The Statesman vs. the Fiery Serpent

Nearly four decades ago, former President and University Distinguished Professor Jimmy Carter set out to eliminate Guinea worm disease from the globe.
He very nearly succeeded.

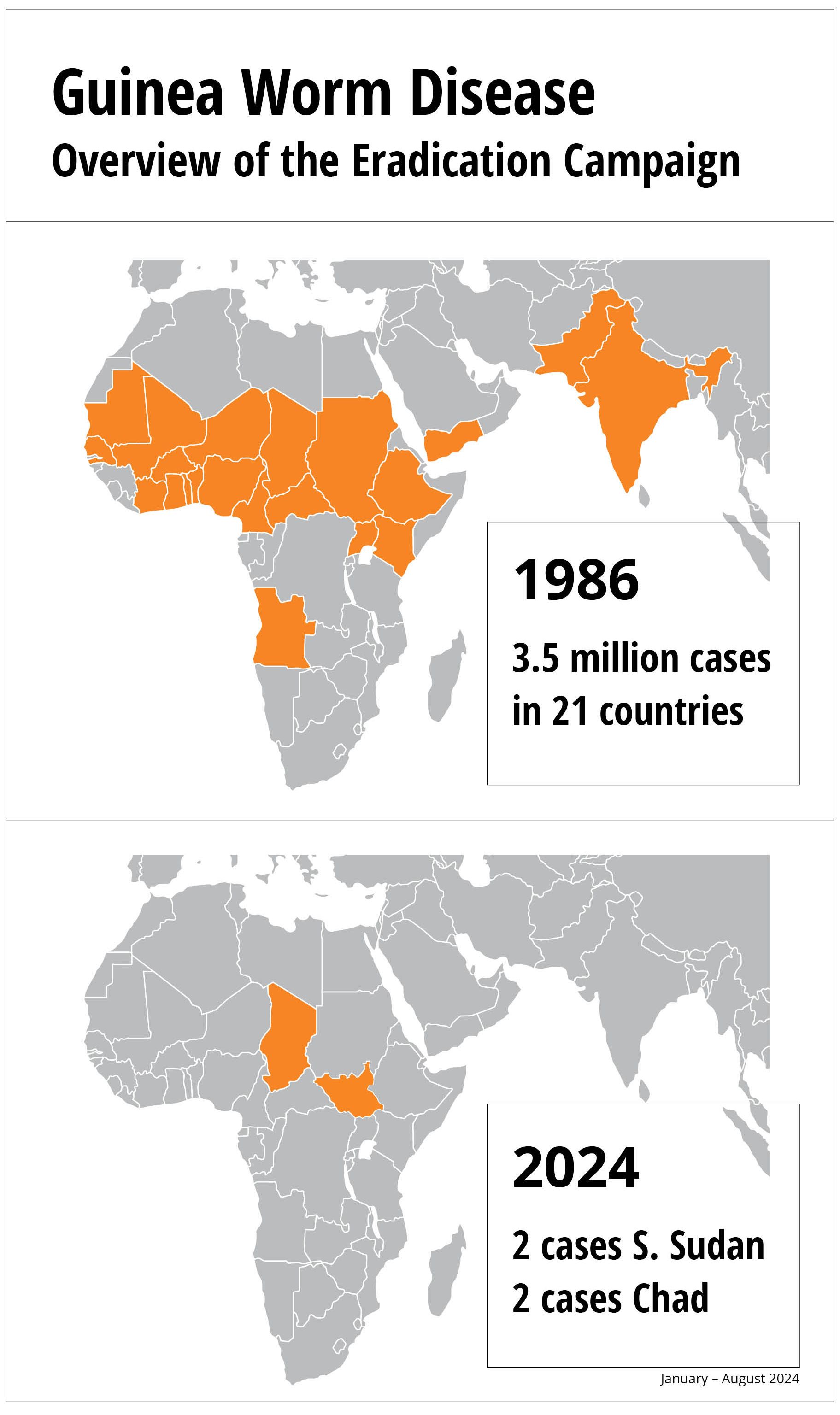
Former US President Jimmy Carter, who died Dec. 29 at 100, said on several occasions that he fervently hoped the last Guinea worm would die before him.
For centuries, the parasitic plague was endemic in countries around the globe.
Acquired by drinking Guinea worm-contaminated water, the female worm grows inside the human body for up to a year before it emerges—excruciatingly—through a blister. Development, sanitation and access to clean water eliminated the pest for about 70 percent of the global population, leaving only the most neglected people in the poorest nations vulnerable to the disease.
Those were the very people the former president was determined to help.
Carter, a University Distinguished Professor at Emory, made it a primary mission to wipe Guinea worm disease from every country in the world. He worked largely through the powerful health arm of his presidential center in Atlanta, the Carter Center.
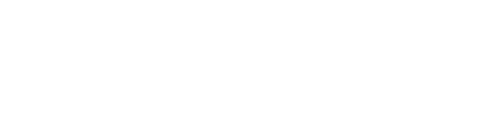
When the Carter Center took up the fight in 1986, there were an estimated 3.5 million cases per year in 21 African and Asian countries. So far this year, just four human cases have been reported. Guinea worm is poised to become the second human disease in history to be eradicated, following smallpox.
To achieve this staggering reduction, Carter leveraged the influence, connections and knowledge gained during his presidency.
At a hospital in Ghana, former President Jimmy Carter and his wife, Rosalynn, are present as a Guinea worm is slowly pulled from a child’s foot in 2007. Photo: The Carter Center/L. Gubb
At a hospital in Ghana, former President Jimmy Carter and his wife, Rosalynn, are present as a Guinea worm is slowly pulled from a child’s foot in 2007. Photo: The Carter Center/L. Gubb
He supported and supplied a unique coalition of “Guinea worm warriors” made up of endemic countries’ ministries of health, global experts, and community-based health workers. These warriors overcame rainy seasons that left entire communities inaccessible, dispelled long-held beliefs about the cause of Guinea worm disease, and, in some cases, informed country leaders about the existence of the disease in their populations.
