CURING THE UNCURABLE
EMORY’S PHILIP SANTANGELO IS LEADING GROUNDBREAKING MRNA RESEARCH TO TRAIN THE IMMUNE SYSTEM TO FLIP THE SWITCH ON GENES TO FIGHT CANCER AND OTHER DISEASES.
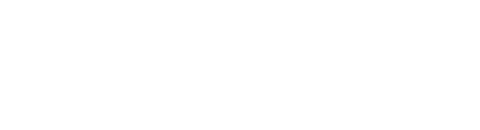
PHILIP SANTANGELO is a risk-taker whose bold scientific ventures often surprise colleagues in his field. But when it comes to the formidable challenge of eradicating cancer and other diseases, boldness is exactly what is needed.
Santangelo, a professor in the Wallace H. Coulter Department of Biomedical Engineering at Emory and Georgia Tech and a researcher at Emory’s Winship Cancer Institute, is taking one of the biggest leaps in current scientific research and doing it with the full support of the federal government. He’s entrusted with $24.8 million in funding over three years from the brand-new Advanced Research Projects Agency for Health (ARPA-H) to push an existing research tool — messenger RNA (mRNA) — in new directions that might lead to treatments for not just a single disease but a whole range of them.
This past August, U.S. President Joe Biden announced that ARPA-H had selected Emory as the first recipient of its funding to support transformative biomedical and health breakthroughs, including the Biden Cancer Moonshot. “Over the past few years, COVID-19 vaccines developed using mRNA technology have saved millions of lives around the world,” Biden said in the announcement. “Now, a skilled team at Emory University in Atlanta will work to adapt these technologies to turn more cancers into curable diseases. This is a bold endeavor that has the potential to transform the fight against cancer and other difficult diagnoses.”
After receiving this landmark funding and support from the White House, Santangelo and his team will focus on using mRNA to develop breakthrough treatments and drugs. “Getting those into clinical trials, really being able to get that out to people, is something that is extremely challenging,” Santangelo says. “Having partners in government, in industry and across the landscape is going to be incredibly important. We can’t do this alone, and that’s why the Cancer Moonshot and the support from the administration is huge — because it’s the only way to fuel this kind of work.”
UNDERSTANDING MRNA’S PROMISE
TO BETTER UNDERSTAND the work of Santangelo and his lab, it is necessary to take a journey back in time. Messenger RNA has always existed, but wasn’t discovered until the 1960s. In fact, mRNA exists in every living cell on earth. It refers to a single strand of the double-helix molecule deoxyribonucleic acid — more popularly known as DNA — that holds the genetic blueprint to determine every characteristic of every organism.
Meanwhile, mRNA — the RNA short for ribonucleic acid — contains all the genetic information in its parent DNA molecule, but does the work of instructing cellular machinery called ribosomes to assemble the building blocks of new proteins. This is why it’s called a messenger.
The scientific breakthroughs from mRNA began in the 1980s, when multiple research teams learned how to engineer specific strands of mRNA in the lab to create individually tailored proteins that stimulated the formation of disease-blocking antibodies. The technology’s big moment came in 2020, when pharmaceutical firm Moderna and the Pfizer / BioNTech partnership used mRNA to create two of the most widely used COVID-19 vaccines at record speed.
Santangelo believes the same precision approach can be used to create new tools that could be used to attack many other afflictions — including a multitude of cancers and autoimmune diseases — that result when the immune system is suppressed or dysregulated.
“When I looked at a lot of different diseases that afflict large numbers of people,” Santangelo says, “one theme that became pretty obvious was that the immune system was not quite doing what we wanted it to do or not doing it as well as we’d like. We wanted to build a molecular toolbox for new drugs that would then allow us to manipulate the immune system in a way that hadn’t been done before and unlock new treatments to cure these diseases.”
That would be an unusually ambitious project for most scientists, who frequently complain that grant-making agencies are only interested in funding research with small, safe, incremental goals. However, ARPA-H, an arm of the National Institutes of Health, was created in 2022 to disrupt that pattern and push the envelope by funding potentially groundbreaking research by scientists such as Santangelo. ARPA-H fully recognizes that the risks are high, but so are the potential rewards.
