FROM BENCH TO BREAKTHROUGH
How Emory health innovations — therapeutics, tools and
technologies — from trailblazing researchers are saving lives
around the globe.

HIV antiretroviral drugs taken by tens of millions of people. Virtual reality simulations that help people confront their phobias and addictions. AI-driven imaging solutions that pinpoint cancer cells.
These transformative innovations may seem worlds apart, but they share a common thread: Each began as a bold idea in an Emory lab and was nurtured through years of research, testing and collaboration. From the earliest phases of bench work to clinical trials and commercialization, the path to impact is complex and often high stakes.
Behind the scenes — and for 40 years now — Emory’s Office of Technology Transfer (OTT) has played a crucial role in bringing these big ideas to the marketplace by helping researchers secure patents, navigate licensing and launch partnerships. Since its founding in 1985, the office has supported the development of 26 FDA-approved drugs, 24 medical devices and more than 130 startup companies.
“When it comes to measuring success in tech transfer, nothing matters more than getting new products to market,” says Todd Sherer, Emory associate vice president for research and OTT’s executive director. “That’s the ultimate validation of our work — it proves the impact of university research in real-world terms. While we certainly track metrics like invention disclosures, patents and licenses, those are means to an end. The true measure is whether a discovery becomes something that helps people.”
The following stories celebrate some of the university’s most groundbreaking medical and healthcare innovations — and the researchers whose work from the lab bench is creating real-world impact.
HOW EMORY HELPED CHANGE
THE COURSE OF HIV TREATMENT
It’s estimated that more than 90 percent of people in the U.S. living with HIV — and millions more around the world — have taken at least one of the life-saving drugs developed by Emory researchers Dennis Liotta, Ray Schinazi and Woo-Baeg Choi. These medications helped transform HIV from a fatal diagnosis into a manageable chronic condition and in doing so reshaped public health on a global scale.
Effective HIV drugs developed by Emory researchers mean the disease is now manageable rather than a death sentence.
Effective HIV drugs developed by Emory researchers mean the disease is now manageable rather than a death sentence.
The journey began in the early 1990s, when Liotta, a chemistry professor, resolved to tackle the HIV/AIDS epidemic head-on.
“I made it my personal goal to create a safe and effective AIDS drug,” says Liotta, Samuel Candler Dobbs Professor of Chemistry. “It is so gratifying that it became part of a series of combination therapies that transformed AIDS from a death sentence to a manageable chronic disease.”
Liotta partnered with virologist Schinazi and postdoctoral researcher Choi to develop two groundbreaking compounds: 3TC (lamivudine, sold as Epivir) and FTC (emtricitabine, sold as Emtriva). Both are nucleoside reverse transcriptase inhibitors — a class of drugs that stops HIV from replicating.
“In addition to being quite effective, Emtriva is one of the safest antiretroviral agents available,” says Liotta. “This is quite important because AIDS patients have to take their drug regimens every day of their lives.”
Emory’s patent for one of the drugs was filed just seven days ahead of a competing group, but it would take nearly a decade of laboratory refinement, testing and commercial groundwork before either compound reached the market.
That persistence paid off. In 2001, Epivir became the first Emory-developed drug to win FDA approval, followed by Emtriva in 2003. These medications became central components of Truvada, a once-daily HIV treatment approved in 2004 — and later the first drug approved to prevent HIV infection in high-risk populations.
By 2006, Atripla —a single-tablet regimen combining Emtriva with two other agents — simplified HIV treatment further, reducing the number of pills patients have to take and improving patient compliance around the world. In addition to its use in HIV, Epivir is widely used to treat hepatitis B (HBV), which affects over 400 million people globally and is a leading cause of liver cancer. Schinazi also discovered telbivudine, another highly effective treatment for HBV.
“Everyone was intrigued but skeptical about our work — no one realized the importance of what we had found,” recalls Schinazi, professor of pediatrics, director of the Laboratory of Biochemical Pharmacology and co-director of the HIV Cure Scientific Working Group at Emory.
“It’s very gratifying to see that our work has helped so many people all over the world. HIV is no longer a death sentence.”
The collaborative spirit among Liotta, Schinazi, and Choi became a model for how Emory approaches research innovation.
“When the overriding goal is the health of patients, every source of insight and expertise is welcome,” says Liotta. “That culture is part of what made our discovery possible.”
Their success also catalyzed the future of drug development at Emory. In 2005, the university sold rights to future Emtriva royalties in what was then one of the largest intellectual property deals in higher education. The proceeds were reinvested into research, including the creation of two Emory-linked entities: the Emory Institute for Drug Development (EIDD) and DRIVE (Drug Innovation Ventures at Emory). Funded in part by Liotta’s own share of earnings, the two groups work together to move scientific discoveries into therapeutic realities — and were instrumental in the discovery of molnupiravir, an antiviral used during the COVID-19 pandemic.