Carter even negotiated a cease-fire in a brutal civil war in Sudan so health workers could access the country.
Eradication will be even more extraordinary because it will have been accomplished with no treatment, no vaccine, no acquired immunity, and no cure. The only tool: convincing people in remote regions of the world to change the way they have collected and consumed water for generations.
Hurdles remain on the path to eradication, including the recent emergence of Guinea worm in domestic dogs mainly in Chad. Together with the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC) and many other partners including Emory, the Carter Center is staying focused on its founder’s goal.
“Eradicating Guinea worm disease and the suffering it causes has long been a dream of my grandparents, and they have worked incredibly hard to make it a reality,” said Jason Carter, Carter Center board chair and eldest grandson of former President Carter and the late First Lady Rosalynn Carter. “They witnessed firsthand how this work improves the lives of millions of people, and the Carter Center will keep working with our partners until there are zero cases.”
Jason Carter addressed his grandfather's fight against guinea worm in his eulogy:
“The thing that’s remarkable [about Guinea worm] is that this disease is not eliminated with medicine. It’s eliminated by neighbors talking to neighbors about how to collect water in the poorest and most marginalized villages in the world. And those neighbors truly were my grandfather’s partners for the last 40 years. …
“When he saw a tiny 600-person village that everybody else thinks of as poor, he recognized it. That’s where he was from. That’s who he was. And he never saw it as a place to send pity. It was always a place to find partnership and power, and a place to carry out that commandment to love your neighbor as yourself. Essentially, he eradicated a disease with love and respect.”
Guinea worm has plagued humanity for at least 3,000 years. Calcified evidence of the worm has been found in Egyptian mummies, and it’s written about in Egyptian medical texts.
The Fiery Serpent
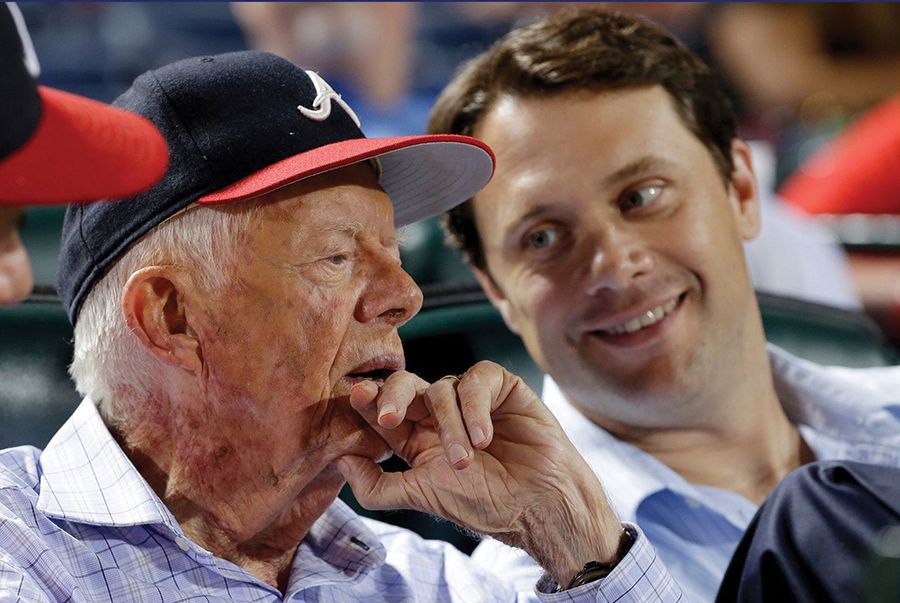
Parasitologists believe the biblical “fiery serpents” that attacked the Israelites who had escaped Egypt might have been Guinea worms. And some contend the snake that coils around a staff in the medical symbol is actually a Guinea worm.
