I AM AN EMORY RESEARCHER (COPY)
Seema Lakdawala: Understanding Influenza Transmission


Wilbur Lam Wants to Solve All the Problems
WILBUR LAM IS MANY THINGS. He is a professor of pediatrics and biomedical engineering, contact principal investigator of the Atlanta Center for Microsystems Point-of-Care Technologies, associate dean of innovation at Emory School of Medicine and director of the new center for the Advancement of Diagnostics for a Just Society. And he’s recently been named Emory’s inaugural vice provost for entrepreneurship.

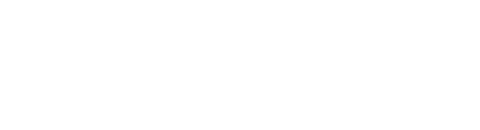
He’s married to Melissa Williams, a social psychologist and professor at Emory’s Goizueta Business School, and they have two children, a son in college and a daughter in high school. In his free time, Lam messes around on his Fender Stratocaster, harkening back to his time in a band comprised of pediatric residents named “Booster Shot.”
During residency training in pediatrics at the University of California, San Francisco, Lam was astounded by how antiquated clinical care technology was compared to the innovative research going on in labs at the same university—sometimes even in the same building.
“There’s always been a significant disconnect between the most cutting-edge stuff that’s being developed scientifically and what is serving patients,” he says.
That lag could be 10, 20, even 30 years. “So that’s what I decided to take on: to accelerate the time it takes to invent a technology and enable it to improve lives.” He combined his subspecialty training in cancer and blood diseases for children—pediatric hematology oncology—with a PhD in bioengineering.
Convergence of Cultures
Lam is the oldest son of a young couple who emigrated from Hong Kong to Canada. His father’s job as a chemist in the oil and gas industry brought them to the U.S., and the family ended up in Houston.
Lam was accepted into a combined BA/MD program at Rice University’s Baylor College of Medicine. He spent much of his undergraduate years “playing guitar, picking up gigs, and meeting people,” he says. “So luckily, I had already been accepted to medical school.”
While Lam was serving his UCSF residency, his wife, Melissa, was getting her PhD in social psychology at Berkeley, so they ended up in the San Francisco Bay Area. “This was the rise of the .com era and a new science that was the convergence of technology and medicine,” Lam says. “It was the heyday of nanoscience and nanotechnology.”
Lam moved to Atlanta to work at Emory and Georgia Tech in their combined biomedical engineering research program more than a decade ago. One of the elements that drew him to this academic medicine ecosystem was the culture. “The level of collaboration among different investigators, departments and universities here is unlike anything I’ve seen across the country,” he says.
He decided to start a laboratory that lives in both the department of pediatrics and the department of biomedical engineering, with a footprint on the clinical and technological sides.
“It’s truly a 50/50 split,” he says. “From a basic science standpoint, we study blood and the biophysics of blood, but we’re also a ‘gadget lab’ where we develop new technologies.” A one-stop shop, the lab is home to a versatile group of bioengineers, electrical engineers, mechanical engineers, physicists, biologists and physicians who can take technologies from “basement to bench to bedside” says Lam, or “from PhD project to publication to product.”