Now, Emory’s HIV legacy continues through a new generation of researchers. Christina Gavegnano, once a graduate student in Schinazi’s lab, recently led the discovery of a first-in-class therapy that could address HIV persistence — the virus’s ability to hide in the body despite treatment. Her small-molecule compound, VIP943, targets and eliminates the HIV reservoir using the cell’s own degradation machinery.
“This could be a turning point in the fight against HIV,” says Gavegnano, now an assistant professor at Emory. “We’re attacking the root of viral persistence, not just suppressing symptoms.”
FIGHTING COVID-19 WITH
ORAL THERAPUETICS
Years before the pandemic emerged, Emory scientists were developing what would become one of the world’s first oral treatments for the virus.
Beginning in the early 2010s, George Painter, along with fellow Emory researchers Gregory Bluemling, Michael Natchus, David Guthrie and David Perryman, worked on EIDD-2801 — a broad-spectrum antiviral first aimed at Venezuelan equine encephalitis, a Cold War-era bioterrorism threat. Their compound showed promise against multiple viruses, including influenza and coronaviruses. When COVID-19 struck, they quickly repurposed it.
Molnupiravir halts the viral spread of COVID-19 and is being studied as a way to fight enchephalitis and influenza.
Molnupiravir halts the viral spread of COVID-19 and is being studied as a way to fight enchephalitis and influenza.
Renamed molnupiravir — after Thor’s mythical hammer — the drug became one of the first oral medications approved to treat COVID-19. It was the 26th FDA-approved drug born at Emory, and DRIVE’s first to reach the market.
Molnupiravir works by targeting the virus’s replication machinery. It introduces errors into SARS-CoV-2’s genetic code, essentially jamming the “copy machine” the virus uses to reproduce. If taken early, the drug halts viral spread in the body and helps prevent severe illness.
In November 2021, the U.K. approved molnupiravir for high-risk patients, followed by U.S. FDA Emergency Use Authorization the next month. Painter, hearing it could save lives, wept. “It was a little overwhelming, to tell the truth,” he says.
The pill’s portability — no injections, no cold storage — made it especially practical in global settings. Clinical trials showed it could eliminate infectious virus from nasal swabs within five days.
Even as molnupiravir, now sold by Merck as Lagevrio, continues to help COVID-19 patients, Emory scientists are studying its use against other RNA viruses, including encephalitis and influenza. “Our continuing mission is to search for other antiviral agents that are usable by the general public to address other tough diseases,” says Painter. “So, we are on it. That’s our job.”
Another Emory-driven breakthrough during the pandemic was baricitinib, an anti-inflammatory drug originally used for rheumatoid arthritis. In international clinical trials led by Emory physician-scientist Vincent Marconi, it significantly reduced the risk of death in hospitalized COVID-19 patients requiring oxygen or ventilation. The FDA later authorized it as a standalone treatment.
The drug’s success was rooted in earlier Emory research on JAK inhibitors for HIV, led by Schinazi and Gavegnano. That groundwork provided the scientific basis for rapidly repurposing baricitinib to address COVID-19’s deadly immune overreaction.
“Our extensive work with JAK inhibitors in the HIV space became a roadmap for tackling COVID-19 in record time,” Gavegnano says.
Emory and the U.S. Department of Veterans Affairs hold patents on this approach, licensed to Eli Lilly in 2021. Like molnupiravir, baricitinib reflects Emory’s vital role in turning decades of research into timely, life-saving treatments.
THE TELL-TALE HEART:
THE EMORY CARDIAC TOOLBOX
A 3D image of a beating heart rotate on screen. Nearby, color-coded scans reveal blood flow through the heart muscle — highlighting areas of concern in black voids. This technology, the Emory Cardiac Toolbox (ECTb), is one of the most widely used cardiac imaging systems in the world.
Developed by researcher Ernest Garcia, now a professor emeritus of radiology at Emory’s School of Medicine, the Toolbox helps answer a critical question: Does a patient have coronary artery disease? Over three decades, Garcia and his collaborators at Georgia Tech and Cedars-Sinai built a suite of software tools that allow physicians to analyze blood flow and heart function with greater precision.
The Toolbox’s latest advances help identify which patients are likely to benefit from cardiac resynchronization therapy, a method used to correct irregular heartbeats. “Just by analyzing how the heart beats, we can now predict whether resynchronization will help restore proper rhythm,” Garcia says.