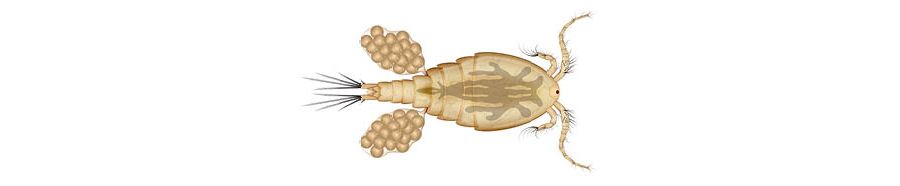
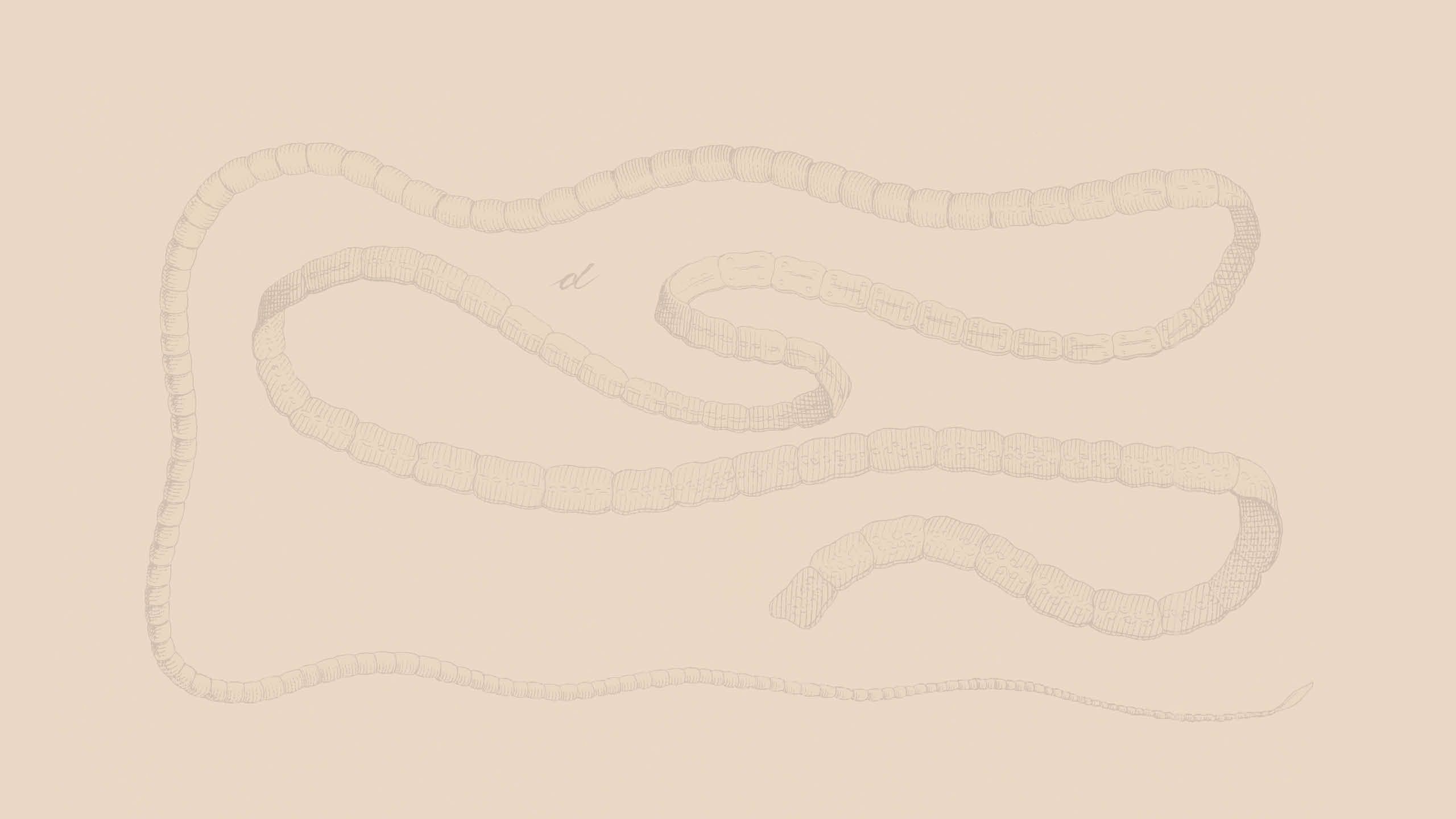
A person contracts Guinea worm from drinking stagnant water contaminated with tiny Cyclops fleas, which eat and then carry parasitic Guinea worm larvae. Once inside a person’s stomach, the flea breaks down and releases the male and female larvae, which mature and roam inside the abdomen until they find a mate. The male dies and the female continues to grow—reaching lengths of up to three feet.
Cyclops water fleas are intermediate hosts for Guinea worm.
Cyclops water fleas are intermediate hosts for Guinea worm.
Nine to 12 months later, the worm, which resembles a thin strand of spaghetti, finally emerges through a burning blister, usually in the lower limbs. The disease is also known as dracunculiasis, or “affliction with little dragons,” because the worm feels like tiny, hot daggers poking through skin.
Immersing the wound in water can soothe the burn but also causes the worm to release hundreds of thousands of larvae. The cycle may then begin anew.
Guinea worms are thin, thread-like parasites. Inside the human body, they can grow up to three feet long before emerging through the skin. Photo: The Carter Center
Guinea worms are thin, thread-like parasites. Inside the human body, they can grow up to three feet long before emerging through the skin. Photo: The Carter Center
The treatment is the same as it has been for thousands of years. The worm must be pulled gently from the wound, centimeter by centimeter, and wound around a twig or piece of gauze. The process is agonizingly slow, requiring anywhere from a few days to months to steadily tug the worm free.
Women have described the pain as worse than childbirth. Men have said it is more painful than a gunshot wound. The blister where the worm emerges often becomes infected, and if the worm happens to emerge from a joint, the person can be left crippled. Breaking an emerging worm will cause it to pull back into the body where it will die, calcify, and possibly cause deformities.
‘Public Enemy No. 1’
Compounding the disease’s heavy toll, the worms often emerge during the harvest season, devastating not only people’s bodies but their livelihoods. Crops cannot be harvested. Water cannot be collected. Children cannot attend school.
Emily Staub, an alumna of Oxford and Emory College, is associate director and press liaison to Health Programs for the Carter Center. She has seen firsthand the devastation the worm inflicts on its victims: A fierce faced, massively muscled man, normally stoic like most villagers, lay in the dirt and moaned as a worm was pulled from his leg. A young mother of several children, all of whom had emerging worms, sobbed out her anguish and shame, believing she had brought on a hex that afflicted her children. A 6-year-old girl screamed at the top of her lungs outside a dark hut, begging others not to touch the worm coming out of her foot and swatting away their hands.
Another child missed so much school because of Guinea worm that her parents decided not to send her back. “Her life was forever changed by a slim, three-foot-long worm,” says Staub. “Neglected tropical diseases like Guinea worm don’t kill you, but they can take away your opportunities and your dignity.”
Stories such as these explain the names given to Guinea worm through the decades. Roughly translated, these include “the empty granary,” “public enemy No. 1,” “the crippler,” and “the impoverishment.”
