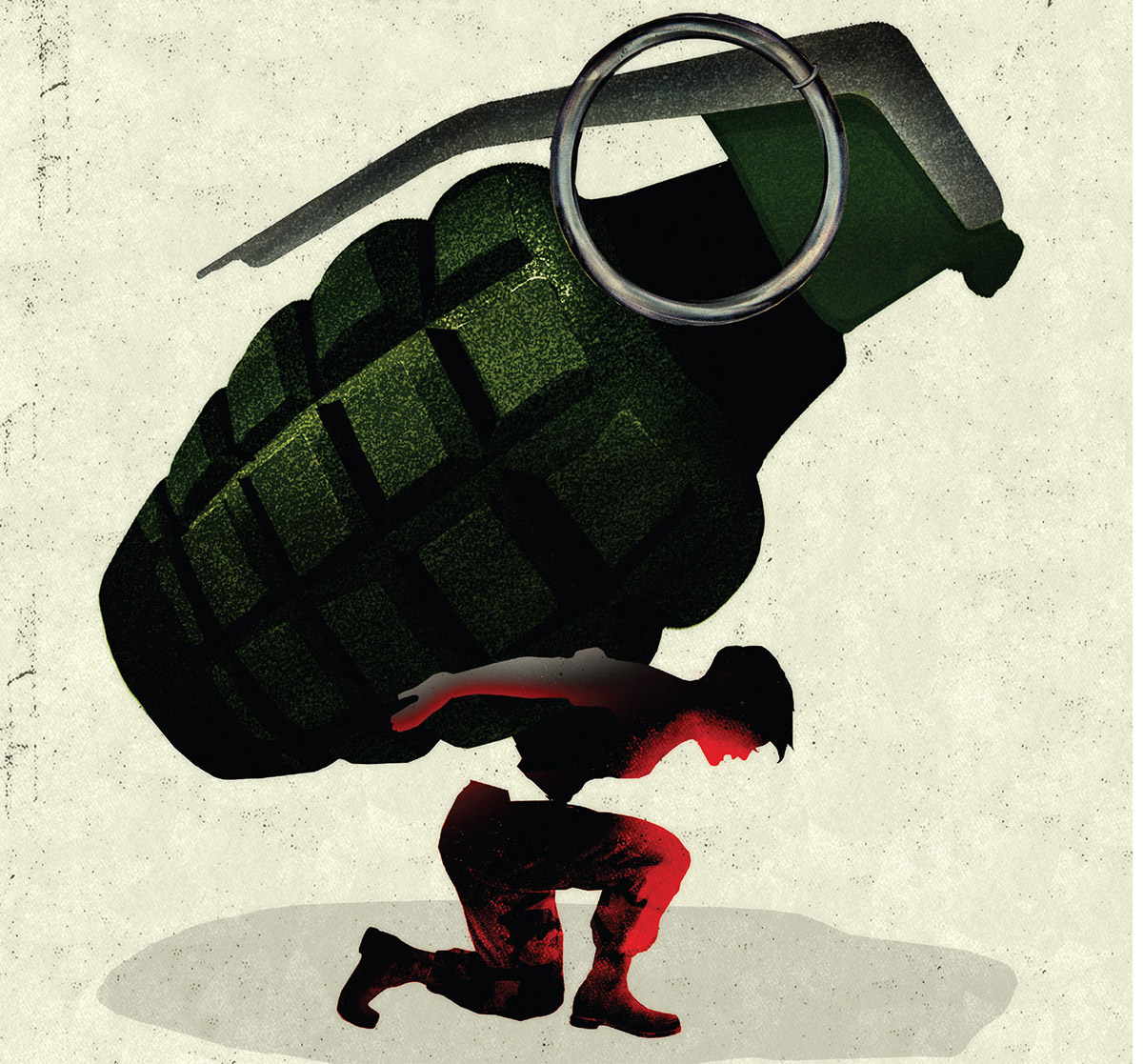
Flashpoint: Healing the invisible wounds of modern warfare

The invisible wounds that injured soldiers struggle with have devastating long-term consequences on their health, yet too often they have difficulty seeking and getting timely and effective care. The Emory Veterans Program aims to change that."
By Sylvia Wrobel, Illustrations by Brian Stauffer
In modern warfare, as in conflicts from eras past, one constant endures: military members are specifically trained not to give in to their emotions.
They tough it out, push through, apply their training, do their jobs. Emotional “weakness” could get them or their comrades killed.
These same traits don't serve veterans nearly as well after they return home. Keeping terrifying, life-threatening experiences locked away inside and ignoring the fear associated with them can, in fact, magnify their impact.
“People are haunted by these past experiences,” says Barbara Rothbaum, director of Emory’s Trauma and Anxiety Recovery Program and Emory’s Veterans Program. “They may relive them through nightmares, flashbacks, or thinking of them when they don’t want to. They may have problems sleeping, concentrating, or being easily startled.”

