle dozens of samples simultaneously, for the kind of high-throughput readout needed to conduct research.
Testing its clinical potential
To test the efficacy of MCATS at measuring the activity of platelet function, the researchers drew blood samples from healthy volunteer donors. They first validated that the MCATS response was sensitive to the mechanical forces of platelets.
They next added to the healthy blood samples different antiplatelet drugs, ranging from over-the-counter aspirin to a panel of different prescription medications. The MCATS results showed that the antiplatelet therapies reduced the mechanical activity of platelets by an amount similar to the reduction observed in aggregometry.
The researchers also received permission to take blood samples for investigation from seven patients pre- and post-cardiopulmonary bypass surgery. The results showed that the MCATS readings for the platelet activity of each individual patient’s sample correlated to their likelihood to need platelet transfusions to minimize bleeding after surgery.
The researchers are now enrolling participants in a prospective study to further explore MCATS as a diagnostic tool. People diagnosed with a platelet disorder will have their blood samples tested pre- and post-treatment to assess how well a therapy is working.
“The bottom line is that MCATS is a whole new way to measure platelet function using a really tiny sample,” Sniecinski says. “It’s telling us something specific that we haven’t been able to measure before and that can give us a new way to understand what’s going on with platelet dysfunction and the best methods for controlling it.”
“Blood work up gives you a basic readout of your health based on data like platelet count and metabolic concentrations,” Salaita adds. “Now we’re adding information about the mechanics of platelets. That’s like getting a whole new dial on your dashboard for monitoring your health.”
Work on the current paper was funded by the National Institutes of Health, the National Science Foundation and the American Heart Association.