As devastating as the worm is, it can easily by stopped by filtering the tiny fleas out of contaminated water and keeping infected people out of water sources. This disease strikes mostly marginalized and isolated people in the poorest of countries, however—places where nothing is particularly easy.
Some contend the snake that coils around a staff in the medical symbol is actually a Guinea worm. The disease is also known as dracunculiasis, or “affliction with little dragons,” because the worm feels like tiny, hot daggers poking through skin.
Some contend the snake that coils around a staff in the medical symbol is actually a Guinea worm. The disease is also known as dracunculiasis, or “affliction with little dragons,” because the worm feels like tiny, hot daggers poking through skin.
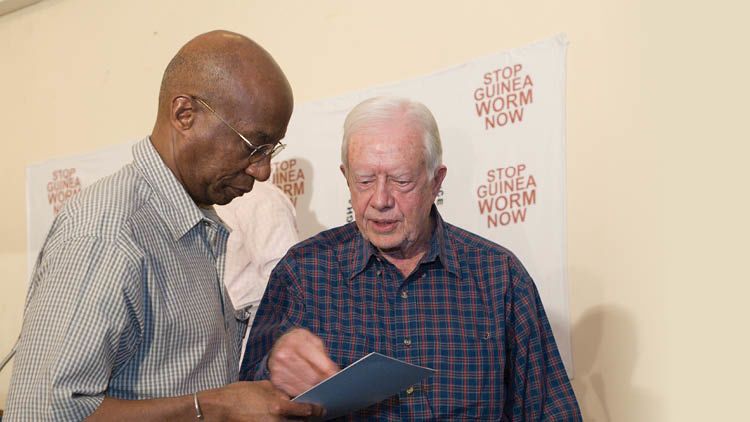
Donald Hopkins, special advisor for the Guinea Worm Eradication Program, talks with former President Carter in Ghana in 2007. Photo: The Carter Center/L. Gubb
Donald Hopkins, special advisor for the Guinea Worm Eradication Program, talks with former President Carter in Ghana in 2007. Photo: The Carter Center/L. Gubb
Former President Jimmy Carter and World Health Organization (WHO) Director-General Margaret Chan attend a press conference in London announcing a new funding campaign for the eradication of Guinea worm disease in 2011. Photo: Imago
Former President Jimmy Carter and World Health Organization (WHO) Director-General Margaret Chan attend a press conference in London announcing a new funding campaign for the eradication of Guinea worm disease in 2011. Photo: Imago
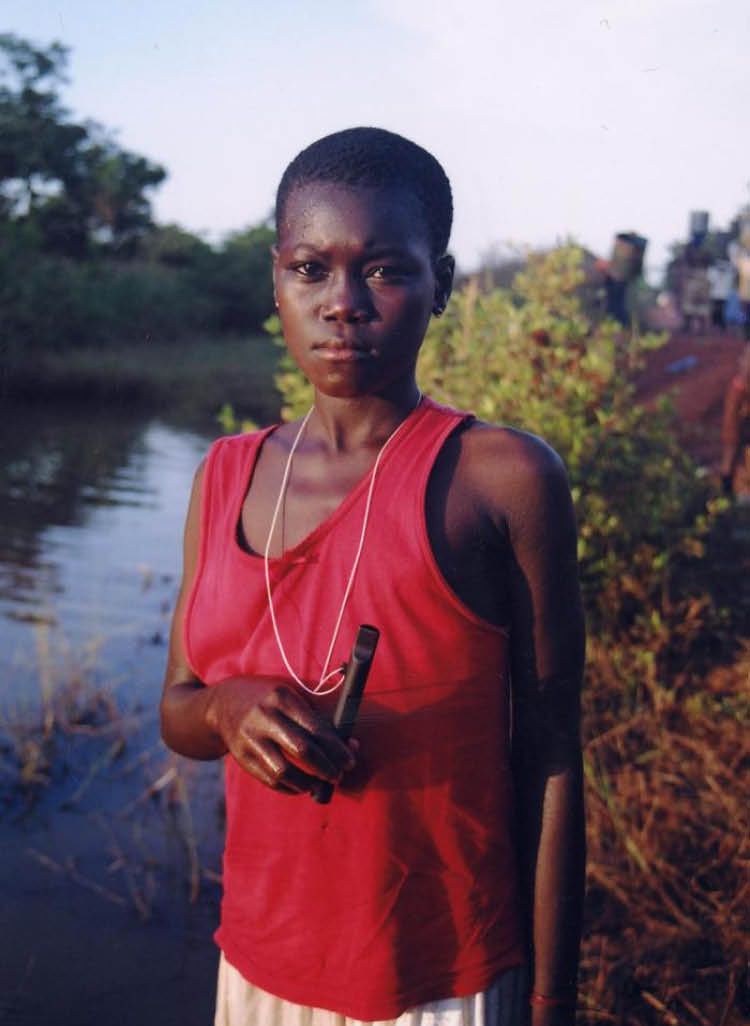
A woman uses a Carter Center-donated fine mesh filter cloth fitted over a clay pot used to hold water. Filtering the tiny water fleas out of drinking water is the most effective way to prevent Guinea worm disease. Photo: The Carter Center/E. Staub
A woman uses a Carter Center-donated fine mesh filter cloth fitted over a clay pot used to hold water. Filtering the tiny water fleas out of drinking water is the most effective way to prevent Guinea worm disease. Photo: The Carter Center/E. Staub
A Game Changer
Donald Hopkins and colleagues at CDC began trying to drum up interest in fighting Guinea worm in the early 1980s. However, the former deputy director and then acting director of the CDC had little success generating support or funding to wage a campaign against a disease most people had never heard of, that occurred in the most desolate of places.