Santangelo and his team pursue ideas he says others might describe somewhere between “complex” and “crazy.” However, when he applied to ARPA-H for funding, he was confident he had enough preliminary data to back up his gamble. His job is now to prove to ARPA-H and his colleagues that he can do what he said he can do.
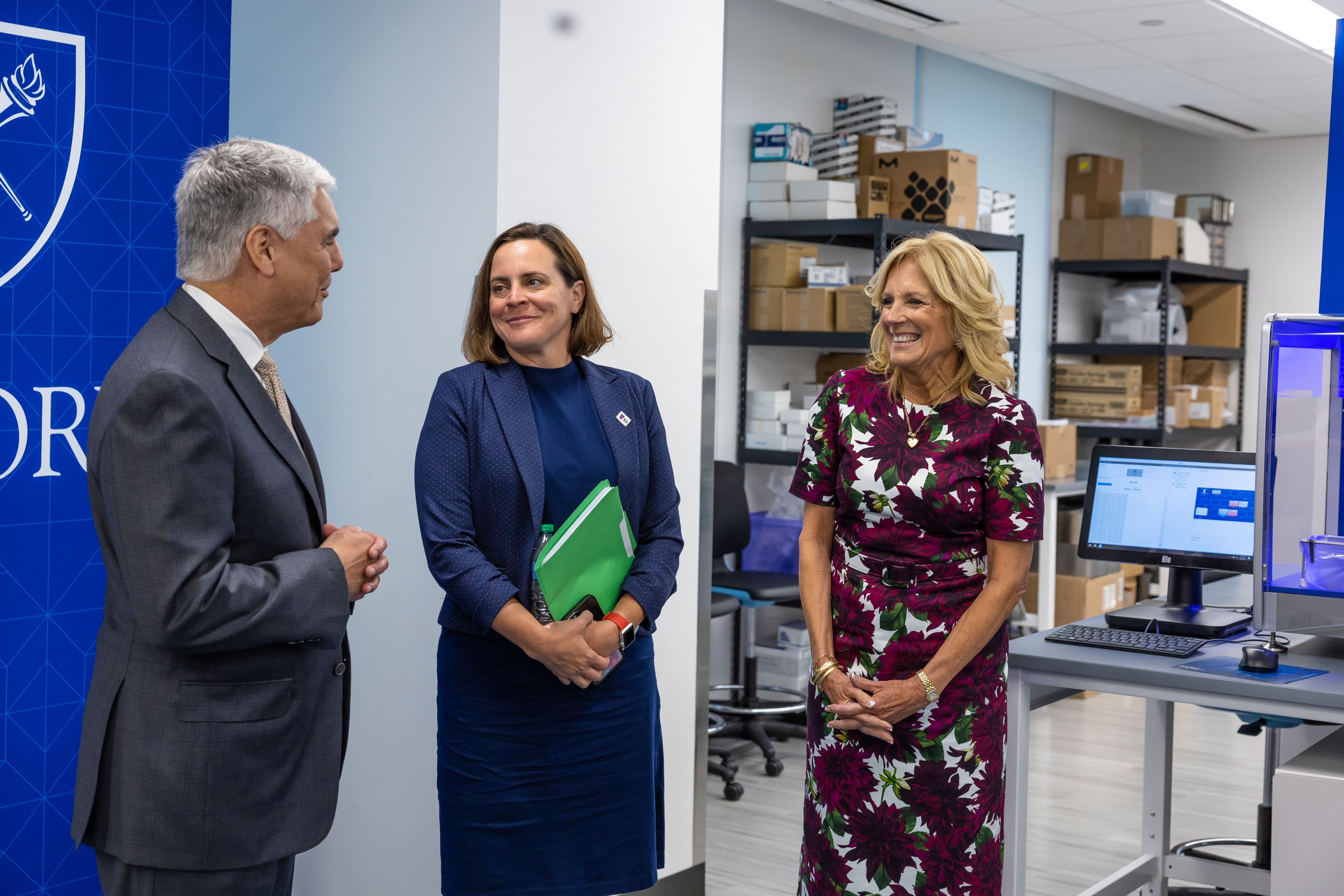
He’s already in the spotlight: Shortly after the agency picked Santangelo as its first recipient, his research drew first lady Jill Biden to Emory in September to tour his lab and learn about his work. “As a mom who watched my son die of cancer, the one thing I never gave up on was hope. As a mother, you can’t,” she said after the tour. “This work gives families the power to hold on to that hope just a little bit longer. Because this work could change lives.”

