A small section of the envelope protein, located on its “tail”, is necessary for HIV Env to be sorted into viral particles.
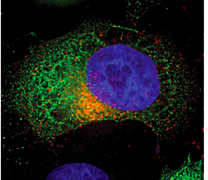
Red is HIV Env, and green is the protein that interacts with its tail, FIP1C. Where they are present together is yellow, and blue is the HeLa cell nucleus.
Virologists at Emory University School of Medicine, Yerkes National Primate Research Center, and Children’s Healthcare of Atlanta have uncovered a critical detail explaining how HIV assembles its infectious yet stealthy clothing.
For HIV to spread from cell to cell, the viral envelope protein needs to become incorporated into viral particles as they emerge from an infected cell. Researchers led by Paul Spearman, MD, have found that a small section of the envelope protein, located on its "tail", is necessary for the protein to be sorted into viral particles.
The results were published June 1 in Proceedings of the National Academy of Sciences.
The finding could explain why the HIV envelope protein has an unusually long tail, an element that distinguishes it from similar viruses. The tail is required for HIV to infect and replicate in the cells it prefers: macrophages and T cells. The long tail is also thought to help HIV avoid the immune system, and figuring out how to manipulate it could help researchers design more effective vaccines.
Spearman is chief research officer for Children's Healthcare of Atlanta and Nahmias-Schinazi Professor and vice chair of research in Emory University School of Medicine’s Department of Pediatrics. Co-author Eric Hunter, PhD is co-director of Emory's Center for AIDS Research and a Georgia Research Alliance Eminent Scholar.
Working with Spearman, postdoctoral fellow Mingli Qi, PhD, and colleagues previously found that a protein from host cells called Rab11-FIP1C is important for the envelope protein to become part of viral particles in the cells HIV prefers.
"The new paper shows that the protein we found is the key factor in determining envelope incorporation in T cells and macrophages," Spearman says. "Now we know the part of the envelope protein required, which is probably the part that binds to Rab11-FIP1C, and have more evidence that this pathway is really important for the virus."
HIV particles are marked by a relatively sparse level of Env protein, which is thought to help HIV avoid provoking the immune system. It may be possible to either interfere with or enhance HIV envelope incorporation in cells, Spearman says. Enhancing the process could make the vaccines his lab is designing, based on non-infectious virus-like particles, more potent. Conversely, interfering with envelope incorporation could be an antiviral drug target.
The research was supported by the National Institutes of General Medical Sciences (GM111027), and the James B. Pendleton Charitable Trust.