Emory began licensing the software in the 1990s, and in 1999 helped launch Syntermed Inc., which distributes the technology worldwide. With more than 10,000 installations, ECTb has become a global tool in the fight against heart disease.
Garcia, who credits the software with saving his own life after a cardiac event, sees its reach as a model for academic medicine. “Once you feel the satisfaction of walking into a hospital in China or Italy and seeing your software helping a patient,” he says, “you realize this is exactly what research should do—translate into something that improves lives.”
Emory has helped move more than 65 breakthroughs from discovery to market. Discover more of these success stories that are saving lives.

AI AT WAR WITH CANCER:
SMARTER IMAGING FOR SMARTER TREATMENT
Imagine cancer treatment as a war, and the physician as the general who must pinpoint the enemy’s exact position. Thanks to AI-powered molecular imaging software, doctors now have sharper, faster, and more personalized tools to guide their strategy.
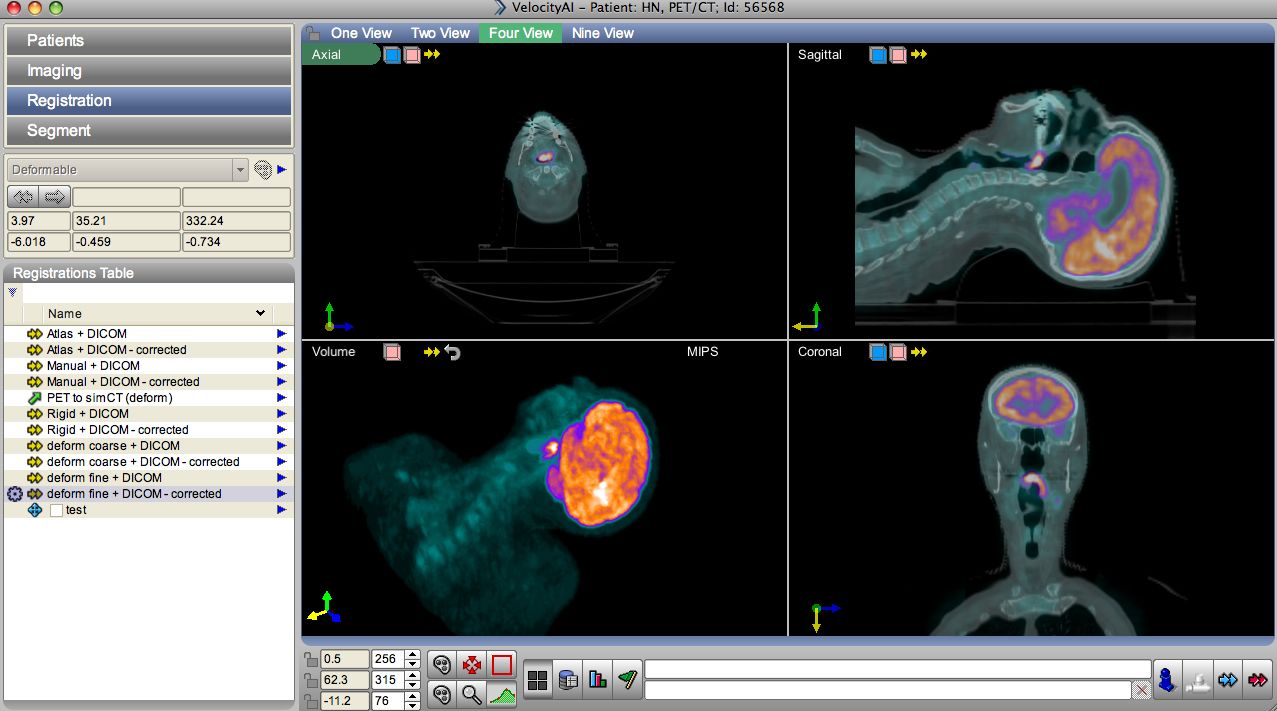
Developed at Emory by radiation oncologists Tim Fox and Ian Crocker, the technology — Velocity AI — helps physicians “see” cancer more clearly by integrating multiple scans into one dynamic, 3D-like image. The core technology, deformable image registration, aligns soft tissue across different image sets, warping and matching them to provide a high-resolution view of tumor boundaries.
“Essentially, we're trying to use imaging more as a predictive tool for cancer,” says Fox. “If you're able to assess the tumor response more quickly, then you can modify the treatment if the patient is not responding. It could have a huge impact on patient care.”
Velocity AI helps physicians see cancer more clearly by combining scans into a dynamic 3D image that precisely maps tumor boundaries.
