In injured mouse intestines, specific types of bacteria step forward to promote healing, scientists have found.
One oxygen-shy type of bacteria that grows in the wound-healing environment, Akkermansia muciniphila, has already attracted attention for its relative scarcity in both animal and human obesity.
The findings emphasize how the intestinal microbiome changes locally in response to injury and even helps repair breaches. The researchers suggest that some of these microbes could be exploited as treatments for conditions such as inflammatory bowel disease.
The results were published in on January 27 in Nature Microbiology. Researchers took samples of DNA from the colon tissue of mice after they underwent colon biopsies. They used DNA sequencing to determine what types of bacteria were present.
“This is a situation resembling recovery after a forest fire,” says Andrew Neish, MD, professor of pathology and laboratory medicine at Emory University School of Medicine. “Once the trees are gone, there is an orderly succession of grasses and shrubs, before the reconstitution of the mature forest. Similarly, in the damaged gut, we see that certain kinds of bacteria bloom, contribute to wound healing, and then later dissipate as the wound repairs.”
The first author of the Nature Microbiology paper is instructor M. Ashfaqul Alam, PhD. Asma Nusrat, MD and colleagues at the University of Michigan contributed to the paper.
In healthy intestines, the microbes in the colon are separated from the cells that line the intestines by a layer of mucus. The biopsy procedure removes that barrier and creates a small wound in the intestine.
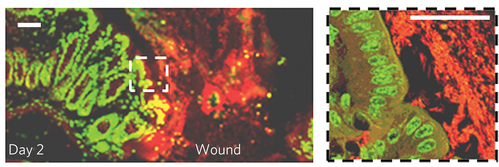
The wound environment is hypoxic, meaning that there is less oxygen than in the surrounding tissue. That encourages the growth of Akkermansia muciniphila and several other types of anaerobic bacteria, which can’t tolerate higher levels of oxygen. The hypoxia appears to be the result of an influx of neutrophils, immune cells that respond to the injury and consume the oxygen.
A robust feedback loop forms, involving the injured microenvironment and Akkermansia, according to Alam. Akkermansia reaches a peak of about 8 percent of the bacteria present. The levels of anaerobic bacteria are increased at two and four days after the biopsy procedure, and then dissipate.
Neish and his colleagues have previously shown that probiotic bacteria, such as those found in yogurt, promote intestinal healing and wound closure by triggering our cells to produce reactive oxygen species. Akkermansia has the same type of effect on intestinal cells, they found. Indeed, the enzymes that produce the reactive oxygen species are necessary to create the hypoxia, which in turn allows Akkermansia to grow.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (RO1DK089763, RO1DK055679), the National Institute of Allergy and Infectious Diseases (RO1AI64462) and the Crohn's and Colitis Foundation of America.