THE QUEST TO CURE CANCER AND OTHER DISEASES
ARPA-H IS FUNDING Santangelo’s research through an initiative dubbed the cancer moonshot. His project is named CUREIT — short for Curing the Uncurable via RNA-Encoded Immunogene Tuning. CUREIT aims to develop a suite of mRNA tools that can be used to train the immune system to fight disease.
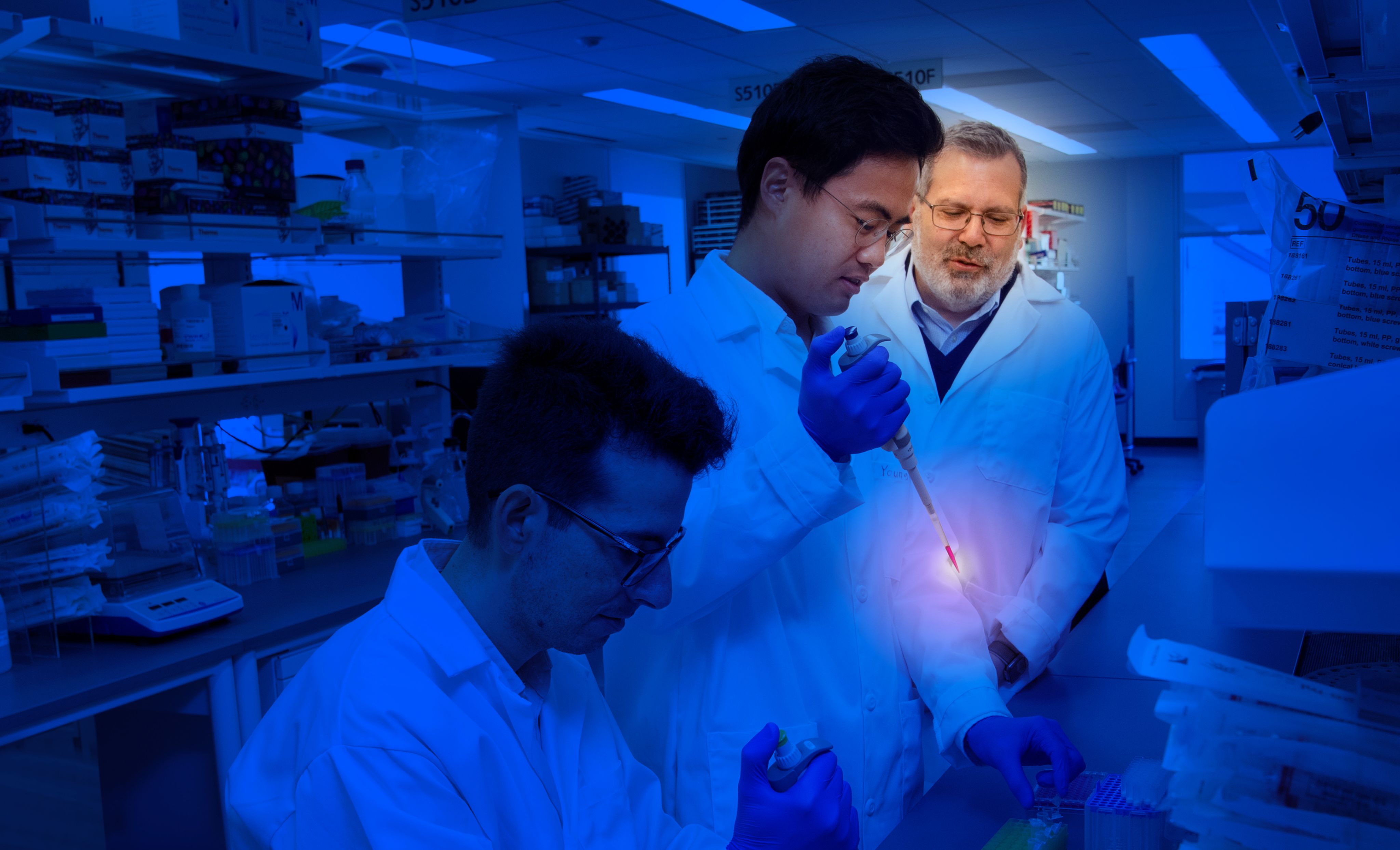
