Researchers at Emory University School of Medicine have received a $5 million, five-year grant from the National Heart Lung and Blood Institute to identify and validate new cardiovascular disease risk biomarkers.
Doctors often measure the levels of certain chemicals in the blood, such as cholesterol or glucose, as indicators of risk for conditions such as heart disease or diabetes. Emory researchers want to find similarly easy-to-measure indicators of the health of someone’s blood vessels, which could indicate risk for heart attacks or death. Atherosclerosis, which can lead to heart attacks, is fundamentally an injury to the blood vessels.
“Advanced technology can allow us to detect the levels of many substances in someone’s blood, very quickly and cheaply,” says Dean Jones, PhD, professor of medicine and director of the Emory Clinical Biomarkers Laboratory. “We can see that individuals have distinct metabolic profiles, with patterns that reflect genetics, diet, behavior and environment. Our proposal is to tap this vast amount of information and harness it to help doctors and patients make everyday decisions in cardiovascular medicine.”
Doctors can now estimate the health of blood vessels by non-invasive tests that measure stiffness and the capability of blood vessels to contract and relax. These tests reflect future risk of cardiovascular disease. Testing for presence of coronary artery disease often requires invasive angiography.
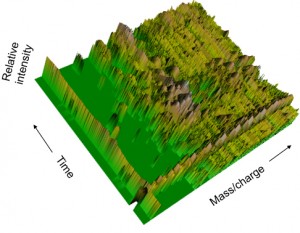
Jones and his colleagues are planning to use metabolomics to sort through thousands of substances in the blood, via mass spectrometry, to find those whose levels match established measures of blood vessel function and coronary artery disease. They think patterns of metabolic markers could be early warning signs of cardiovascular disease.
"Cholesterol and HDL already form part of someone's Framingham risk score, for example,” says Jones. “Where the new biomarker profiles will be important is for people with intermediate risk, who are making decisions like: should I take a statin drug, and which one? And for people with established cardiovascular disease, there is a need to know who will be most likely to benefit from an intervention or medical therapy.”
Jones will team with Arshed Quyyumi, MD, co-director of the Emory Clinical Cardiovascular Research Institute, to study vascular health in and analyze samples from two groups of study participants. Quyyumi's group has already been investigating markers of inflammation and oxidativestress in the context of cardiovascular disease.
One of the groups consists of roughly 900 healthy individuals enrolled in a personalized health program as part of the Emory-Georgia Tech Predictive Health Institute. The second is the Emory Cardiovascular Biobank, which includes more than 4,000 individuals with suspected cardiovascular disease, who are referred for coronary angiography at Emory.
Collaborators for this project include Tianwei Yu, PhD, assistant professor of biostatistics and bioinformatics, and Hanjoong Jo, PhD, Ada Lee and Pete Correll professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University.
To build a model connecting biomarkers with disease risk, Jones, Quyyumi and Yu will track disease progression in both groups of people over the study period. Jo has developed a mouse model of acute atherosclerosis, where alterations in blood flow can lead to blocked arteries within a couple of weeks. In the animal studies, researchers will further probe and validate biomarkers identified in humans.
Emory’s metabolomics study is part of a consortium established by the NHLBI (P20 HL113451) examining altered metabolism and biomarkers in both cardiovascular and lung diseases. The four partnering institutions are Cleveland Clinic, Washington University St. Louis, National Jewish Health and Weill Cornell Medical College. Participating in the consortium will allow researchers to compare results in independent groups of patients.