Multi-drug resistant microbes—microorganisms that can grow in the presence of many types of antibiotics—are a stubborn, persistent and widespread problem, especially in healthcare settings like hospitals and nursing homes. Difficult to treat under the best of circumstances, they can acquire multiple kinds of resistance to every kind of antibiotic used against them. Sometimes, resistance mechanisms may even accumulate and consolidate within a particular species of bacteria. Worse, they can move from the digestive tract of individuals to the environment, then back to the human gut of new individuals to spread throughout populations.
Even though these individuals may not have symptoms, patients who are colonized with these multi-drug resistant microbes are at higher risk of worse outcomes such as bloodstream infections, sepsis, even death. “Patients who have symptomatic infections are just the tip of the iceberg,” says Michael Woodworth, MD, assistant professor in Emory’s School of Medicine. “Silent transmission is a problem. One person may have no symptoms at all and pass it on to another person who has no symptoms either. This may happen across several people in a chain before someone has a symptomatic infection that is harder to treat with antibiotics.”
The few existing treatments for reducing colonization of multi drug resistant organisms have had only limited effectiveness. Now however, new research from Drs. Woodworth and Colleen Kraft, professor in the Department of Pathology and the School of Medicine’s Division of Infectious Diseases, has managed to reduce multi drug resistant colonization by transplanting microbiota from the stool of healthy donors into kidney transplant recipients, an especially vulnerable population. The study, published recently in Science Translational Medicine, was inspired by earlier findings in 2013 that microbiota transplants managed to reduce a hospital infection associated with a single drug-resistant microbe, C. difficile.
Woodworth says the trial was so effective, “it was stopped early because it wasn’t thought to be ethical to continue to treat patients with antibiotics because the efficacy with fecal microbiota transplant was so much higher.”
Because studies of patients with C. difficile treated with fecal matter transplants have shown reduced colonization of other organisms as well, Woodworth and Kraft wondered whether it might be possible to extend the technique to a wider range of microorganisms. Starting in 2018, the team began taking material from an existing fecal banking program recruited from healthy volunteers, filtering it, suspending it in saline and administering by enema it to kidney transplant patients participating in a clinical trial at Emory University Hospital and the Emory Clinic. All the patients had a history of at least one infection caused by a multi drug resistant organism.
Kidney transplant patients were chosen because they are have had many encounters in the healthcare system, receive more antibiotics and have a higher burden of multi drug resistant organisms. They also stand to lose more because the newest antibiotics used to treat them are often nephrotoxic and could injure their transplanted kidney. One group of patients started with a transplant, then got a second transplant if they were still drug resistant organism positive after 36 days. A second group got a delayed fecal transplant at the 36 day mark if they were still positive after an observation period. As an additional control, Woodworth and Kraft studied infection data in a third group of kidney patients who were eligible for the study but didn’t receive a fecal transplant.
The researchers found the group treated with fecal microbiota transplants had a shorter time to negative stool culture for multidrug resistant organisms compared the control group. At day 36, everyone in the control group was still multi drug resistant organism positive vs only a third of the group treated with fecal microbiota transplants. Eight of the ten participants who received at least one transplant were negative by day 36. Eight out of nine who received all transplants were negative by day 36. The researchers concluded the patients with transplants had more rapid multi drug resistant organism decolonization and longer time to a recurrence of multi drug resistant organization infection.
The investigators got a surprise when they used the powerful tools of metagenomics, letting them study DNA from whole classes of microorganisms at the same time, to see which microbes persisted in their patients after the transplant. In three patients, the investigators found that a resistant strain of bacteria before the transplant was replaced by another strain of the same species after transplant.
Knowing how this happened could be an important step in developing a microbiota-based treatment for antibiotic resistance but investigating it turned out to be a challenge.
