Coping with Chronic Pain
"It's important to treat pain responsibly, and we're increasingly using more kinds of natural medications."

By Sherry Baker
CHRONIC PAIN can be caused by inflammation, injury, infections, surgery, cancer. But there are times when zeroing in on exactly where the pain is coming from—and what can best be done to relieve it—isn’t obvious or easy.
Patients may find themselves with prescribed medications that leave them feeling dazed or nauseous, unable to drive or work, and with the potential for addiction or abuse. “Our focus is treating pain and function, but in the healthiest way possible so we can get patients back to where they enjoy their life again,” says Anne McKenzie-Brown, director of Emory’s division of pain management and director of the Emory Pain Center at Emory University Hospital Midtown.
Back pain is the most common type reported and it’s the leading cause of disability for people under the age of 45, according to the American Academy of Pain Medicine.
“These patients fall into a couple of categories,” McKenzie-Brown says. “Some may have degeneration of the spine. We also see, in the older population, disc or spinal stenosis, which is a narrowing of the spine. And a lot of patients have lumbar spondylosis—back pain caused by arthritis of the facet joints, or following some kind of injury that doesn’t get better after many months. We also see a lot of patients with back pain that didn’t quite get better after back surgery.”
Other common types of pain include severe discomfort in the middle of the spine that may radiate to the hip from the sacroiliac joint, and radicular pain—back pain that shoots down the leg—known as sciatica.
While neurologists tend to treat vascular and migraine headaches, Emory Pain Center physicians typically treat headache patients whose pain originates from the back of the head and the neck due to occipital neuralgia (nerve pain). Headaches can also arise after accidents from trauma to upper cervical facets—small flexible joints containing nerves that exit the spinal cord on their way to other parts of the body. “People will say they have headaches coming from their necks, and they actually do,” McKenzie-Brown says. “We see headaches combined with neck pain that may radiate to the arm and shoulder too.”
Peripheral neuropathy—nerve damage that can cause weakness, numbness, and pain—can be the result of long-standing diabetes and is becoming more common with the epidemic of type 2 diabetes in the U.S. “There can also be medication-induced neuropathy, especially in people who had cancer treated and are in remission, but are left with some nerve damage,” McKenzie-Brown says.
The Opioid Factor
Once a patient comes to the pain center, the physicians may order tests such as EMGs (a test that records the electrical activity of muscles), MRIs, and others, depending on what is appropriate to make a diagnosis. A personal plan of action is then determined with input from the patient. This may include, but is not limited to, pain medication.
Since opioid addiction and abuse have been declared a national emergency, their use and prescriptions are under increased scrutiny. “Opioids present a double-edged sword,” says Emory pain specialist Boris Spektor, pain fellowship program director and assistant professor of anesthesiology. “They are extremely effective in the short term for acute pain that subsequently resolves, although potential side effects include nausea, sedation, and constipation.” Physicians must ensure that opioids are being taken as directed, are improving function, and are allowing patients to reach their goals, he says. Unfortunately, chronic exposure to opioids often leads to development of tolerance and an increase in dose, with a corresponding increase in risk of side effects. “This can create a downward spiral,” says Spektor. For chronic pain patients who have not been helped by other treatments and are on stable amounts of opioids, it may be necessary to continue this therapy. “But it’s important for them to understand the potential downstream effects,” he says, “which include hormonal changes, immunosuppression, increased risk for fractures, and risk of addiction.”
The majority of pain medications used at the center are non-opioid. “And most of the patients we have on opioids we are weaning to the lowest possible dose,” says McKenzie-Brown, who recently served on a national committee of 18 health experts who produced a report on opioid overuse for the National Academies of Sciences, Engineering, and Medicine. “We found we need to look not only at the way physicians treat pain but also at patients’ expectations in the way their pain is managed.”
- Nearly 50 million adults experience significant chronic or severe pain.
- More than 11% of adults report having had pain every day over the course of three months.
- Low back pain is the most common (27%), followed by severe headache or migraine pain (15%), neck pain (15%), and facial pain (4%).
- Women are more likely to experience pain than men, and twice as likely to experience migraines or severe headaches.
- An estimated 20% of American adults (42 million) report that pain or physical discomfort disrupts their sleep a few nights a week or more.
