Cancer immunotherapy drugs that block the inhibitory PD-1 pathway have shown success in clinical trials and are now FDA-approved for melanoma, lung cancer and bladder cancer. Yet many patients’ tumors do not respond to these drugs.
Scientists from Emory Vaccine Center have now shown what molecular features distinguish the subset of T cells that wake up when re-energized by PD-1-blocking agents.
The researchers expect that their findings will be valuable for optimizing treatment with PD-1-targeting drugs. The experiments were performed in mice with chronic viral infections, the system in which T cell exhaustion and PD-1’s immune-braking function were first discovered.
The results were published online by Nature on Tuesday, August 2.
PD-1-blocking agents such as nivolumab, pembrolizumab and atezolizumab are part of a class of drugs known as checkpoint inhibitors, and many cancer researchers are now trying to figure out how to enhance their activity by combining them with other types of drugs.
“If we know more about the markers on the T cells that expand after PD-1’s inhibition is removed, that could facilitate the rational design of combination therapies,” says senior author Rafi Ahmed, PhD, director of Emory Vaccine Center and a Georgia Research Alliance Eminent Scholar.
The first author of the Nature paper is postdoctoral fellow Sejin Im, PhD. Collaborators from NIAID (National Institute of Allergy and Infectious Diseases), University of Iowa, Harvard Medical School, Dana Farber Cancer Institute and University of São Paolo, Brazil contributed to the paper.
More than a decade ago, Ahmed and colleagues had shown that the immune systems of mice with chronic viral infections were full of inactive, or “exhausted” antiviral T cells. These cells displayed high levels of PD-1, and antiviral activity could be revived if PD-1’s interactions with its counterpart on other cells (PD-L1) were blocked.
In the current paper, the authors demonstrate that the exhausted antiviral T cells can be divided into two groups. One group undergoes a proliferative burst when virus-infected mice are given PD-1-blocking antibodies, and the other group lacks the capacity to proliferate.
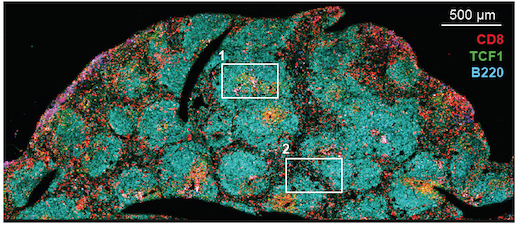
Even before PD-1-blocking antibodies were introduced, the expandable group of virus-specific T cells was dividing at a slow rate. These cells were only in the T cell zones of lymphoid organs (lymph nodes and spleen), not circulating throughout the body. After PD-1 is blocked, these cells divide and differentiate into effector-like cells that migrate to infected tissues.
“If you imagine chronic viral infection – or cancer -- as a war, the expandable T cells are not in the intense part of the battle,” Ahmed says. “But they are somewhat engaged. It’s like they’re waiting in a shelter, ready to respond.”
The researchers also showed that a gene called TCF1 was important for the generation and maintenance of the PD-1-responsive T cells in mice. Inside and outside, the PD-1-responsive cells had molecular characteristics that resembled memory T cells or stem-like cells, while the non-responsive T cells were more terminally differentiated. The authors catalogued several co-stimulatory molecules and receptors present on the surfaces of the PD-1-responsive T cells, which possibly could be targets for drugs.
In collaboration with researchers at Winship Cancer Institute of Emory University, Ahmed’s laboratory is looking for immune cells with similar characteristics in cancer patients. It is possible that this group of revivable T cells may be found in contact with the tumor, or perhaps more likely, in lymph nodes nearby, Ahmed says.
The research was supported by the National Institute of Allergy and Infectious Diseases (R01AI30048, P01AI056299).