The Wounded Warrior Project's Warrior Network connects post-9/11 veterans with individualized care. Regardless of discharge status, deployment history, or length of service, wounded veterans can receive free care for post-traumatic stress disorder, traumatic brain injury, military sexual assault, anxiety, and depression. The initiative connects four academic medical centers across the U.S., including Emory, whose Veterans Project is ramping up to treat more than 1,000 qualified veterans over three years.
If post-traumatic stress disorder (PTSD) is accompanied by physical injuries, especially trauma to the brain, returning to routine day-to-day life and recovering one’s sense of self can be especially challenging. Since the wars in Afghanistan and Iraq started nearly 15 years ago, the Department of Defense reports that of the 2.4 million men and women deployed, more than 52,000 have been physically wounded. The primary injury in these conflicts is blast-related: fiery, eardrum-shattering explosions caused by improvised explosive devices (IEDs), rocket-propelled grenades, and landmines.
But the most common diagnoses for veterans of these modern conflicts involve mental health. Among post-9/11 veterans seeking treatment, an estimated one in three experience PTSD. A little under half are diagnosed with traumatic brain injury (TBI), the signature wound of modern war. For many, PTSD and TBI overlap. (These numbers don’t count veterans who have not entered care or who have dropped out.)
Due to Emory’s longstanding experience treating veterans with mental health issues, especially PTSD, the national Wounded Warrior Project selected Emory Healthcare Veterans Program as one of four founding national centers in a new Warrior Care Network to receive a $15 million grant.
The network connects post-9/11 veterans, regardless of their discharge status, deployment history, or length of service, with individualized care for mental health issues, such as PTSD, PTSD as a result of military sexual trauma, TBIs, anxiety, and depression.
Based on a recent survey by the Wounded Warrior Project, the number of veterans needing such care may be even higher than previously thought. Projections based on survey responses indicate that at least 400,000 service members are suffering from PTSD and another 320,000 from TBIs. The survey of more than 23,000 injured service members—the largest such survey of this generation of veterans—also found that more than one in three veterans had difficulty getting mental health care, put off getting such care, or reported that they did not get the care they needed.

The military was the family Meredith never had. She embraced everything about it -- the uniform, the rules, the lingo, hanging out with her comrades. For the first time, she felt like somebody had her back. Pretty ironic, because that feeling was shattered when her commanding officer sexually assaulted her. Go ahead and tell, he said. No one will believe you didn't want it and you'll be dishonorably discharged. She stayed silent, but her performance plummeted. She didn't re-enlist. Back home, she had trouble sleeping, focusing, and trusting anyone, especially men. She didn't date. especially men. She didn't date. She didn't even want to be alone with the manager at the grocery store where she worked part-time, and began to call in sick.
Military sexual trauma, caused by sexual assault, sexual activity against a service member’s will, or repeated sexual harassment, is now common enough that the VA system automatically asks all soldiers if they have experienced it. One in four female soldiers answers yes. Men are less likely to say yes, but those who do—or should have—also may suffer lingering effects, including depression, anxiety, and panic, chronic pain, and gastrointestinal and heart problems. Treatment of PTSD following military sexual trauma is another expertise of Emory’s Veterans Program.
The program launched in September under the auspices of the new, comprehensive Brain Health Center and is ramping up to treat more than 1,000 qualified veterans during the next three years. The staff plans to work with 200 veterans during the first year, 350 the second, and 500 the third. Some of these vets already have been diagnosed with PTSD, TBI, anxiety, or depression and are seeking a second opinion or additional resources. Others have not been diagnosed but describe nightmares, trouble sleeping, angry outbursts, depression, difficulties dealing with their children, anxiety, memory problems, and other symptoms often seen with PTSD or TBI.
“The invisible wounds that our injured warriors struggle with every day have devastating long-term consequences on their health, yet too often they have difficulty seeking and getting timely and effective care for these conditions,” says Jeremy Chwat, chief program officer at the Wounded Warrior Program. “We envision and seek to create a world where warriors who live with PTSD and TBIs have access to the timely and quality care they need to recover, heal, and move forward.”
Veterans for whom Emory’s program has appropriate services are accepted for care. After a comprehensive assessment, an interdisciplinary team of specialists under the direction of Sheila Rauch, clinical director of Emory’s Veterans Program, designs a treatment program personalized to that veteran’s needs. For instance, a veteran whose PTSD is exacerbated by sleep problems may see different therapists from a veteran whose PTSD causes depression, anxiety, or anger. Veterans with TBIs often have cognitive and emotional issues, so treatment is shaped accordingly.
When Louise signed up to serve, she told her parents to please stop worrying about their little princess. At that time, women were not allowed in combat. She didn't tell them that her unit was assigned to drive along roads often laced with landmines or IEDs. Like most traumatic brain injuries suffered by military personnel, Louise's was in the mild range. She doesn't remember the vehicle she was riding in getting hit, only dizziness and blurry vision afterward, then, back home, irritability and depression. Everything seemed harder, slower. Her hands were sometimes shaky and she had a hard time remembering specific words. She wasn't sure what was from her physical injuries and what was from anxiety. She just knew she wasn't the same as before.
Depending on the veteran, treatment may include psychotherapy, pharmacotherapy, cognitive rehabilitation, stress management, or sleep training, offered collaboratively by Emory specialists in psychiatry, psychology, neurology, and rehabilitation medicine.
The Brain Health Center has many of the services veterans need in one place—MRI for diagnostic imaging, gait analysis, a sleep laboratory, cognitive impairment assessment and therapy, rehabilitation, and wellness resources. At this initial stage of the program, all participants live within commuting distance and receive outpatient care once a week or as indicated. In the spring, intensive two-week, full-day sessions will be available for veterans who live farther away.