Reclaiming Life
The center’s team strives to combine improved function with pain relief. “If your activities have been limited by pain, we want you to get back to enjoying your life and be able to go back to work,” McKenzie-Brown says. For most patients, that involves physical therapy (PT). Patients are amazed at how well PT works and how much better it makes them feel, McKenzie-Brown says. “Just seeing that they are able to get up and move and do things is beneficial. The mindset is crucial.”
Emory Pain Center physicians also prescribe topical pain-relieving creams and recommend complementary therapies, such as massage, acupuncture, and yoga when appropriate.
They even try to provide alternatives to nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, Advil, and Motrin, which can have serious side effects if taken regularly. “It’s important to treat pain responsibly, and we’re increasingly using more kinds of natural medications,” McKenzie-Brown says. “For example, especially for patients who have trouble with stomach irritation or kidney infections, I recommend turmeric and tart cherry juice.”
All physicians at the Emory Pain Center are trained interventional pain specialists, and they get together frequently to discuss different kinds of pain and treatment options. The following are some of the most common minimally invasive options:
- Radiofrequency denervation. Also known as radiofrequency ablation, this procedure relieves facet joint pain and pain caused by trauma to the back, such as from a car accident. First, nerves thought to be causing the pain (usually in the neck and lower back) are injected with a tiny amount of numbing anesthetic. If the pain is relieved for hours to days, the patient is considered a good candidate for radiofrequency ablation, which involves zapping the troublesome nerves with pinpointed heat, causing a tiny lesion that “kills” the nerve. In some patients, the nerves regenerate and pain returns in six months to a year. For others, relief can last for years or never return.
- Spinal cord stimulation. A small electrode implanted in the epidural space allows electrical impulses to be sent to the spine, via a control device. The stimulation changes pain signals to a more pleasant feeling, or may block pain entirely. The stimulator is primarily used for neuropathic pain and for a condition known as “failed back surgery syndrome,” which can occur when people have scar tissue or persistent pain in their back and legs after surgery.
- Trigger point injections. This outpatient procedure is used to relieve musculoskeletal and myofascial pain caused by trigger points—small knots in muscles. Depending on the type of pain and the area to be treated, doctors insert a small needle into the patient’s trigger points. The injections, which contain a local anesthetic (such as lidocaine), saline, or steroids, may be repeated as needed. Trigger point injections break the cycle of pain by relaxing the muscle and are most effective when combined with PT.
- Nerve blocks. In this technique, numbing medication is injected in a group of nerves to block pain to a specific body part. For example, sympathetic nerve blocks treat pain that may persist after an injury or surgery, occipital nerve blocks can help headaches originating from the neck, and epidural nerve blocks are used to relieve spinal stenosis pain and herniated disc pain. When the appropriate area is numbed, the extremity gets warmer because the area receives more blood flow, which relieves pain and allows patients to do more PT.
Surgical Options
While treatments and therapies can help, there are times when surgery is necessary.
Emory surgeons and pain center physicians have a close, collaborative relationship. “I look at MRIs and talk with the surgeons and discuss why they are using one approach compared with another,” says McKenzie-Brown. “Sometimes, we send patients for surgical evaluation and the surgeon says, yes, we can perform surgery, but let’s wait six months and try more non-surgical approaches—especially if patients are high risk due to additional health problems.”
On the other hand, if a patient complaining of back pain is experiencing neurologic changes, such as weakness or a sudden lack of coordination with their hands, or difficulty controlling their bladder or bowel, the clinic immediately contacts a surgeon and sends images. “Usually, they will see our patients relatively quickly,” McKenzie-Brown says.
Treating Cancer Pain
Malignancies, especially when advanced, can bring pain in and of themselves. “Pancreatic cancer and metastatic lung, metastatic breast and, in general, any cancer that has spread is more likely to cause pain,” says Vinita Singh, director of cancer pain treatment at the Emory Pain Center and chief quality officer for Emory’s pain division.
The Emory Pain Center has an acute pain service to help patients hospitalized with intense cancer-caused pain. For instance, doctors may perform a celiac plexus block—an injection that blocks nerves transmitting pain signals from the abdomen—to help pancreatic cancer patients decrease their hospital stay and go home with their pain relieved.
When Singh first started in pain medicine, oncologists did not frequently refer patients to her who were just starting treatment. But that’s changed with increased awareness of the clinic and the importance of early pain management. The number of people coming to the Emory Pain Center with cancer-related pain is steadily rising.