“We started looking around for a celebrity who could bring attention to the cause,” says Hopkins, former director of health programs at the Carter Center and current special advisor for the Guinea Worm Eradication Program. “We were actually thinking about trying to get Harry Belafonte. But then President Carter got involved, and it was a game changer.”
For his part, Carter adopted the cause shortly after he and his wife, Rosalynn, in partnership with Emory, established the Carter Center, a nongovernmental, non-profit dedicated to “Waging Peace. Fighting Disease. Building Hope.”
Carter wanted his center to focus on areas others were ignoring, and when a friend and former member of his presidential administration told Carter about Guinea worm, he was interested. When he traveled to a small village in Ghana where many of the residents were incapacitated due to Guinea worm, he grew indignant. Among the afflicted villagers was a young woman whom Carter thought was holding her infant. However, when he went to greet the baby, he realized she was holding not her infant but her hugely swollen breast, from which a thin, white worm was emerging.
Carter took up Guinea worm as a personal mission and made it a flagship program of the center. Today, the Guinea Worm Eradication Program, which includes a large number of Emory alumni, is but one of the center’s programs targeting neglected tropical diseases.
“Guinea worm was a disease no one else was willing to tackle—it was ignored by governments and NGOs alike because it was too obscure and afflicted only the world’s most forgotten people,” says Kelly Callahan, an alumna of the Rollins School of Public Health and director of the Carter Center’s Trachoma Control Program who previously worked in the Guinea worm program. “That’s precisely why President Carter decided to take it on.”
That said, Callahan and other Carter Center officials are quick to point out that each country’s Guinea worm program is run by its ministers of health. The center works closely with government officials to provide technical guidance and logistical and financial support.
The Carter Center team knew getting safe water to far-flung, isolated villages was going to be too expensive, too political and take too long. Instead, the center embraced the option of teaching people in vulnerable areas to filter their water, giving them the low-cost tools to do so.