Testing the Home Tests
In a fortuitous move, Lam and colleagues from Emory and Georgia Tech saw the need for a diagnostic research center. In 2018, the Atlanta Center for Microsystems Engineered Point-of-Care Technologies (ACME POCT) was established as part of the National Institutes of Health’s (NIH) research network. ACME POCT fosters the development of new tests and technologies used in point-of-care settings.
Most COVID-19 home tests were approved by ACME POCT at Emory, Georgia Tech and Children’s Healthcare of Atlanta.
Most COVID-19 home tests were approved by ACME POCT at Emory, Georgia Tech and Children’s Healthcare of Atlanta.
Before the pandemic, there were only a few such tests commonly used in ERs, pharmacies and people's homes. Glucose monitors and pregnancy tests were some of the well-known tests available over the counter. Once the pandemic hit full force, however, the need for rapid, accurate home testing became paramount. “The NIH saw that Emory, in our unique ecosystem with Children’s Healthcare of Atlanta and Georgia Tech, had the medical know-how, the large patient populations, and the technical capabilities to have a robust center for new point-of-care diagnostic tests,” Lam says.
Emory was poised to play a large part in the effort to bring simple, effective home testing directly to consumers. Specifically, the NIH wanted to dramatically shrink the timeline to develop, test, and market COVID-19 home tests. “And that,” says Lam, “was the incipience of the NIH’s RADx program, which stands for ‘rapid acceleration of diagnostics.’ ”
The lab is home to a versatile group of bioengineers, electrical engineers, mechanical engineers, physicists, biologists and physicians who can take technologies from “basement to bench to bedside”

Stamp of Approval
ACME POCT became the validation center for most technologies the NIH was planning to fund and scale up. “COVID tests you’ve seen when you go to CVS or Target, or that you ordered on Amazon, by and large came through us first for our stamp of approval,” says Lam. The FDA uses Emory data to determine whether a diagnostic technology gets authorization and is made available to the public.
“Our center helped the entire country and world get through the pandemic,” Lam says. “At the same time, our team developed valuable skills.” ACME POCT has now been selected as the RADx Innovation Funnel validation center and received contracts of more than $57 million since 2022 to research diagnostic tests for other diseases as well, such as hepatitis C and mpox.
Prepandemic, Lam says, “no one really thought about the capability to diagnose an infectious disease in their living room. Now I think that’s here to stay,” he says. “The question becomes, how do we apply that paradigm to other diseases?”
Honey, I Shrunk the Technologies
The Lam lab studies, specifically, diseases of the blood such as clotting disorders and sickle cell, which often involve microfluidics or nanotechnology.
“A lot of what goes on in terms of those disease processes happens at this really, really small level, at the single-cell level,” Lam says. “And the only way to study that is to create technologies also at that scale. We can manipulate molecules and provoke or coax certain biological processes to behave in certain ways.”
At the same time, Lam is interested in shrinking very large medical technologies and devices to the point where they become portable.
“When I was a graduate student, one of the first technologies I co-invented was an ear scope that we could attach to the iPhone,” he says. “My son was a toddler and he had a lot of horrible ear infections. Luckily, I was a pediatrician, so I'd prescribe antibiotics and my wife or I would go to CVS down the block and pick them up. One time she said, ‘What does a family without a pediatrician do when they have a kid who has ear infections all the time?’ I said, ‘Well, they go to the ER and usually at night because the symptoms get worse then.’ It made us realize there was a problem that could theoretically be solved.”
The smartphone ear scope inspired Lam’s first company, which he co-founded and then sold to Johnson & Johnson a few years ago.
A Just Society
“So how does discovery happen?” Lam asks. “Frequently it’s through serendipity, but even that requires a community. With the centers I direct, community building is a big part of our ethos.”
The new Center for the Advancement of Diagnostics for a Just Society (ADJUST) is focused on helping underserved populations get equitable access to diagnostic technologies and simplifying the user experience. “What the tech developer thinks is easy to use is probably completely different than what the ultimate end user thinks is easy,” says Lam, the center's director.
Imagine that: A group of medical inventors and innovators focused on weary patients, underserved communities, and harried parents at home with a sick kid in the middle of the night.
Lam is convinced the potential for problem-solving is unlimited if the right questions are posed: “Who are you trying to serve? What problem are you trying to solve? How will you solve it? And if you do solve it in this particular manner, will it be used? Those are the questions we need to be asking.” – Mary Loftus, Designer Peta Westmaas
As seen in Emory Health Digest.
Learn more about Emory:
Emory’s Research Impact
Emory News Center
Emory University