Velocity AI helps physicians see cancer more clearly by combining scans into a dynamic 3D image that precisely maps tumor boundaries.
Fox likens the system to Doppler radar — allowing physicians to track tumors and their response to therapy in real time. What once took hours can now happen in seconds, improving workflow and enabling faster clinical decisions.
In 2014, Varian Medical Systems acquired Velocity Medical Solutions, expanding the reach of the software. Today, Velocity is used in more than 200 cancer centers worldwide, helping physicians reduce uncertainty and better target their treatments.
“We needed to do a better job integrating imaging into the treatment planning,” says Fox. “From there, we just kept adding to it —creating a tool that solved a lot of our problems.”
As cancer remains the second leading cause of death in the U.S., innovations like Velocity AI offer new hope by turning complex data into clearer decisions — and better outcomes.
BUILDING A CULTURE OF
ENTREPRENEURSHIP

AT EMORY, ENTREPRENEURSHIP IS BECOMING EVERYONE’S BUSINESS. It’s gaining traction all across the university, showing up in classrooms, labs, studios and even dorm rooms. The goal: make entrepreneurial thinking more inclusive, interdisciplinary and part of everyday academic life.
“There’s great work happening in all of our schools and across our campuses,” says Wilbur Lam, Emory’s inaugural vice provost for entrepreneurship. “By connecting these efforts, we’re starting to build a pipeline that supports faculty and students no matter their background or discipline.”
Lam brings extraordinary firsthand experience to the job. A pediatric hematologist, bioengineer and serial entrepreneur, he’s led major research labs, helped bring diagnostics to market, mentored student teams and served as a national advisor to the NIH and FDA during the COVID-19 pandemic.
“I’ve seen how challenging it can be to translate academic work into real-world impact,” he says. “And I’ve also seen what happens when the right support is in place.”
Since stepping into the role a year ago, Lam has worked to align Emory’s many entrepreneurial efforts — encouraging collaboration, surfacing new ideas and guiding projects from concept to launch. One key initiative is Emory’s first university-wide innovation council, where leaders from across schools now meet regularly to share strategies and spark new working partnerships.
The Hatchery, Emory’s student startup hub launched in 2020, has already become a go-to space where graduate and undergraduate students across all disciplines learn how to bring their ideas to life. Now entering what Lam calls its “2.0” phase, The Hatchery is working closely with school leaders to expand entrepreneurial education and programming for student, faculty and staff innovators across the university. “We see The Hatchery as a place where all our learners can give birth to their ideas, and find the community and mentorship to grow them,” he says.
While the university’s Office of Technology Transfer continues to be a bedrock of support for patents, licensing and commercialization, Lam is overseeing efforts to complement that work by focusing on what comes before: surfacing ideas, nurturing new skills and building the confidence to experiment.
“Breakthroughs don’t always look like products or patents,” Lam says. “Sometimes it’s an unexpected synergy, a new model for delivery or a student reimagining a career path.”
One example of this mindset is the upcoming Stuart and Mimi Rose Program for Student Startups, a new for-credit innovation track that connects Goizueta Business School, Emory College of Arts and Science and The Hatchery. Open to students in any major, the Rose Program is designed to guide undergraduates through the process of developing a venture — from idea to launch — as part of formal coursework rather than solely extracurricular activity, Lam says.
He also sees incredible value in growing Emory’s ties to Atlanta’s broader entrepreneurial ecosystem. “We’re actively working with Georgia Tech, Children’s Healthcare of Atlanta and members of the city’s vibrant startup scene,” he says. “These partnerships give our students and faculty access to a powerful network of investors, incubators and business opportunities.”
To help bridge the gap between research and real-world impact, the university operates Emory Innovations Inc. (EII) to assist faculty in rigorously vetting discoveries and inventions that hold potential for commercialization. By de-risking early-stage concepts, EII helps increase their market readiness, Lam says.
“Innovation is a mindset,” Lam adds. “We’re working to build an ecosystem that empowers people across Emory to take chances, collaborate and lead. That culture is taking hold — and it’s getting stronger every day.”
VIRTUALLY BETTER: TREATING PHOBIAS,
ADDICTIONS AND PTSD WITH VR
The weather outside the room’s picture window is calm — blue skies, birds chirping. Then the wind picks up, rain spatters the glass, thunder rumbles, and the lights flicker out. For someone with a phobia of storms, these are powerful triggers. But in this case, the storm is virtual — controlled by a therapist and delivered through a headset.
Virtual Reality Therapy (VRT) immerses patients in realistic, computer-generated environments that help them gradually become more comfortable with fear-inducing situations. Since its founding in 1996, Virtually Better Inc. has led the way in developing virtual tools to treat anxiety disorders such as fear of flying, heights, and public speaking, as well as post-traumatic stress disorder (PTSD).