The challenge was accelerated by Carter’s astute understanding of global politics, connections and access to leaders across the world, as well as personal strength of character.
Carter used his international clout to arrange meetings with the leaders of countries where Guinea worm was endemic and often had to educate them about the problem. When he visited Pakistan in the early days of the campaign, the president and the minister of health had never heard of Guinea worm and didn’t know it existed in their country. (Pakistan became the first of the remaining countries with endemic Guinea worm to eradicate it in 1997.)
Not content to only meet with presidents and ministers of health in capital cities, Carter ventured into the most remote villages to see the work firsthand. He convinced some leaders to accompany him to areas they had never visited.
And he used his influence to convince countries and corporations to take up the charge. Carter persuaded large companies to create, manufacture and donate the specialized cloth needed to filter water, portable filter pipes (Guinea worm “straws”) that could be worn around the neck, and larvicide for targeted bodies of stagnant water.
“It’s not possible to overstate President Carter’s impact on Guinea worm eradication,” says Adam Weiss, alumnus of Emory’s Rollins School of Public Health and director of the Guinea Worm Eradication Program. “He made inroads with foreign leaders through his diplomacy. The fact that he actually traveled to the more remote villages made such an impact, not only on the villagers but on the health workers and leaders—they knew he meant business. And he was able to get donations to a cause no one had supported before.”
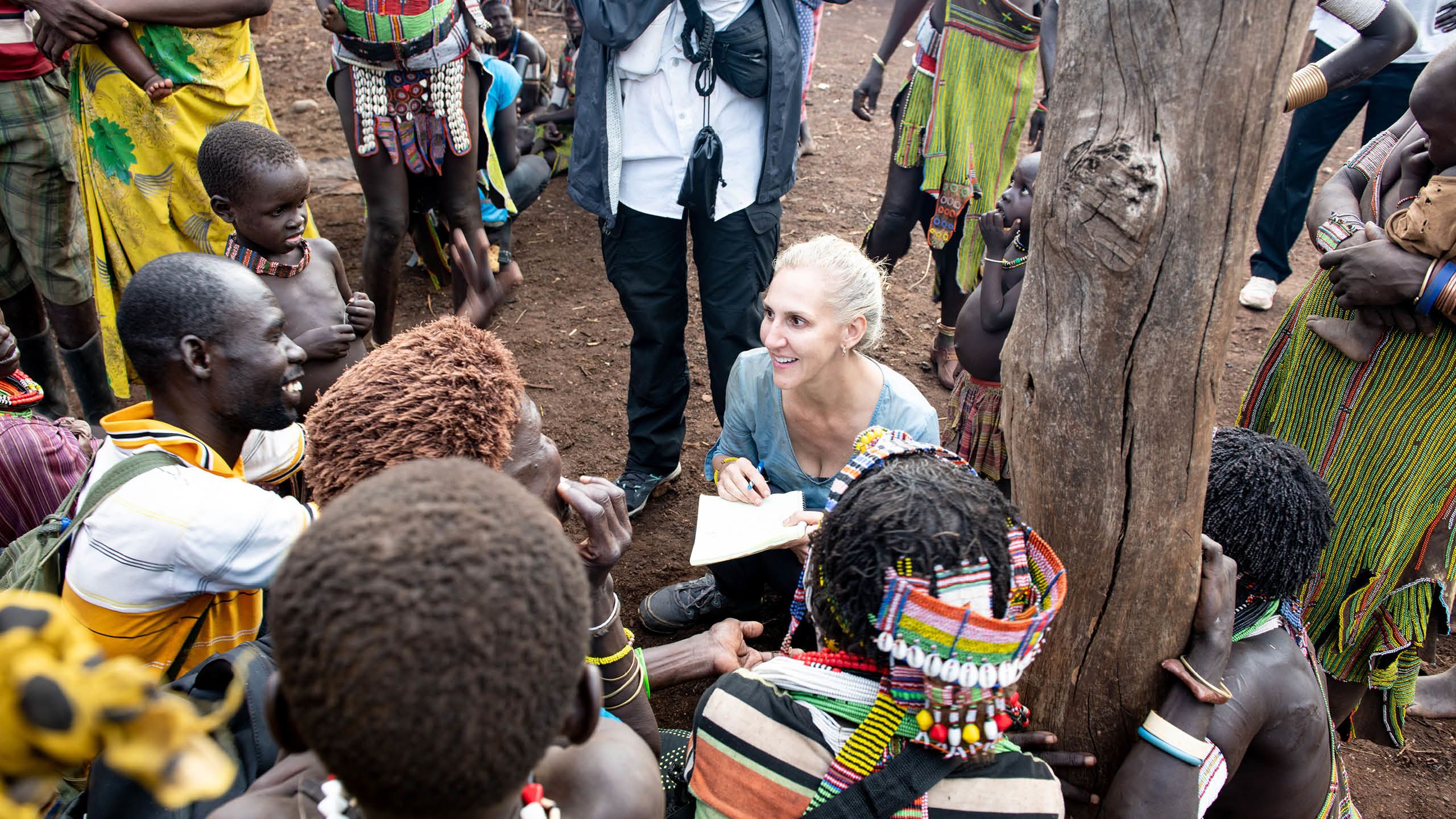
As critical and influential as Carter has been to the eradication efforts, Weiss and others on the eradication team acknowledge that the real work happens on the community level. Health workers from the national program and often the Carter Center worked to train hundreds of thousands of local health workers and village-appointed volunteers in their communities. Since the start, health education and training has taken place in more than 23,000 villages across in 21 countries in Africa and Asia.
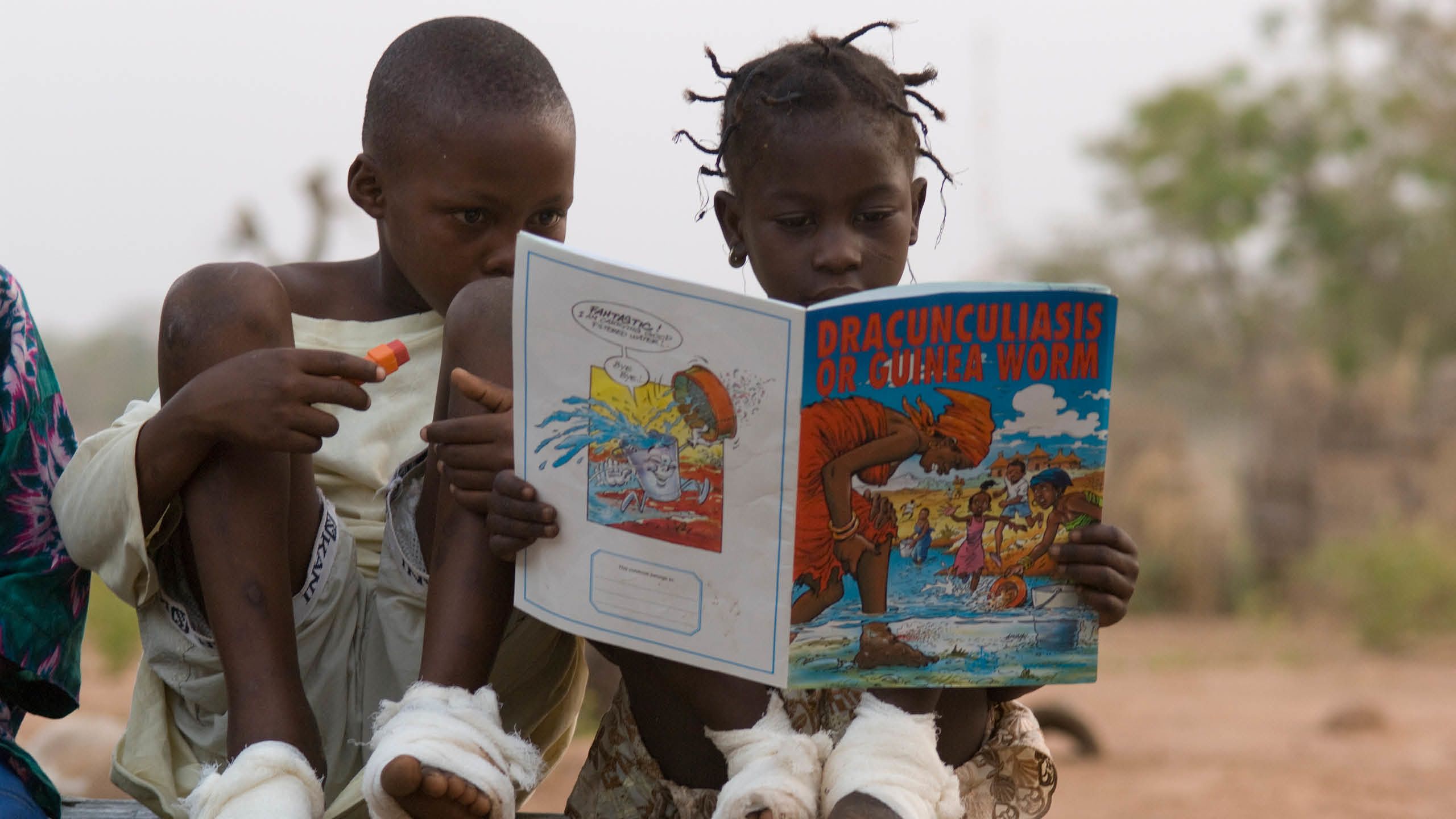
The volunteers go from dwelling to dwelling or visit farming plots or moving groups, using picture books, skits, stories and songs to educate their neighbors about how Guinea worm is contracted and how to prevent it.
