A Medical Entomologist Battles Bubonic Plague in Madagascar
Emory University | June 6, 2023

Madagascar is famous for its biodiversity and unique wildlife, especially lemurs. Less well known is that it’s a hot spot for bubonic plague. The island nation off the southeast coast of Africa is one of the last places where large outbreaks of human plague happen regularly.
Adelaide Miarinjara, who grew up in Madagascar, is now a medical entomologist and a postdoctoral fellow at Emory. Her project, unraveling some of the many mysteries surrounding plague, spans the lab of Thomas Gillespie, Emory professor of environmental sciences, and the Pasteur Institute.
“I chose not to study lemurs,” Miarinjara says. “So many people are already doing that. The animals that I work with, rats and fleas, are not nearly as charismatic. But learning about them may lead to better policies to prevent people getting plague.”

"I had to tame my fear of rats," says Miarinjara, shown during an investigation of a plague outbreak.
"I had to tame my fear of rats," says Miarinjara, shown during an investigation of a plague outbreak.
She has done extensive research on the plague bacterium Yersinia pestis and its flea hosts in labs of the Pasteur Institute and the U.S. National Institutes of Health (NIH).
“As a microbiologist, Adelaide is extremely creative,” Gillespie says. “She’s developed whole new protocols for studying fleas that are allowing her to zero in on unanswered questions.”
Miarinjara came to Emory to explore the ecology of plague transmission. The Gillespie lab is a pioneer in the “one health” approach to epidemics — studying the interactions of people, domestic animals, wildlife and ecosystems to understand how germs jump across species.
“The easier route as a scientist is to stay in your lane and work your way up the hierarchy by incrementally increasing what is known,” says Gillespie. “But Adelaide is bold and determined. She realized that to solve the problem of plague she needed to think more broadly.”
Miarinjara also brings the perspective of a Malagasy, as the locals are known, to her research.

Miarinjara was born in the central highlands of Madagascar, but from the time she was 10 years old, she lived in the town of Mahajanga, near the country’s west coast. Her mother, who has a degree in geography, was a high school teacher. Her father, who also has a degree in geography, worked for the World Wildlife Fund and International Conservation and Ecoformation.
“My father is close to nature, and he would try to teach us about it,” Miarinjara says, referring to herself, her older sister and younger brother.
Most of Madagascar’s flora and fauna is found nowhere else on Earth. But the unique ecosystem is critically endangered. About 90% of the country’s original forests are gone, mostly due to slash-and-burn agriculture.
Meanwhile, much of the human population struggles to stay fed, sheltered and alive. The World Bank estimates that 75% of people in Madagascar live on less than $1.90 per day. The country has one of the highest childhood stunting rates in the world, linked to insufficient nutrition and health care as well as poor water and sanitation.

Her father, Jacob Amedée Miarinjara, works in conservation and feels a deep connection to nature.
Her father, Jacob Amedée Miarinjara, works in conservation and feels a deep connection to nature.
Few Malagasy have the luxury of developing a positive connection to nature, Miarinjara says. “We don’t have the time or the money to visit one of our national parks,” she explains. “Even now, I’ve seen very few of those marvelous things that tourists come from all over the world to see in Madagascar.”
Because they lived in a house in town with a yard, her family could cultivate plants for pleasure. “I never saw anyone giving so much care to plants like my father,” Miarinjara recalls. “I remember laughing at him because he would have us go to the coast, about five minutes away, to collect algae and buckets of sea water to put around a young coconut tree he planted.”
Miarinjara and her siblings grew up without computers and video games, but nature provided plenty of excitement.
Their un-air-conditioned home stayed cool because it was topped with a mat of woven palm leaves that kept out the rain but let in the breeze. The children would race to help their father cover the roof with long poles at the approach of tropical cyclones, which can destroy homes and typically displace thousands of Malagasy every year.

"I was a really curious child. I think I drove my parents crazy with my questions," says Miarinjara, shown with her mother, Emma Laurence Mangatiana.
"I was a really curious child. I think I drove my parents crazy with my questions," says Miarinjara, shown with her mother, Emma Laurence Mangatiana.
Locusts swarms also occurred regularly, wiping out rice and maize crops of subsistence farmers. “The sky would become dark, it was so full of them,” Miarinjara says. “The cats would go crazy chasing after them. I was also curious about everything so I would run to catch them too.”
She first heard about plague when she was around 10 years old. During an outbreak, the radio started airing catchy jingles to educate people about how it spreads.
“It was an engaging song, and we kids would run about the yard chanting, ‘Plague, plague, the fleas that are biting you will transmit plague to you,’” Miarinjara says.
“Everything that is out of the ordinary in life is fun when you are a kid,” she adds. “I didn’t think about how the plague, the locusts and the cyclones mean that people are dying and that houses and livelihoods are being destroyed.”