In all, about 40 percent of the patients Singh treats have cancer or are cancer survivors still plagued by pain and discomfort. “Cancer doctors are realizing it’s helpful for us to address any cancer-caused pain early on so I can do a multi-modality treatment, instead of waiting until patients are on an opioid mountain that’s difficult to get off of,” she says.
Cancer patients not only have a challenging diagnosis to deal with, they often have so many medical appointments they may forget to come to a pain treatment appointment or are too exhausted to follow through. “That’s one of the biggest challenges,” Singh says. “But when they do come and get treated, cancer patients appreciate the fact that it ultimately makes them feel better. This is an opportunity for them to talk about their pain and their quality of life, and for us to figure out a way to help.”
Screening and treating patients for depression are important parts of ensuring that all aspects of their pain are addressed. “Pain can worsen depression, and depression can worsen pain,” says Vinita Singh, director of cancer pain treatment at the Emory Pain Center. “I always tell my patients that treatments for both must go hand in hand. We cannot treat one and forget the other. Research suggests that some antidepressants may actually help with pain relief.”
Post-treatment Pain
Chemotherapy, radiation, and surgery can all cause lingering pain. Post-mastectomy pain, pain after thoracotomy (surgery involving the chest wall), and chemo-induced peripheral neuropathy are some of the pain problems Singh sees that are not caused by cancer but by its treatments. “Neuropathy can be especially worrisome because it may cause a loss of sensation to feet or hands and lead to falls and an inability to drive,” she says. Fortunately, chemo-caused neuropathy often gets better in a year or so, but not always.
Singh uses non-addictive medications, primarily gabapentin (a drug that treats nerve pain) and topical lidocaine creams to treat patients. If that doesn’t succeed, other options—including radiofrequency ablation—are considered. Singh also frequently recommends physical therapy and complementary therapies, including yoga, tai chi, and acupuncture. “I try to think outside the box, using all the principles of anatomy and anesthesia, seeing how we can get pain relief while minimizing the risk and side effects of opioids,” she says.
Singh, who sees acute pain patients at Emory University Hospital and Emory Hospital Midtown, has established monthly, multi-disciplinary pain board meetings that bring together Emory physicians and specialists in oncology, psychiatry, interventional radiology, and other relevant disciplines to discuss complex cases.
Palliative Care
End-of-life issues for those with terminal diseases include dehydration, loss of appetite, nausea, and pain.
“At that point, I get palliative care specialists involved, if they are not already, along with supportive oncology,” Singh says. While it may seem that opioids are reasonable for those at the end of life, she says the drugs can actually cause additional problems. Not everyone tolerates them well, and opioids can result in severe constipation and leave patients feeling drugged.
Singh and colleagues are currently recruiting patients for a clinical trial of intranasal ketamine. They hope a very small dosage of the anesthetic, administered through the nose without going through the stomach, may offer pain relief with fewer side effects.
For now, there are other options. Singh recalls a patient—a retired surgeon in his 60s—who had Parkinson’s disease, heart failure, and advanced terminal cancer. He could not tolerate opioids and was exhausted from constant pain.
Simply trying to make a breakfast omelet was an ordeal. He’d crack one egg then sit and rest before attempting to crack another. A spinal cord stimulator was implanted, which reduced his pain, allowing him to go to church and on walks. He was able to enjoy his last year as much as possible.
“Even in the most advanced cancer cases,” Singh says, “something can absolutely be done to help relieve a patient’s pain.”
Patient Stories
Targeting the Source

For years, Margaret Freeman went to her information technology job in pain, trying to tough out the aches in her neck, back, and shoulders.
At
Freeman, 51, tried over-the-counter pain relievers, hot and cold packs, and chiropractic treatments. Nothing gave much relief. “I would wake up all the time at night with pain,” she says.
She made excuses when friends invited her out. She even missed a large family gathering honoring her mom on Mother’s Day.
Instead, she was flat on her back at home—alone, sad, and in pain. She finally confided in a co-worker, who told her she needed to see a pain specialist. But she hesitated. “I figured I’d be handed a prescription for some heavy-duty pain reliever I wouldn’t want to take anyway.”
In fact, just the opposite happened. Anne McKenzie- Brown, director of the Emory Pain Center, listened carefully to her symptoms: “She knew the right questions to ask, the right places to touch.” The diagnosis was cervical spondylosis, an arthritic condition from wear and tear affecting the spinal discs in her neck, and lumbar myofascial pain, triggered by sensitive points in her muscles.
