Sequencing a patient’s entire genome to discover the source of his or her disease is not routine – yet. But geneticists are getting close.
A case report, published this week in the American Journal of Human Genetics, shows how researchers can combine a simple blood test with an “executive summary” scan of the genome to diagnose a type of severe metabolic disease.
Researchers at Emory University School of Medicine and Sanford-Burnham Medical Research Institute used “whole-exome sequencing” to find the mutations causing a glycosylation disorder in a boy born in 2004. Mutations in the gene (called DDOST) that is responsible for the boy’s disease had not been previously seen in other cases of glycosylation disorders.
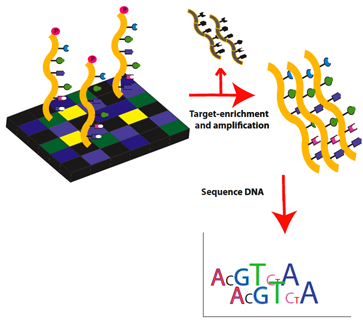
Whole-exome sequencing is a cheaper, faster, but still efficient strategy for reading the parts of the genome scientists believe are the most important for diagnosing disease. The report illustrates how whole-exome sequencing, which was first offered commercially for clinical diagnosis in 2011, is entering medical practice. Emory Genetics Laboratory is now gearing up to start offering whole exome sequencing as a clinical diagnostic service.
It is estimated that most disease-causing mutations (around 85 percent) are found within the regions of the genome that encode proteins, the workhorse machinery of the cell. Whole-exome sequencing reads only the parts of the human genome that encode proteins, leaving the other 99 percent of the genome unread.
The boy in the case report was identified by Hudson Freeze, PhD and his colleagues. Freeze is director of the Genetic Disease Program at Sanford-Burnham Medical Research Institute. A team led by Madhuri Hegde, PhD, associate professor of human genetics at Emory University School of Medicine and director of the Emory Genetics Laboratory, identified the gene responsible. Postdoctoral fellow Melanie Jones is the first author of the paper.
“This is part of an ongoing effort to develop diagnostic strategies for congenital disorders of glycosylation,” Hegde says. “We have a collaboration with Dr. Freeze to identify new mutations.”
Glycosylation is the process of attaching sugar molecules to proteins that appear on the outside of the cell. Defects in glycosylation can be identified through a relatively simple blood test that detects abnormalities in blood proteins. The sugars are important for cells to send signals and stick to each other properly. Patients with inherited defects in glycosylation have a broad spectrum of medical issues, such as developmental delay, digestive and liver problems and blood clotting defects.
The boy in this case report was developmentally delayed and had digestive problems, vision problems, tremors and blood clotting deficiencies. He did not walk until age 3 and cannot use language. The researchers showed that he had inherited a gene deletion from the father and a genetic misspelling from the mother.
"Over the years, we've come to know many families and their kids with glycosylation disorders. Here we can tell them their boy is a true ‘trail-blazer’ for this new disease,” Freeze said. “Their smiles—that’s our bonus checks."
The researchers went on to show that introducing the healthy version of the DDOST gene into the patient’s cells in the laboratory could restore normal protein glycosylation. Thus, restoring normal function by gene therapy is conceivable, if still experimental. However, restoration of normal glycosylation would be extremely difficult to achieve for most of the existing cells in the body.
The research was supported by the National Institutes of Health and by the Rocket Fund.
Reference: M.A. Jones et al. DDOST Mutations Identified by Whole-Exome Sequencing Are Implicated in Congenital Disorders of Glycosylation, online first, Am. J. Hum. Gen (2012). doi:10.1016/j.ajhg.2011.12.024
Originally posted on February 2, 2012