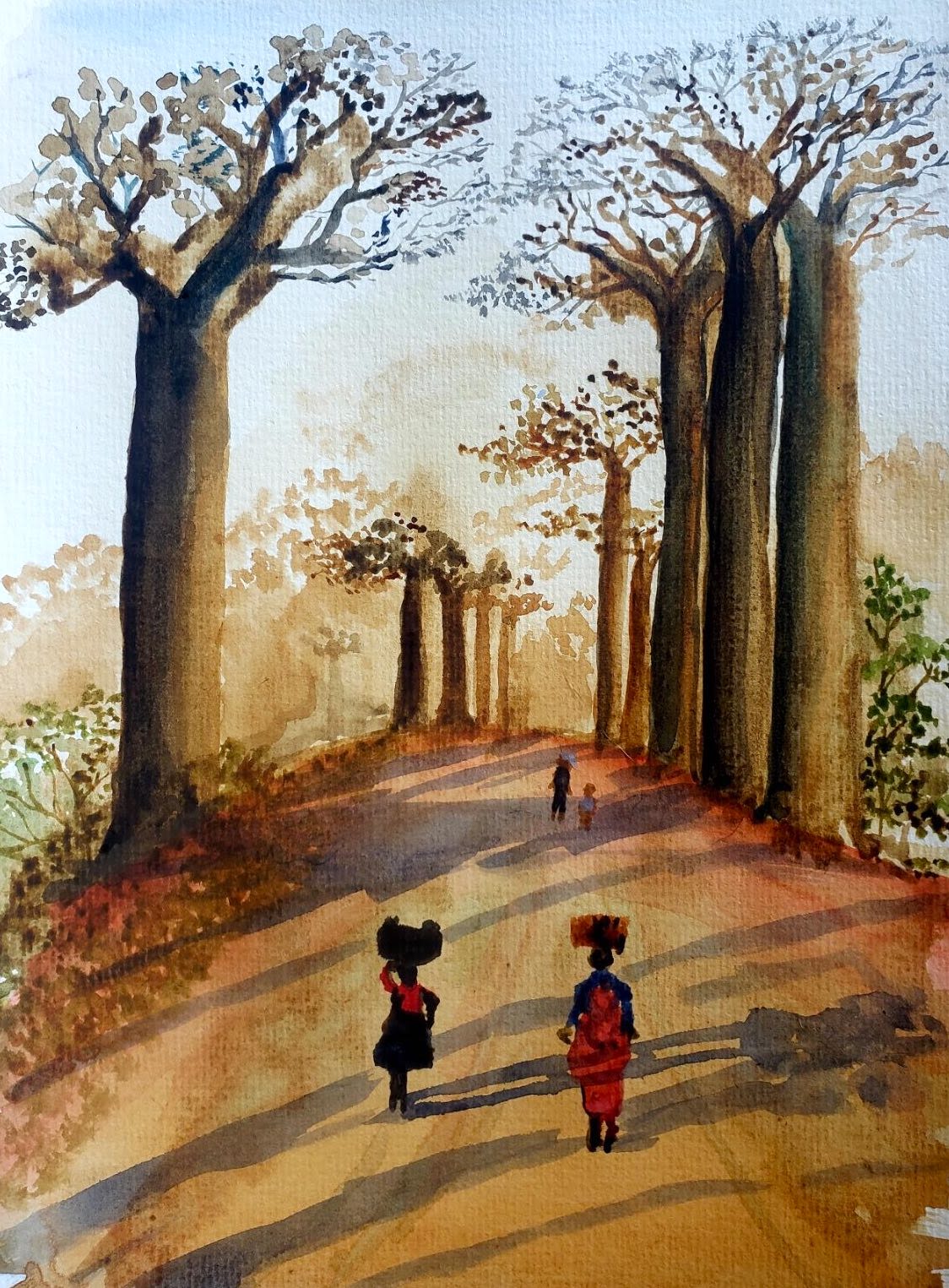


A misty Madagascar morning in watercolor, painted by Miarinjara, who took up art as a hobby in 2019. “I love painting landscapes, not just the natural world but the people living in a landscape and how they are shaping it,” she says.
