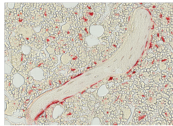
Red staining shows the increased turnover of bone in female mice deprived of sex steroids, an effect that is microbe-dependent. Photo courtesy of Jau-Yi Li.
Probiotic supplements protected female mice from the loss of bone density that occurs after having their ovaries removed, researchers at Emory University School of Medicine and Georgia State University have shown.
The results were published Monday, April 25 in Journal of Clinical Investigation.
In mice, ovary removal induces the hormonal changes that occur with menopause in women. The findings suggest that probiotic bacteria may have potential as an inexpensive treatment for post-menopausal osteoporosis. However, clinical evidence that probiotics can have a lasting effect on the mix of bacteria living in the body is limited.
The immune system was known to be involved in post-menopausal osteoporosis, but the mechanism was previously unclear. Emory and Georgia State researchers found that in mice, the loss of estrogen increases gut permeability, which allows bacterial products to activate immune cells in the intestine. In turn, immune cells release signals that break down bone. Probiotics both tighten up the permeability of the gut and dampen inflammatory signals that drive the immune cells, the team found.
"Our findings highlight the role that intestinal microbes play in modulating gut permeability and inflammation in the context of sex steroid depletion," says senior author Roberto Pacifici, MD. "We think there are direct implications for the treatment of osteoporosis that should be tested clinically."
Researchers led by Pacifici treated female mice twice a week with Lactobacillus rhamnosus GG (LGG), a type of bacteria found in some yogurts, or with a commercially available mix of eight strains of bacteria known as VSL#3. A month after ovary removal, mice that were not treated with probiotic bacteria had lost half of their bone density. But the bone density in probiotic-treated mice stayed the same, the researchers observed.
The type of bacteria was important; treating mice with a laboratory strain of E. coli bacteria lacking probiotic properties did not help, and a mutant LGG bacteria with a defect in sticking to intestinal cells provided a weakened protective effect. In mice that did not have their ovaries removed, probiotic treatment actually led to an increase in bone density.
The scientists also tested the role of gut bacteria in bone loss by studying mice that were raised under germ-free conditions. In this situation, surgical ovary removal is not feasible so the research team used the drug leuprolide, which reduces hormone production by the ovaries. Germ-free mice treated with leuprolide do not have a reduction in bone density.
"What this means is that the presence of some intestinal bacteria is required for sex steroid depletion-induced bone loss," says co-author Rheinallt Jones, PhD, assistant professor of pediatrics. "We observed increased gut permeability following sex steroid depletion. As a result, it is likely that more particles from intestinal bacteria enter the gut tissue and activate immune cells that are known to cause bone loss."
Jones says the team's current investigations are focused on assessing the diversity of the gut microbiome following sex steroid depletion.
"One possibility is that sex steroid deficiency leads to decreased microbiota diversity that exacerbates bone loss, and that probiotics preserve greater diversity," he says.
Pacifici is Garland Herndon professor of medicine and director of the Division of Endocrinology, Metabolism and Lipids in the Department of Medicine at Emory University School of Medicine. The first author of the paper is Jau-Yi Li, PhD, instructor of medicine. Work on germ-free mice was done in collaboration with Benoit Chassaing, PhD and Andrew Gewirtz, PhD at Georgia State University.
This study was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01AR54625, K01AR061453, R01AR059364, R01AR068157), the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK091780, R01DK098391), the National Institute on Aging (R01AG040013) and the Crohn's and Colitis Foundation of America.