Virtually Better simulates realistic environments designed to help patients gradually become comfortable with fear-inducing situations.
Virtually Better simulates realistic environments designed to help patients gradually become comfortable with fear-inducing situations.
“Virtually Better provides an alternative to traditional exposure therapy,” says Jill Uhl, the OTT’s director of license and patent strategy and chief intellectual property officer.. “It allows patients to be treated in-office with greater convenience, lower cost, and less disruption.”
Emory professor of psychiatry Barbara Rothbaum helped pioneer the approach with Georgia Tech’s Larry Hodges. Their first study used virtual heights — glass elevators, bridges — to treat acrophobia. “We had been taking patients up tall buildings and to the top of the parking garage for years,” Rothbaum says, “but we discovered that the virtual reality exposure translated into real life. Seven out of ten people at the end of treatment were able to go into a real-life height situation.”
Today, Virtually Better helps veterans of the Afghanistan and Iraq wars confront trauma through simulated combat scenes. It’s also exploring addiction recovery using virtual bars and drug-use settings. A recent project, “CalmCraft: A Deep Sea Voyage,” helps children manage pain and anxiety through guided breathing in a virtual underwater world.
A SERENDIPITOUS SOLUTION:
OBIZUR AND HEMOPHILIA A
When Emory hematologist Pete Lollar, began researching blood coagulation in the 1990s, he didn’t intend to create a new treatment for hemophilia. But a surprising discovery in his lab would eventually lead to Obizur, a life-saving drug approved by the FDA in 2014 for acquired hemophilia A.
Hemophilia A is a bleeding disorder caused by a deficiency in clotting factor VIII (FVIII). While inherited cases are more common, acquired hemophilia arises when the immune system develops antibodies that inactivate FVIII — often with no prior warning. This can result in sudden, severe bleeding episodes that are difficult to treat.
Lollar and his research team, including Ernest Parker, John Healey and Rachel Barrow, developed a modified form of FVIII based on the pig version of the protein. Delivered intravenously, this recombinant porcine FVIII mimics the function of human FVIII but evades immune detection in patients with inhibitors.
“Porcine FVIII is similar enough to human FVIII to be effective in clotting, but less likely to be neutralized by antibodies,” the FDA explains.
Though the road to approval took 22 years, clinical trials confirmed Obizur’s safety and efficacy, particularly for patients with few other treatment options. The FDA also granted it orphan drug status, a designation that provides incentives like market exclusivity and tax credits to encourage development of treatments for rare diseases — defined in the U.S. as those affecting fewer than 200,000 people.
Now the Hemophilia of Georgia Professor of Pediatrics at Emory, Lollar reflects modestly on the achievement: “This is not really rocket science. We’re basically trying to replace a missing factor.” But for patients, the impact has been profound.
ENGINES OF INNOVATION

Many of Emory’s most impactful health science discoveries have made it out of the lab and into the world thanks in large part to the Office of Technology Transfer (OTT).
For four decades and counting, OTT has helped faculty secure patents, license technologies and launch startups. But in the past few decades, its work has become more than just a support service — it’s a driver of Emory’s mission to serve humanity.
“Early in my career, commercialization was often seen as a distraction from the core work of academia,” says Todd Sherer, associate vice president for research and executive director of OTT. “Today, that mindset has flipped. There’s a broad recognition that translating discoveries into impact is part of our social contract.”
That shift is visible across Emory’s campuses. Patent applications now count toward tenure in the School of Medicine, Sherer says. Internal seed funds and translational research programs support the long path from concept to clinic. Students with an entrepreneurial mindset can build prototypes and pitch ventures at The Hatchery, Emory’s innovation hub.
Sherer says this burgeoning ecosystem — from early-stage funding and career incentives to widespread support and engagement across the university — reflects a significant step forward. “Innovation is not a fringe activity at Emory.” he says. “It’s become a core mission embraced by the president’s and provost’s offices down to the researchers in our labs.”
Most important, Sherer says, in the world of tech transfer success breeds success. Licensing revenue from Emory’s HIV drugs helped launch its drug development arm, DRIVE, which then produced molnupiravir. Now, revenue from that antiviral and others are being reinvested to fuel future waves of innovation. It’s a model showing how academic innovation, when properly supported, can drive an enduring pipeline of life-saving products.
Story by Office of Technology Transfer staff and Roger Slavens. Design by Selena Lim.

Want to know more?
Please visit Emory Magazine, Emory News Center, and Emory University.