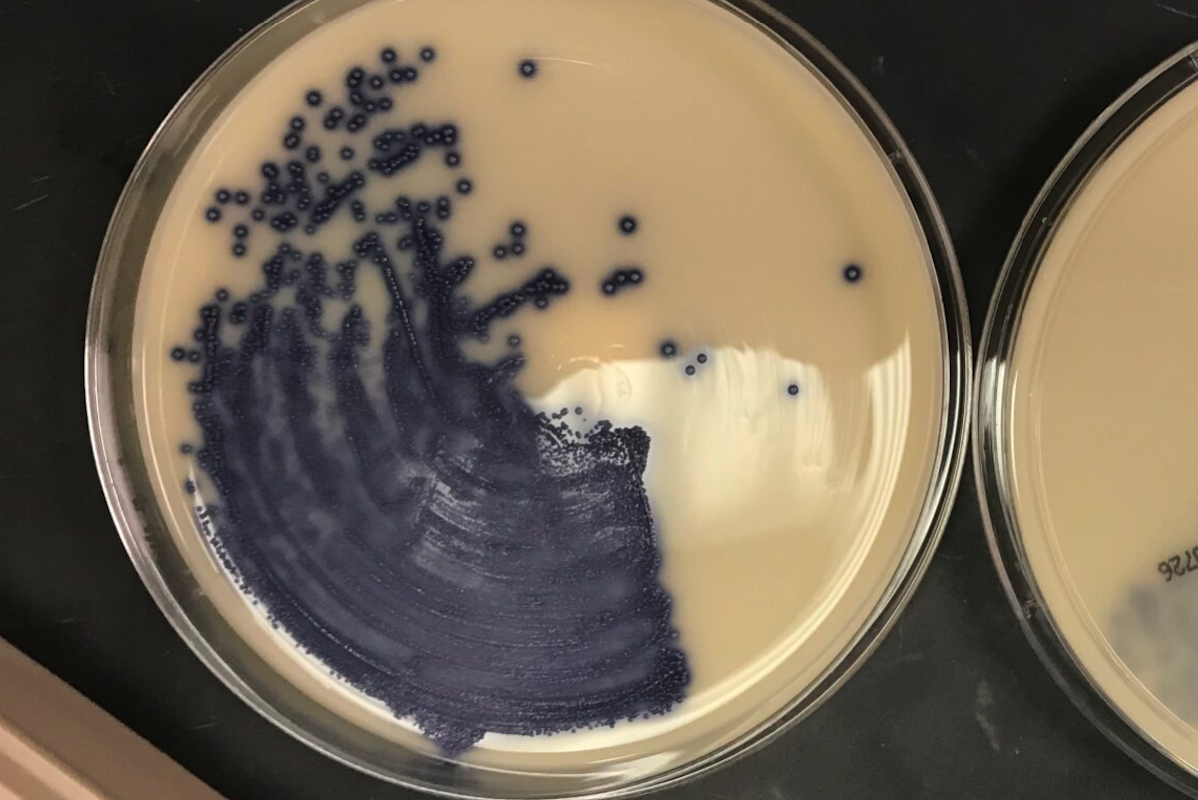
The researchers weren’t sure whether the susceptible strains originated in the patients and expanded after transplant, were introduced by the transplant itself, acquired from the environment, or even represented a genetic change selected by the transplant. They couldn’t find the replacing strains in the transplant material or genetic changes within a single strain that might have led to the loss of drug resistance. Finally, they concluded at least a subset of patients had two strains of E. coli with different levels of resistance to drugs and something about the transplant helped the susceptible strain outcompete the resistant strain. When they plated both strains in vitro on a culture medium, the susceptible strain outcompeted the resistant strain, further evidence that confirmed the metagenomic data that these strains were competing.
Woodworth says his team never expected to discover competition between the resistant and susceptible strains. “It was surprising to us that these bacteria are fighting each other in this way within human hosts,” he says. “And that there are co-occurring strains of different antibiotic susceptibilities that would have totally been missed by other methods.” They are still searching for a more complete explanation for the competitive process, which may exist between different species of microbes or even groups of species as well as between strains of a single species. Ultimately, they hope to develop therapies that are more feasible than the fecal microbiota transplants used in their research.
Two new microbiota therapies against drug resistance were recently approved by the FDA, REBYOTA and VOWST. Studies of these therapies have also suggested they can reduce colonization with antibiotic resistant bacteria but they have only been approved for preventing recurrent infection with a single microbe, C. difficile. Woodworth’s lab is now trying to better understand the strains and genes likely to be most useful for a treatment to reduce colonization with multi drug resistant organisms. “It's important to design these studies to look at not just the resistant bugs, but also the more susceptible ones,” he says. “So we can better understand the microecology of patients that are colonized. The takeaway for me as an infectious disease doctor is hope that we could develop new approaches for these patients who are colonized with antibiotic resistant bacteria beyond isolating them. We hope to help develop something beyond fecal matter transplantation to decolonize patients to prevent infection and transmission.”
Metagenomics refers to deep DNA sequencing of whole communities of microbes. It allows us to understand the composition of these communities without culturing them and also allows us to track closely related strains in these communities over time.