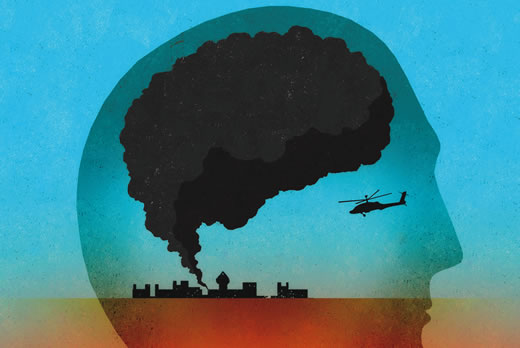
In modern warfare, as in conflicts from eras past, one constant endures: military members are specifically trained not to give in to their emotions.
They tough it out, push through, apply their training, do their jobs. Emotional “weakness” could get them or their comrades killed.
These same traits don’t serve veterans nearly as well after they return home. Keeping terrifying, life-threatening experiences locked away inside and ignoring the fear associated with them can, in fact, magnify their impact.
“People are haunted by these past experiences,” says Barbara Rothbaum, director of Emory’s Trauma and Anxiety Recovery Program and Emory’s Veterans Program. “They may relive them through nightmares, flashbacks, or thinking of them when they don’t want to. They may have problems sleeping, concentrating, or being easily startled.”
If post-traumatic stress disorder (PTSD) is accompanied by physical injuries, especially trauma to the brain, returning to routine day-to-day life and recovering one’s sense of self can be especially challenging. Since the wars in Afghanistan and Iraq started nearly 15 years ago, the Department of Defense reports that of the 2.4 million men and women deployed, more than 52,000 have been physically wounded. The primary injury in these conflicts is blast-related: fiery, eardrum-shattering explosions caused by improvised explosive devices (IEDs), rocket-propelled grenades, and landmines.
But the most common diagnoses for veterans of these modern conflicts involve mental health. Among post-9/11 veterans seeking treatment, an estimated one in three experience PTSD. A little under half are diagnosed with traumatic brain injury (TBI), the signature wound of modern war. For many, PTSD and TBI overlap. (These numbers don’t count veterans who have not entered care or who have dropped out.)
Due to Emory’s longstanding experience treating veterans with mental health issues, especially PTSD, the national Wounded Warrior Project selected Emory Healthcare Veterans Program as one of four founding national centers in a new Warrior Care Network to receive a $15 million grant.
The network connects post-9/11 veterans, regardless of their discharge status, deployment history, or length of service, with individualized care for mental health issues, such as PTSD, PTSD as a result of military sexual trauma, TBIs, anxiety, and depression.
Based on a recent survey by the Wounded Warrior Project, the number of veterans needing such care may be even higher than previously thought. Projections based on survey responses indicate that at least 400,000 service members are suffering from PTSD and another 320,000 from TBIs. The survey of more than 23,000 injured service members—the largest such survey of this generation of veterans—also found that more than one in three veterans had difficulty getting mental health care, put off getting such care, or reported that they did not get the care they needed.
Military sexual trauma, caused by sexual assault, sexual activity against a service member’s will, or repeated sexual harassment, is now common enough that the VA system automatically asks all soldiers if they have experienced it. One in four female soldiers answers yes. Men are less likely to say yes, but those who do—or should have—also may suffer lingering effects, including depression, anxiety, and panic, chronic pain, and gastrointestinal and heart problems. Treatment of PTSD following military sexual trauma is another expertise of Emory’s Veterans Program.

Sheila Rauch
The program launched in September under the auspices of the new, comprehensive Brain Health Center and is ramping up to treat more than 1,000 qualified veterans during the next three years. The staff plans to work with 200 veterans during the first year, 350 the second, and 500 the third. Some of these vets already have been diagnosed with PTSD, TBI, anxiety, or depression and are seeking a second opinion or additional resources. Others have not been diagnosed but describe nightmares, trouble sleeping, angry outbursts, depression, difficulties dealing with their children, anxiety, memory problems, and other symptoms often seen with PTSD or TBI.
“The invisible wounds that our injured warriors struggle with every day have devastating long-term consequences on their health, yet too often they have difficulty seeking and getting timely and effective care for these conditions,” says Jeremy Chwat, chief program officer at the Wounded Warrior Program. “We envision and seek to create a world where warriors who live with PTSD and TBIs have access to the timely and quality care they need to recover, heal, and move forward.”
Veterans for whom Emory’s program has appropriate services are accepted for care. After a comprehensive assessment, an interdisciplinary team of specialists under the direction of Sheila Rauch, clinical director of Emory’s Veterans Program, designs a treatment program personalized to that veteran’s needs. For instance, a veteran whose PTSD is exacerbated by sleep problems may see different therapists from a veteran whose PTSD causes depression, anxiety, or anger. Veterans with TBIs often have cognitive and emotional issues, so treatment is shaped accordingly.