Clinical Director Sheila Rauch
Both options revolve around the cores of psychiatry, neurology, and wellness and may include yoga, meditation, weight training, smoking cessation, and other activities. Local patients may continue to see Emory therapists; out-of-town patients will be referred for continuing care to providers in their communities, many of whom have received training through Emory’s participation in the Georgia division of Star Behavioral Health Providers.
Within the Warrior Care Network, most veterans will go to the center nearest them: Emory’s Veterans Program in Atlanta, Massachusetts General Hospital in Boston, Rush University Medical Center in Chicago, or UCLA Health in Los Angeles.
Some veterans, however, will be transported to the center with the specific expertise they need. A Georgia patient with disfiguring injuries, for example, may go to UCLA’s Operation Mend Program for reconstructive surgery and counseling. Patients from outside the South may be transported to Emory for its experience with PTSD.
The Warrior Care Network coordinates available resources through the VA. One of Rauch’s jobs, as clinical director and a long-time VA employee, is to design ways that Emory’s Veterans Program can align with the VA, especially the Atlanta VA Medical Center, an Emory partner for nearly 70 years.
“Our veterans have put everything on the line for us and our freedom,” says Rothbaum. “It is an honor and privilege to be able to serve them and their families.”
Clifford Morey remembers the injury that divided his life into before and after.

This fall, former Air Force Staff Sergeant Clifford Morey, his wife, Kelli, son, Kevin, and seizure alert dog, Baz, attended Military Heroes Night at an Atlanta Braves game, an initiative supported by the McCormick Foundation through Emory's Veterans Program.
It was a dark, miserable winter in 2008 in upstate Washington. During survival and escape training, the 24-year-old Air Force staff sergeant climbed over a fallen tree, stepped on a hidden layer of ice, and plummeted 200 feet down a rocky mountainside into a tree, catastrophically dislocating his shoulder and damaging nerves along his left side. After slowly healing, he returned to complete training, and was transferred to Warner Robins Air Force base. But over time the injury took its toll. Eventually he was “medically separated” from the military and the work he loved.
Taking a civilian job in Georgia, Morey tried to ignore the worsening pain and weakness along his left side. He soon required a strong leg brace and cane to walk. In 2013 he had his first seizure, which progressed to up to 50 a week. His doctors were stumped. Finally a local neurologist put his symptoms together with a syndrome he had read about, but had never seen: Complex regional pain syndrome type 2, a progressive, degenerative neuroinflammatory disorder caused by traumatic nerve injury. The nerves misfire, continually sending pain signals to the brain—pain at the top end of the pain scale, sometimes resulting in seizures. The neurologist told him he needed a specialist.
By the time he came to Emory, he was nearly comatose. Neurologists recognized that his symptoms were pain-related and changed his medication, resulting in fewer seizures. Morey, who says he also suffers from related depression and mild traumatic brain injury, believes veterans with mental health issues from training or combat injuries “need all the help we can get. I’m thankful that a program like the Warrior Care Network exists for us.”
Contacts
How post-9/11 veterans can access care
Call 1-888-514-5345 or submit a form online. You do not need to have been diagnosed. If services offered by Emory’s Veterans Program are appropriate for you, you will be asked to come to Emory for a comprehensive assessment. Veterans do not pay any out-of-pocket costs for this assessment, nor for any therapy they and their clinicians decide is appropriate. To be able to care for as many veterans as possible, Emory’s Veterans Program does work with insurance companies to collect payment if available. For veterans without insurance, the Wounded Warrior Project and Emory’s Veterans Program will ensure that these programs are delivered at no cost to the veteran.
How clinicians can provide care in their communities
Complete the three-tier Star Behavioral courses and join the Star Behavioral Health Providers registry used by veterans to find clinicians who understand what they have experienced. Contact Liza Zwiebach at georgiaadmin@starproviders.org or 404-727-8964.







