Hypothermia, or lowering the body's temperature, can reduce the damage to the brain after a stroke, but cooling by physical means alone can be difficult to manage.
Scientists at Emory University School of Medicine have shown that a drug that induces hypothermia can decrease the damage to the mouse brain and improve recovery of function after a stroke.
The results, published online March 29, 2012 in the FASEB Journal, suggest that drug-induced hypothermia could be helpful for the clinical treatment of acute stroke.
The senior author of the paper is Shan Ping Yu, MD, PhD, professor and O. Wayne Rollins chair in anesthesiology and pain medicine at Emory University School of Medicine. The first author is postdoctoral fellow Ko-Eun Choi, MD.
Considerable evidence, including data from several clinical trials, indicates that mild to moderate hypothermia can help in stroke treatment. The lower temperature can reduce the needs of neurons for energy, and diminish the levels of toxic chemicals that accumulate in the brain after a stroke.
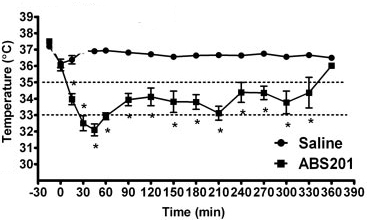
Mild to moderate hypothermia means lowering body temperature to a range between 32–34 °C (90–93 °F). Specialized equipment is currently needed to reduce the body and brain temperature just enough and not too far. Deep hypothermia (a body temperature between 20–25 °C) has several harmful side effects.
Doctors can physically cool a patient's body invasively with a cooling catheter, or non-invasively with vests/leg wraps/caps. Cooling the body in this way requires several hours, when time is essential after a stroke. In addition, the body's responses to cooling, shivering and tighter blood vessels, can interfere with the process of cooling itself.
"Well-controlled temperature is a key factor for successful stroke therapy. The way drug-induced hypothermia works is to lower the 'set point' of the temperature regulating center in the brain," Yu says. "Although this is considered the most efficient way of reducing body and brain temperature, we think this is the first example of applying it to treat ischemic stroke."
Yu's team used a drug called ABS-201 that mimics the effects of the hormone neurotensin to lower body and brain temperature in mice. Neurotensin doesn't last long enough in the bloodstream and doesn't cross the blood-brain barrier. ABS-201, in contrast, can pass through the blood-brain barrier and reduces body and brain temperature in mice below 35°C within 15 minutes, without making them shiver. The same effects can be observed in rats and monkeys without obvious side effects or toxicity, Yu says.
Injecting ABS-201 one hour after blockage of an artery supplying blood to the brain could reduce the area of damaged brain tissue by 30 percent. Mice treated this way also showed an improved ability to sense through their whiskers on the injured side three weeks later. A similar effect was not seen in mice given ABS-201 but kept at normal body temperature, or in mice where only physical cooling was applied.
The researchers recently received NIH funding to explore additional neurotensin derivatives and further test their protective effects and toxicity. ABS-201 and similar chemicals may also have antipsychotic and analgesic effects, which are expected to be "transient and tolerable" in humans, Yu says.
He and his colleagues are currently testing the protective effect of ABS-201 in animal models of hemorrhagic stroke and traumatic brain injury. A potential advantage for drug-induced hypothermia is that it could be applicable to both ischemic stroke (caused by blood clot) and hemorrhagic stroke (bleeding), he says.
"We are planning to examine ABS-201 and other compounds in a stroke model with larger animals," Yu says. "If we can show it to be effective and safe in different animal models, a clinical trial can be expected in a few years."
The team's development of ABS-201 began at Medical University of South Carolina and is in collaboration with Thomas Dix, PhD, associate professor at MUSC and chief scientific officer at Halimed Pharmaceuticals, who holds the patent for the neurotensin derivatives.
The research was supported by the National Institute of Neurological Disorders and Stroke.
Reference: K.E. Choi, C.L. Hall, J.M. Sun, L. Wei, O. Mohamad, T.A. Dix and S.P. Yu. A novel stroke therapy of pharmacologically induced hypothermia after focal cerebral ischemia in mice. FASEB Journal 26, online before print (2012)
Writer: Quinn Eastman