Emory microbiologists have detected heteroresistance to colistin, a last-resort antibiotic, in already highly resistant Klebsiella pneumoniae, a bacterium that causes blood, soft tissue and urinary tract infections.
The results are published online in the journal mBio.
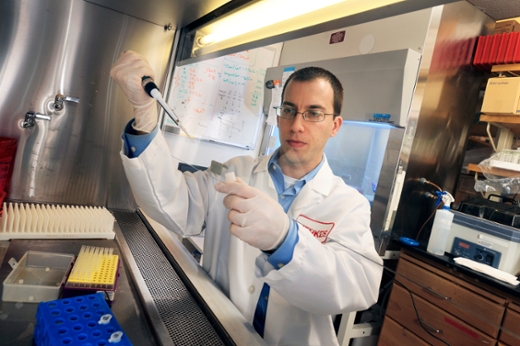
David Weiss, PhD, director of the Emory Antibiotic Resistance Center and a researcher at the Yerkes National Primate Research Center, and his colleagues previously observed heteroresistance to colistin in other bacteria, called Enterobacter. In 2013, the Centers for Disease Control and Prevention (CDC) listed Carbapenem-resistant Enterobacteriaceae (CRE), which include Klebsiella, as one of the top three urgent antibiotic resistant threats. Various types of Klebsiella are estimated to be responsible for 10 percent of infections acquired in health care facilities.
“This is concerning because Klebsiella is a more common cause of infection than Enterobacter, and these isolates were carbapenem-resistant, which means that they might actually be treated with colistin,” says Weiss, professor of medicine at Emory University School of Medicine and Emory Vaccine Center. “To our knowledge, this type of heteroresistant Klebsiella has not been observed in the United States before.”
The first author of the paper is Immunology and Molecular Pathogenesis graduate student Victor Band. Co-authors include Sarah Satola, PhD, Eileen Burd, PhD, Monica Farley, MD and Jesse Jacob, MD. Burd is director of clinical microbiology lab at Emory University Hospital and Farley is director of the Department of Medicine’s Division of Infectious Diseases.
The bacterial isolates came from urine samples from two patients in Atlanta-area hospitals as part of the nationwide Multi-site Gram-Negative Surveillance Initiative, part of the CDC-funded Emerging Infections Program.
Heteroresistance means that bacterial resistance to particular antibiotics is harder to monitor. Heteroresistance is caused by a minor subpopulation of resistant bacteria which are genetically identical to the rest of the susceptible bacteria.
The bacterial isolates described in the mBio paper were not detectable with current diagnostic tests, although it was possible to see them by waiting an extra 24 hours for the resistant population to grow out. It appears that maintaining colistin resistance all the time is disadvantageous for bacteria. Probing the mechanism of heteroresistance, Weiss and his colleagues were able to see a signature of colistin resistance, in terms of genes turned on and off.
In a mouse model of peritonitis (body cavity infection), infection with the heteroresistant isolates was lethal and untreatable by colistin. Colistin is viewed as a last resort measure for bacterial infections that are resistant to other drugs, partly because it is poisonous to the kidneys.
“Clinical laboratories should consider testing for heteroresistance to colistin if this last-line antibiotic is required for treatment,” the authors say. “However, the extra time required is a downside. Novel diagnostics that rapidly and accurately detect colistin heteroresistance are needed.”
The research was supported by the Burroughs Wellcome Fund, the Department of Veterans Affairs (I01BX002788) and the NIH Director's Office of Research Infrastructure Programs (P51 OD011132: primate centers).