Physical therapy helped, but she didn’t have complete relief until after two minimally invasive procedures. “I used radiofrequency denervation and ablated the nerves in specific facet joints,” McKenzie-Brown says, “as well as lumbar trigger point injections with
Freeman checks in at the center if she has symptoms return, but most of the time she feels great, able to jump on a trampoline with her nieces, ride a scooter, and join friends at social events. “The bottom line is this: I got my life back.”
Action Plan

Brenda Jones, 65, loves to be active, going out with friends, making art, and gardening.
These simple pleasures, though, were sometimes too painful to pursue.
When Jones was 17, she had several surgeries for scoliosis, involving nearly her entire spine and resulting in post-operative pain. She has had spinal degenerative disease above and below her surgery sites, chronic nerve pain, rheumatoid and psoriatic arthritis (which causes her immune system to attack her joints), and chronic nerve pain from carpal tunnel syndrome. She’s also had multiple joint replacement surgeries, including her hip and, most recently, her shoulder.
In 1992, she could no longer work. “I’ve been in so much pain I felt delirious at times,” she says. “I could hardly do anything. It was difficult to even think clearly.”
She sought treatment from Emory pain specialist Boris Spektor, who devised a personalized treatment plan. “Brenda was open-minded to combining several treatments to achieve relief,” he says.
First, she discontinued chronic opioid therapy, switching to non-opioid nerve pain medications, topical complementary medications, physical therapy (including competitive table tennis), and injection therapy.
Spektor also performed radiofrequency ablation of the medial branch nerves in her neck and lower back.“This essentially silenced the nerves that were transmitting pain signals from the facet joints,” he says. “She experiences about a year of substantial pain relief from each procedure.“
Jones understands she will never be truly cured. “I’ll need ongoing care and treatment,” she says. “But for six years so far, Dr. Spektor has helped me get back on my feet, literally, and do some of the things I enjoy.”
The Toughest Battle
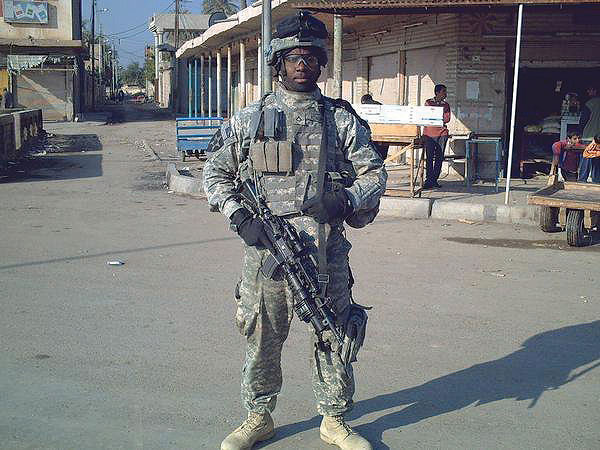
In June 2007, while serving in the Army in Iraq, David Kendrick’s unit received intel that there was going to be an attack on a nearby college. “I had just finished checking a backyard and was walking back to my Humvee when I heard the crack of a rifle,” he says. “I fell to the ground and blacked out from the pain.”
Thanks to quick and courageous action by fellow soldiers, he survived. But his femur had been shattered in three places and his femoral artery was severed. He was in and out of the hospital for 14 surgeries.
During one of his many medical visits, he wondered out loud why he was always trying to find a way to get back into the hospital. “Because you’re addicted to opioids,” a doctor answered.
Yet the prescriptions didn’t stop. Kendrick wasn’t ready to believe the drugs he was taking—Vicodin and morphine—were a problem. After all, he had severe injuries and was in pain, and the drugs helped.
Once he was out of the hospital, he was placed in a Warrior Transition Unit in Colorado Springs for soldiers who needed at least six months of rehabilitation. “We all had some kind of opioids, and we passed them around like candy,” he says. After a friend and fellow vet died from drug use, however, Kendrick decided to get clean and sober, which he has been for seven years now. He moved to Atlanta five years ago and sees Emory doctors and specialists at the Atlanta VA Medical Center.
Although often still in pain, Kendrick says he doesn’t need or want heavy-duty medication. “I’ve sat in on some physical therapy orientation sessions at Emory because I want to encourage others,” he says. “There is
Kendrick earned a degree in business and is now a professional public speaker. After word got around that he had found a way out of opioid addiction, a few friends from the unit reached out. “I’m trying to be a mentor to them,” he says. “I tell them to focus on what’s really important in life.”