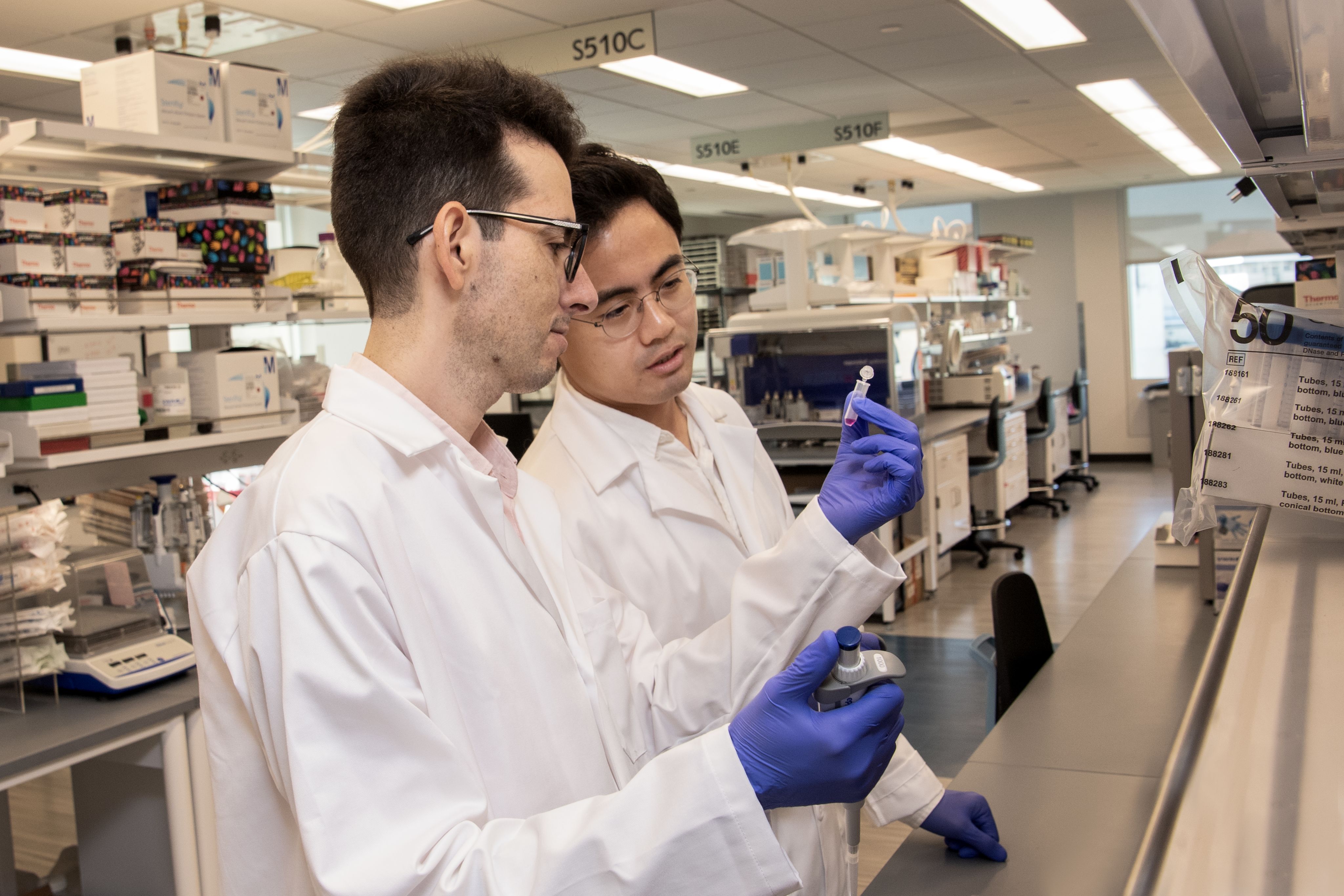
Santangelo will pursue these goals in collaboration with other researchers from Emory, including immunologists, physicians and students, as well as scientists from Yale University, the University of Georgia and the German biotech firm Transimmune. Santangelo’s lab will supply the custom-designed mRNA and formulations.
