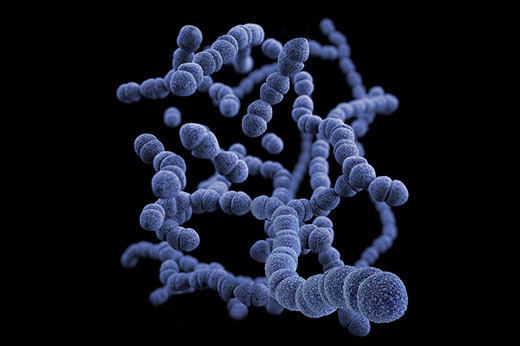
Researchers have mapped the most common bacterial cause of pneumonia around the world and revealed how these bacteria evolve in response to vaccination.
Scientists from Emory University, the Wellcome Sanger Institute and the Centers for Disease Control and Prevention (CDC) worked with many collaborators around the world to carry out a global genomic survey of Streptococcus pneumoniae, discovering 621 distinct strains, or lineages, across more than 50 countries.
Two papers, published in The Lancet Infectious Diseases June 10, and earlier in EBioMedicine, reveal which strains of S. pneumoniae (also known as the pneumococcus) are circulating around the world and explain why pneumococcal pneumonia rates are still high despite the existing vaccines. Funded by a grant from the Bill & Melinda Gates Foundation, this work will help predict which strains will be important for new pneumococcal vaccines, and shows that ongoing global genomic surveillance is vital.
Pneumonia is an infection of the lungs that is responsible for the deaths of hundreds of thousands of people a year globally and is the single largest infectious cause of death of children under 5 years old worldwide. Streptococcus pneumoniae is the most common cause of bacterial pneumonia. Healthy people often carry these bacteria without becoming ill, but they can cause fatal infection, especially in young children and some adults.
Many countries around the world have introduced the pneumococcal conjugate vaccine (PCV) over the last ten years. This vaccine, which targets the coat around each S. pneumoniae bacterium, has greatly reduced the number of childhood infections. However, while PCV is highly effective against up to 13 important coat types (known as capsular serotypes), there are over a hundred types known, and despite the vaccine, pneumococcal pneumonia rates remain very high.
To understand and help combat this infection, researchers set up the Global Pneumococcal Sequencing project (GPS) to carry out genomic surveillance of S. pneumoniae worldwide. Working with partners around the world, the researchers sequenced the DNA of over 20,000 S. pneumoniae samples from infected people from 51 countries.
Robert Breiman, MD, director of the Emory Global Health Institute and principal investigator for the project, says, “GPS turns a spotlight onto a new era in which the intersection of genomics and public health enables unparalleled capacity for optimizing prevention strategies, while providing an immensely valuable tool for forecasting and addressing new challenges ahead.”
Samples were collected both before and after PCV introduction, and the DNA sequences and health data were compared. This makes it possible to determine changes in the bacteria that could affect how well the vaccine protects against the pneumococcus, and whether new strains are emerging that would impact disease severity and ease of treatment.
The researchers discovered 621 genetic strains globally, each associated with one or more coat types. They also saw that the levels of non-vaccine type bacteria rose after the introduction of PCV, showing how bacteria evolve in response to the vaccine.
The pneumococcus can cause disease in other areas of the body too, for example infecting the brain or blood, causing meningitis or bloodstream infections, which can all lead to sepsis. Infant vaccination with PCV protects against these pneumococcal infections too. By reducing the transmission of S. pneumoniae between children, PCV also reduces the number of adult infections through herd immunity.