The CRISPR system has attracted considerable attention for its potential uses in biotechnology, but its roles in bacterial gene regulation are still surprising scientists.
In Francisella bacteria, defects in the CRISPR system lead to increased permeability and vulnerability to antibiotics.
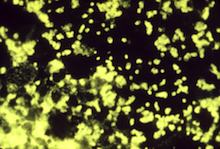
Image credit: CDC
CRISPR, a system of genes that bacteria use to fend off viruses, is involved in promoting antibiotic resistance in Francisella novicida, a close relative of the bacterium that causes tularemia. The finding contrasts with previous observations in other bacteria that the CRISPR system hinders the spread of antibiotic resistance genes.
The results were published Monday in PNAS Early Edition.
The CRISPR system has attracted considerable attention for its potential uses in genetic engineering and biotechnology, but its roles in bacterial gene regulation are still surprising scientists. It was discovered by dairy industry researchers seeking to prevent phages, viruses that infect bacteria, from ruining the cultures used to make cheese and yogurt.
Bacteria incorporate small bits of DNA from phages into their CRISPR region and use that information to fight off the phages by chewing up their DNA. Cas9, an essential part of the CRISPR system, is a DNA-chewing enzyme that has been customized for use in biotechnology.
F. novicida infects rodents and only rarely infects humans, but it is a model for studying the more dangerous F. tularensis, a potential biological weapon. The bacteria infect and replicate inside macrophages, a type of immune cell.
Researchers at the Division of Infectious Diseases of the Emory University School of Medicine and the Emory Vaccine Center were surprised to find that when the gene encoding Cas9 is mutated in F. novicida bacteria, they become more vulnerable to polymyxin B as well as standard antibiotic treatments such as streptomycin and kanamycin. They were able to trace the effects of the mutation back to a defect in “envelope integrity.” Cas9 regulates production of a lipoprotein, which appears to alter membrane permeability.
“The mutant bacteria are more permeable to certain chemicals from the outside,” says David Weiss, PhD, assistant professor of medicine (infectious diseases) at Emory University School of Medicine and Yerkes National Primate Research Center. “That increased permeability also seems to make them more likely to set off alarms when they are infecting mammalian cells.”
Graduate student Timothy Sampson, working with Weiss, found that Cas9 mutant bacteria may be more likely to leak bits of their DNA, a trigger for immune cells to get excited. This is a large reason why Cas9 is necessary for F. novicida to evade the mammalian immune system, a finding published in a 2013 Nature paper.
The regulatory role for Cas9 does not appear to be restricted to F. novicida; Weiss’s team found that a Cas9 mutant in Campylobacter jejuni, a bacterium that is a common cause of human gastroenteritis, also has increased permeability and impaired antibiotic resistance.
The findings add to recent discoveries where Cas9 has been found to be involved in virulence – the ability to cause disease in a living animal or human -- in various pathogenic bacteria such as Campylobacter and Neisseria meningitidis.
Sampson recently completed Emory's Microbiology and Molecular Genetics graduate program and has begun postdoctoral work at Caltech. The research was supported by the National Institute of Allergy and Infectious Diseases grants U54-AI057157 (through the Southeastern Regional Center of Excellence for Emerging Infections and Biodefense), R56-AI87673, R01-AI11070, and the Burroughs Wellcome Fund Investigators in the Pathogenesis of Infectious Disease program.