They demonstrate the ways to properly filter all drinking water, such as using a pipe filter or fitting the cloth filters snugly over a bucket or large clay drum used for household water storage. They explain why people who have a Guinea worm need to stay out of any water sources, and if someone has already gone in the water, they make sure larvicide is swiftly added to that source to prevent transmission. They report anyone who shows signs of an imminent or emergent worm so the individual can be monitored and taken care of at containment center if they prefer.
The containment centers can offer faster, more sanitary worm extractions, along with meals, a sleeping mat, access to safe water and space for dependents. Once the worm is extracted, the person can depart with the bed mat and sheet, and perhaps a bag of sorghum to compensate for the time they missed out on working.
“We [Carter Center staff] provide the tools and the support, but the village coordinators and volunteers are the ones who were eradicating Guinea worm,” says Sarah Yerian, an alumna of Emory’s Rollins School of Public Health and senior associate director of the Guinea Worm Eradication program. She worked in South Sudan first as a technical advisor, then as a regional coordinator, and later as the center’s country lead. “I’d do whatever I could. When I was checking in on one of the villages in my territory, I’d hike out into the fields and gardens if it was planting season. I’d pick up a hoe and do some planting so the woman could sit and talk to the volunteer, who did all the education about Guinea worm and its prevention.”
A pipe filter can be worn around the neck, as seen here on a woman in Ghana, and used while drinking directly from water sources to filter out the fleas that cause Guinea worm disease. Photo: The Carter Center/E. Staub
A pipe filter can be worn around the neck, as seen here on a woman in Ghana, and used while drinking directly from water sources to filter out the fleas that cause Guinea worm disease. Photo: The Carter Center/E. Staub
In places where larger household water filters weren’t feasible, such as populations displaced by conflict, the Carter Center borrowed an idea from the Tuareg, a nomadic tribe in West Africa. These tribesmen cut up the larger household filters into smaller bits and tied them to the end of hollow reeds, using them as straws to suck water through. The center created a more durable prototype patterned after these hand-made devices and added a string so it could be worn around the neck. In 2001, more than 9 million pipe filters were distributed in southern Sudan, which was the largest public health intervention at the time. The design was further refined and manufactured with help from the Danish company Vestergaard. The portable pipe filters have since been distributed in all endemic countries.
The Carter Center had filter pipes made and distributed to more than 9 million people in southern Sudan in what was the largest public health intervention at the time.

Overcoming Obstacles
The path to eradication has been anything but smooth. Ghana had been making significant progress when a new president who did not prioritize Guinea worm prevention efforts came to power. For about 10 years, the number of cases remained stagnant, and local leaders became complacent. Then a big outbreak sent the numbers soaring, erasing years of progress. Carter visited afflicted villages and was so frustrated by the reversal that he threatened to rename the plague Ghana worm. His visit re-energized the program, and Ghana was declared Guinea worm free in 2015.
War posed another roadblock. In 1995, Carter used his diplomatic ability—including the threat to publicly shame the country’s leaders in a CNN press conference he called for that reason—to help negotiate a six-month-long cease-fire in Sudan between opposing sides that had been engaged in a brutal civil war. The cease-fire, the longest humanitarian cease-fire in history at the time, allowed health workers to access previously inaccessible areas to distribute medicine and preventative health measures going beyond just Guinea worm. In addition to distributing more than 200,000 cloth filters to about 2,000 endemic villages, health workers delivered treatment and education to prevent river blindness, another neglected tropical disease. They also immunized an estimated 100,000 children against measles and polio.
Today, conflict and insecurity in places like Mali, South Sudan, and Ethiopia means people can be displaced and delivery of supplies interrupted. “The benefit of being community-based and having nearly 100 percent of your local staff and volunteers native to that country is that even if people are displaced or put on lockdown temporarily, the staff and volunteers are among them, continuing to teach and monitor,” says Weiss. “That makes the system very resilient.”
Women gather water from a local pond and carry it to their homes in large barrels atop their heads. This water must be filtered to remove the copepods (water fleas) that can carry the parasitic larvae of the Guinea worm. Photo: The Carter Center
Women gather water from a local pond and carry it to their homes in large barrels atop their heads. This water must be filtered to remove the copepods (water fleas) that can carry the parasitic larvae of the Guinea worm. Photo: The Carter Center
Adam Weiss, director of The Carter Center Guinea Worm Eradication Program, gently pulls a Guinea worm from a young boy's ankle in Ghana. Photo credit: The Carter Center/E. Staub
Adam Weiss, director of The Carter Center Guinea Worm Eradication Program, gently pulls a Guinea worm from a young boy's ankle in Ghana. Photo credit: The Carter Center/E. Staub
Sarah Yerian (far left), senior associate director of the Guinea Worm Eradication Program, demonstrates procedures for treating water sources with larvicide in South Sudan in 2019. Photo: The Carter Center
Sarah Yerian (far left), senior associate director of the Guinea Worm Eradication Program, demonstrates procedures for treating water sources with larvicide in South Sudan in 2019. Photo: The Carter Center
Kelly Callahan, director of The Carter Center's Trachoma Control Program, shows her digital camera to village children in Ghana in 2010. Photo: The Carter Center
Kelly Callahan, director of The Carter Center's Trachoma Control Program, shows her digital camera to village children in Ghana in 2010. Photo: The Carter Center
Donald Hopkins, special advisor for the Guinea Worm Eradication Program, talks with villagers in Nigeria about Guinea worm prevention in 2009. Photo credit: The Carter Center/E. Staub
Donald Hopkins, special advisor for the Guinea Worm Eradication Program, talks with villagers in Nigeria about Guinea worm prevention in 2009. Photo credit: The Carter Center/E. Staub
While at the containment center in Ghana, two young children look at a picture book about Guinea worm disease, learning that "you get Guinea worm from the water. If you drink it unfiltered, you get Guinea worm," the young girl said. In May 2010, with Carter Center support, Ghana reported its last case of Guinea worm disease and announced it had stopped disease transmission a year later. Photo: The Carter Center/L. Gubb
While at the containment center in Ghana, two young children look at a picture book about Guinea worm disease, learning that "you get Guinea worm from the water. If you drink it unfiltered, you get Guinea worm," the young girl said. In May 2010, with Carter Center support, Ghana reported its last case of Guinea worm disease and announced it had stopped disease transmission a year later. Photo: The Carter Center/L. Gubb
The emergence of Guinea worm in dogs in Chad has been a significant setback in eradication efforts.
