An experimental drug called nepicastat shows promise in helping treat cocaine addiction, based on its ability to stave off relapse-like behavior in animals trained to give themselves cocaine. The National Institute on Drug Abuse is beginning a clinical trial testing nepicastat with cocaine-dependent humans this spring.
The animal results were published online this week by the journal Neuropsychopharmacology.
"The main triggers for relapse in humans are stress, the drugs themselves, or exposure to drug-associated cues, like seeing drug paraphernalia or a friend they used to do drugs with," says senior author David Weinshenker, associate professor of human genetics at Emory University School of Medicine. "We can show that nepicastat weakens animals’ drive to return to cocaine-seeking behavior following a period of abstinence, when it is triggered by each of those three situations."
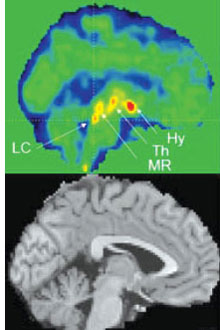
Nepicastat — originally developed for the treatment of heart failure — works by inhibiting the enzyme dopamine beta-hydroxylase and lowering levels of the brain chemical norepinephrine. At the junctions between nerve cells, cocaine increases the levels of both norepinephrine and its relative dopamine by blocking enzymes the brain uses to clear them away. Cocaine addiction research has generally focused more on dopamine, because it plays a large role in the feelings of pleasure produced by natural rewards such as food or sex and is "hijacked" by drugs of abuse.
Norepinephrine similarly has roles in attention, arousal, and stress, but seems particularly important for relapse behavior. Lowering norepinephrine levels does not stop animals from giving themselves a steady stream of cocaine, but it does inhibit their tendency to try to get it after a break or exposure to relapse triggers.

An experimental drug that lowers norepinephrine levels can inhibit relapse-like behaviors in rats trained to give themselves cocaine.
In the new paper, research assistant professor Jason Schroeder, (first author of the paper) conducted experiments where rats are trained to press a lever to get a drug infusion. While the cocaine is being given, a light turns on. Then later after a break, the rats are exposed to the light only.
This is analogous to a human addict, during a period of abstinence, coming to a place where they used to take drugs or meeting a friend with whom they did drugs, Weinshenker says. Nepicastat reduces the number of times a rat will push the lever in an attempt to get cocaine. It also works when this relapse-like behavior is brought on by a small dose of cocaine or yohimbine, a drug that induces anxiety and stress responses in humans.
In a situation where a rat has to press a lever an increasing number of times to get a drug infusion, nepicastat also reduces how hard the rat is willing to "work" to get the cocaine. A rat might normally push a lever up to 75 times to get one infusion of cocaine – but nepicastat will cut that number to 45. However, nepicastat does not prevent rats from working hard to obtain other rewards such as food or sugar.
Recent small-scale studies in humans suggest that nepicastat may make cocaine less enjoyable. In addition, Weinshenker’s laboratory has also recently found that nepicastat makes animals more sensitive to aversive behaviors induced by cocaine, such as repetitive movements that are thought to model psychosis. In fact, humans with low levels of dopamine beta-hydroxylase, the enzyme that is inhibited by nepicastat, are more susceptible to cocaine-induced paranoia.
The research was supported by the National Institute of Drug Abuse (DA027535) and the National Institute of Neurological Disorders and Stroke (NS065663).
Weinshenker is co-inventor on a patent on the use of dopamine beta-hydroxylase inhibitors for the treatment of cocaine dependence. This has been reviewed by Emory in accordance with its conflict of interest policies.
J.P. Schroeder, S.A. Epps, T.W. Grice and D. Weinshenker. The Selective Dopamine β-Hydroxylase Inhibitor Nepicastat Attenuates Multiple Aspects of Cocaine-Seeking Behavior. Neuropsychopharm. (2013) doi: 10.1038/npp.2012.267
