A more contagious coronavirus variant known as B.1.1.7 is still susceptible to antibodies induced after COVID-19 infection or immunization with a currently available vaccine.
Another variant called B.1.351 reduces antibodies' ability to neutralize it. More concerning, but well-armed the immune system may be able to fight off B.1.351.
The variant of the SARS-CoV-2 virus known as B.1.1.7 is still susceptible to antibodies induced after “wild type” COVID-19 infection or immunization with a currently available vaccine.
Yet mutations in another viral variant called B.1.351 reduced -- but did not eliminate – antibodies’ neutralizing and binding activity.
These are the conclusions from two papers published this week by Emory Vaccine Center scientists. The B.1.1.7 report was published in JAMA (Journal of the American Medical Association), and the B.1.351 report was published in Cell Host Microbe.
The Emory researchers’ results are reassuring, with respect to the increasingly prevalent B.1.1.7 variant, which was first identified in the United Kingdom. They mean that people who had COVID-19 early in the pandemic, or have been vaccinated already, will likely not face a handicap against the B.1.1.7 form of the virus.
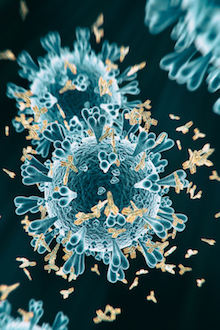
In contrast, the B.1.351 variant -- first identified in South Africa -- contains mutations in the SARS-CoV-2 spike protein predicted to diminish the ability of previous infection- or vaccine-induced antibodies to bind and neutralize the virus. Yet well-armed, the immune system may still be able to fight off B.1.351.
“Against B.1.351, we do see a modest reduction in neutralizing antibody activity,” says Emory virologist Mehul Suthar, PhD, who led or co-led both studies. “Yet the good news is that 8 months out, people who had COVID-19 are still showing decent titers when measured against this emerging variant.”
Overall, the findings highlight the continuing ability of coronaviruses to mutate and escape what the immune system can throw at them. Both variants have been detected in the United States – B.1.1.7 in December 2020, and B.1.351 in January 2021, according to the Centers for Disease Control and Prevention.
The B.1.1.7 variant is thought to be more contagious than the strain of SARS-CoV-2 that initially emerged at the beginning of 2020. A sample – originally isolated from a patient in San Diego -- was provided by the Centers for Disease Control and Prevention.
“The B.1.1.7 variant appears to replicate at higher levels in the respiratory tract,” Suthar says. “One of the mutations – the D614G spike mutation – took over sometime during the summer in many places, because viruses carrying it out-competed others. However, the B.1.1.7 mutations appear not to affect the potency of the neutralizing antibodies we obtained.”
For B.1.351, which is also appearing more in some countries, clinical studies show that some vaccines currently being deployed may not be as effective in preventing infections as against other strains. But the efficacy read-out numbers depend on how prevalent B.1.351 was when and where the study was conducted, says immunologist Jens Wrammert, PhD, who co-led the study on that variant.
“We need to continue to monitor other variants as they emerge,” Wrammert adds. “We don’t know which one is going to take over and be the most problematic.”
The first author of both papers is postdoctoral fellow Venkata Viswanadh Edara, PhD, based in Suthar's lab at Yerkes National Primate Research Center.
In the two papers, some of the antibody samples came from adults who participated in the phase 1 Moderna mRNA-1273 vaccine study in 2020. These samples were provided by the National Institute of Allergy and Infectious Diseases. Another set of antibody samples came from acutely infected COVID-19 patients and people who had recovered from acute COVID-19.
In those naturally infected groups, the neutralizing antibody activity was reduced about four-fold, comparing B.1.351 to B.1. However, the reduction was not as strong for individuals who were more than 3 months past their infections. The paper included antibody samples up to 8 months post-infection.
The sample of B.1.351 variant virus – originally isolated from a patient in South Africa -- was provided by BEI Resources, established by the National Institute of Allergy and Infectious Diseases. The B.1 reference virus was obtained from an Emory Healthcare patient.
To test neutralizing antibodies, researchers in Suthar’s laboratory use a live virus assay, which is considered to more accurately reflect the cellular context of antibodies as they interact with infectious virus in culture. Live virus assays are conducted under Biosafety Level 3 (BSL3) conditions, in contrast with pseudovirus assays, which mix SARS-CoV-2 genes into other viruses, and can be performed more conveniently in the laboratory.
The research was supported by the National Institute of Allergy and Infectious Diseases (U19AI05726617S1 CCHI Immune Memory Supplement, U19AI090023, R01AI127799, R01AI148378, K99AI153736 and UM1AI148684) and Yerkes National Primate Research Center (P51OD011132).
Support also came from Vital Projects/Proteus funds, the Emory Executive Vice President for Health Affairs Synergy Fund, the Pediatric Research Alliance Center for Childhood Infections and Vaccines and Children’s Healthcare of Atlanta, the Oliver S. and Jennie R. Donaldson Charitable Trust and Woodruff Health Sciences Center’s COVID-Catalyst-I3 Funds and 2020 COVID-19 CURE Award.