The emergence of Guinea worm in dogs in Chad has been a significant setback in eradication efforts.
The Final Hurdle: Dogs
The current number of Guinea worm cases would be a blinding victory light at the end of an arduous tunnel if not for a relatively recent development—the emergence of Guinea worm in domestic dogs in Chad. Though a challenging setback to be sure, those fighting the disease have deployed interventions and are searching for new tools to deal with the canine disease reservoir.
In 2012, some 50 dogs were found to have Guinea worm in Chad, and the numbers climbed each year. The new development confounded Weiss and colleagues. “I’ve been in this program for more than 20 years, and I was taught that this is a human disease, period,” says Weiss. “When it turned up in dogs, we didn’t know if this was a game stopper or a game changer.”
Field staff concluded the dogs were contracting the disease by eating raw fish guts and other aquatic waste discarded when villagers were preparing food. Another intervention was launched – convincing people to bury fish waste and tether dogs, especially if they have emerging worms.
“We estimate some 80 percent, or over 30,000 dogs, at the household level are being tethered,” says Weiss. “As a result, we had a 40 percent decrease in animal infections in 2024 from 2023.”
Members of the Carter Center Guinea Worm Eradication Program remain convinced eradication can and will be achieved. “We are in one of the best positions we’ve ever been in as far as the momentum and will to get it done,” says Weiss. “Everyone understands the risk. If you let up on the gas pedal at this point, even a little, you risk losing all the ground you’ve made. No one wants that to happen.”
A Powerful Legacy
When the last Guinea worm dies, untold millions will be spared needless suffering, and not only their health but their opportunities will improve. “In the early years, we found that eliminating Guinea worm from a community had a 29 percent economic rate of return,” says Staub. “In Ghana, one area increased its yam production 50 percent within a year of eradicating Guinea worm. By eliminating Guinea worm from a region, you are eliminating a source of poverty.”
The Guinea Worm Eradication Program also leaves behind reinforced health and surveillance systems in areas that previously lacked them. And the people who have been involved in the efforts have more opportunities and trained skills. Greg Vaughn, an Emory alumnus and a partner with Spencer Stuart, who sits on the board of trustees at Emory as well as the Carter Center, visited a village in South Sudan that was free of Guinea worm. “I was struck by how being trained and educated as part of the Guinea worm eradication effort opened doors for many,” he says. “Some had gone on to become teachers. Others were working within the county health department. They were able to have better lives as a result of working in the Guinea worm program.”
Perhaps the most powerful legacy of Guinea worm eradication, though, will be hope.
“I think it will change the mindsets of people in the villages as well as people in the ministries of health,” says Hopkins. “They can attack other problems that have lingered through generations, and they can alleviate more suffering.”
And, at long last, Jimmy Carter’s most fervent wish will be realized.
Written by Martha Nolan. Design by Peta Westmaas. Edited by Mary Loftus.
COLLABORATIONS
The collaboration between Emory University and the Carter Center, established in 1982, has fostered an extraordinary community of scholarship and practice, advancing peace and improving health around the world. President Jimmy Carter referred to the partnership as a “marriage that has worked out quite well.”
Emory faculty, alumni, staff and students contribute to Carter Center fieldwork, with Emory students providing the largest cohort of interns for the center. And center experts are Emory adjunct professors, aiding faculty research and bringing their expertise in international affairs, conflict resolution, public health and more into the classroom.
HEALTH PROGRAMS
In addition to Guinea worm, the Carter Center’s Health Programs fight five other diseases by using health education and simple, low-cost methods. The diseases are:
River blindness. A parasitic infection that can cause intense itching, skin discoloration, rashes, and eye disease that often leads to permanent blindness. The parasite is spread by the bites of infected black flies that breed in rapidly flowing rivers.
Trachoma. A bacterial eye infection found in marginalized, isolated communities lacking basic hygiene, clean water, and adequate sanitation. Trachoma is easily spread from person to person through hands, clothes and eye-seeking flies. It eventually causes blindness if left untreated.
Schistosomiasis. A waterborne parasitic infection that damages internal organs. The most common symptoms are blood in urine and/or feces and an enlarged liver, diarrhea, abdominal pain, weakness and anemia.
Lymphatic filariasis. Caused by thin worms transmitted to humans by the bites of mosquitoes. These worms damage lymphatic system that results in fluid collection in the tissues (most commonly the legs and genitalia), severe swelling, and periodic fevers. A long-standing infection can result in an irreversible condition called elephantiasis.
Malaria. A potentially fatal mosquito-borne parasitic disease, widespread in tropical and subtropical regions. Symptoms include fever, intense headaches, vomiting and body-shaking chills. Without treatment, malaria can lead to anemia, hypoglycemia, cerebral malaria, coma and death.