“We have to screen through literally thousands of different RNAs to see which ones get the response we want,” says immunologist José Assumpção, a postdoctoral researcher and key member of Santangelo’s team. “We can try different combinations. For certain types of cancer, we need a certain type of response. For other types, we need different responses.”
The same variability and specificity is needed when targeting autoimmune and infectious diseases. “I can also modulate these,” Assumpção says.
The project is based on the insight that not just cancer, but many other debilitating ailments as well, have a failure of the immune system at their core. “In the case of cancer and chronic infections,” Santangelo says, “the immune system is essentially suppressed by the disease. We need to be able to reawaken it.”
Because existing approaches to regulating the immune system — via vaccines, antibodies and cell-based therapies — all have problems with cost or effectiveness, it’s necessary to change the immune-regulating model with a completely new system. That’s where Santangelo’s research comes in, aiming to develop a new class of mRNA-driven drugs that can regulate genes in the body’s immune cells — switching them on or off to get the desired response. This approach is independent of disease type and can potentially be used to treat a wide swath of afflictions.

A DEEPER LOOK AT HOW MRNA WORKS
MESSENGER RNA VACCINES are created by engineering molecules of mRNA in the lab that contain genetic instructions to make a piece of the disease-causing virus. When this is administered into the body, it triggers the production of an immune response. Scientists began experimenting with this approach several decades ago, excited by the possibility of being able to custom-design a molecule that could enter a person’s cells and get them to produce exactly the right antigens — the suite of organic molecules immune systems can recognize — that would lead the immune cells to respond and fight a particular disease.
It took years of struggle, false starts, dead ends and slow progress to develop that promise into an effective therapeutic tool.
Researchers first had to learn to manufacture specific kinds of mRNA molecules in the lab, control the natural instability that led them to frequently degrade into other molecules and find a way to encase them in tiny fat droplets known as lipid nanoparticles in order to deliver them to the cell’s interior.
Some of the early research, including Santangelo’s, was backed by the Defense Advanced Research Projects Agency (DARPA), the Pentagon’s own high-risk, high-reward program that served as an inspiration for ARPA-H. Rather than being a specifically targeted medicine, mRNA is a platform — a speedy, plug-and-play approach that could be used to attack other diseases the same way.
Not surprisingly, both established pharmaceutical firms and biotech startups are now seeking to harness mRNA to find ways to teach cells in the body to make their own medicines for both cancer and particularly stubborn infectious diseases such as tuberculosis and malaria. Merck and Moderna, for example, recently began randomized trials of a tunable mRNA drug for melanoma that can be precisely matched to the unique characteristics of tumors affecting individual patients.
Santangelo’s lab has been conducting its own related mRNA research for some time. “We knew the building blocks were there,” he says. “They helped fuel the preliminary work that was needed in order for us to take this next bold step.”

TURNING IMMUNE CELLS INTO SUPERHEROES
“ALL OF OUR DRUGS are similar to the vaccines but not the same in that we use mRNA differently,” Santangelo says. “We use it to express particular molecules that allow us to target specific genes and turn those genes on and off. We’re going to be using this technology to essentially alter the way immune cells function but without changing your DNA. We’re targeting multiple cell types of different parts of the immune system and manipulating how those individual cells function. We can change that function by manipulating multiple genes within those cells. It’s really a layered approach.”
If his research is successful, Santangelo believes it will radically enhance immune response, leading to a technology that can be adapted to multiple diseases — a multipronged approach he thinks will be more productive in the long run. It’s like putting a cape and a Superman insignia on the body’s own cells, he says.
“That’s partly why we can attack different problems,” he adds. “Many of these cell types contribute to different diseases and even help cure them but we haven’t had a good way to manipulate this entire system. We are trying to develop a system approach that allows us to manipulate multiple cell types and multiple genes to get the outcomes that we want.”
Santangelo hopes to be able to develop a platform that’s flexible, effective and safe enough to prove itself in actual drug development and clinical testing. He doesn’t expect to produce drugs in the short run. Instead, he’s picked his first disease targets in collaboration with the Winship Cancer Institute, based on the fact they have reasonable preclinical models that could be built upon. “My goal,” he says, “is that once we demonstrate the platform with preclinical models, we can then apply them to some of the more difficult tumors that are very hard to treat.”
Santangelo says the large grant will let him search for discoveries on a scale that’s not possible in conventionally funded research. He’ll also be able to try approaches that aren’t part of the existing scientific repertoire and have a higher chance of not paying off — but also might result in breakthroughs if they do. “A lot of things we’re going to do aren’t going to work,” he says. “But at the same time, the things that do, we really feel like are going to push the field forward.”
Some might call that risky.
Santangelo sees it as a once-in-a-lifetime opportunity to make big progress that couldn’t be made otherwise in the ongoing fight against cancer.
Or as Emory President Gregory L. Fenves explained after touring Santangelo’s lab with the first lady: “At Emory, it isn’t enough to simply accomplish something great, to reach a goal or earn recognition. We measure our success through lives changed and lives saved.”
Story by Tony Van Witsen. Design by Ruby Katz and Elizabeth Hautau. Photos by Jack Kearse and Emory Photo Video.






9 WAYS MRNA RESEARCH CAN HELP FIGHT DISEASES
In the span of three decades, messenger ribonucleic acid (mRNA) has moved from a promising series of experiments to a breakthrough technology being used in hundreds of labs around the world. Molecules of mRNA can be engineered in labs — like Emory’s Philip Santangelo’s — then introduced into living cells, where they can switch on immune responses needed to attack a particular disease, from COVID-19 to cancer.
Here are nine examples of how researchers are using mRNA to combat diseases:
COVID-19 Vaccines: Perhaps the most widely known application of mRNA technology, these vaccines provide instructions to the immune system to produce a viral spike protein, triggering an immune response without causing the disease itself.
Cancer Immunotherapy
Messenger RNA-based cancer treatments are being researched to instruct the immune system to target specific cancer cells. These treatments can then turn on or turn off genes as needed, potentially enhancing the body’s ability to fight different types of the Big C.
Infectious Diseases
Messenger RNA vaccines could be used to fight other infectious diseases, ranging from influenza to Zika to rabies. The versatility of the mRNA platform allows for rapid vaccine development and adaptation to new variants.
Interference RNA
Known as post-transcriptional gene silencing, this process has emerged as a disease-fighting tool that can stop faulty protein production in cancer cells or attack malfunctioning genes in a range of health conditions.
Rare Genetic Disorders
Messenger RNA technology can potentially be used to correct or compensate for genetic mutations that cause conditions such as cystic fibrosis or certain types of muscular dystrophy.
Autoimmune Diseases
Ongoing research to develop mRNA-based therapies for autoimmune diseases, such as multiple sclerosis and rheumatoid arthritis, aims to modulate the immune response and reduce inflammation.
Inhaled MRNA Medicines
These could reshape treatment of chronic respiratory diseases by delivering therapeutic molecules directly to the lungs, minimizing side effects.
PersonalIzed Medicine
Messenger RNA research has the potential to tailor treatments to an individual’s unique genetic makeup, especially valuable in cancer therapy and rare genetic disorders.
Regenerative Medicine
Researchers are exploring the use of mRNA to promote tissue regeneration and repair in conditions such as heart disease, stroke and neurodegenerative diseases.

Want to know more?
Please visit Emory Magazine, Emory News Center, and Emory University.