A misty Madagascar morning in watercolor, painted by Miarinjara, who took up art as a hobby in 2019. “I love painting landscapes, not just the natural world but the people living in a landscape and how they are shaping it,” she says.
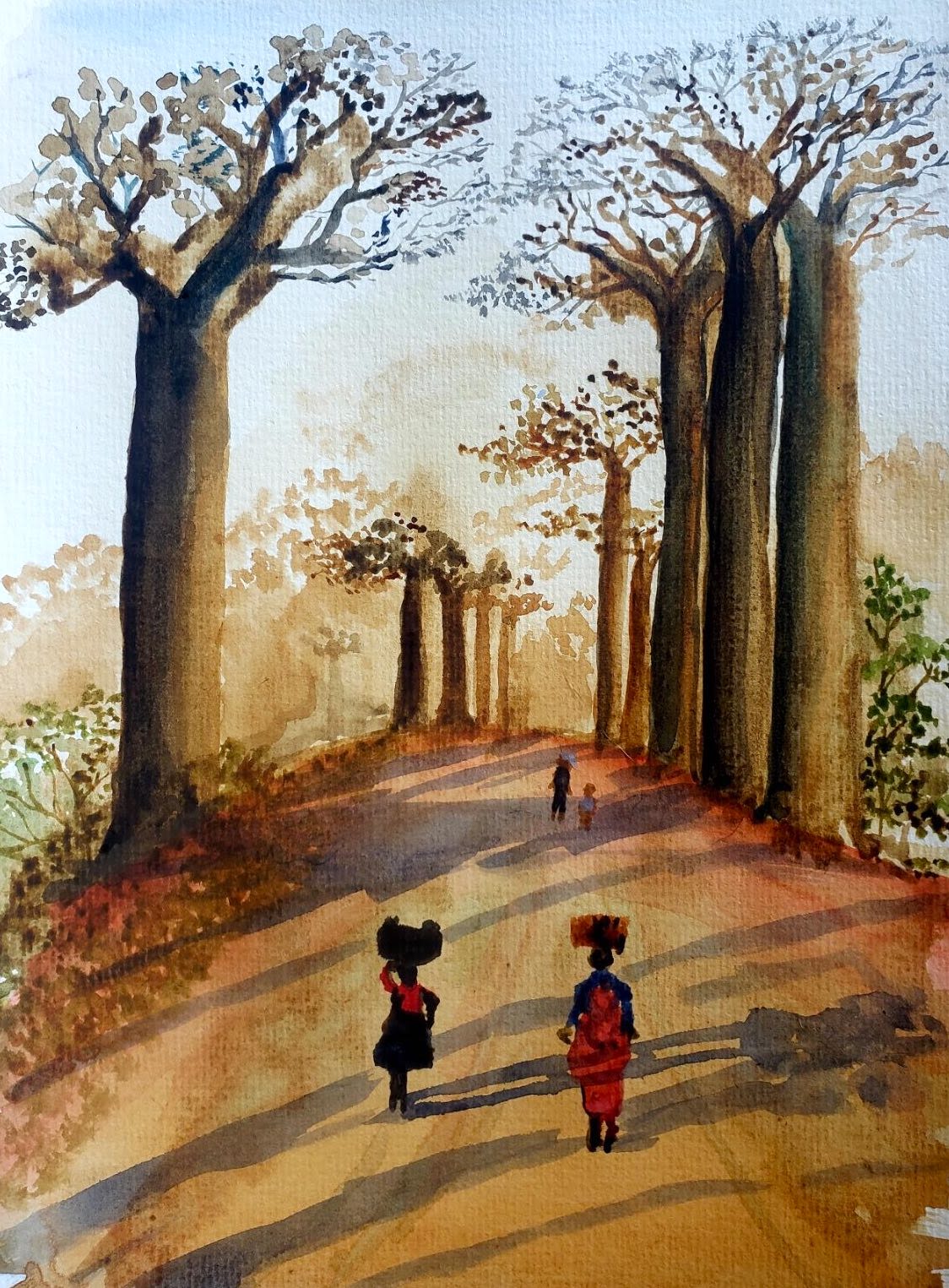
Madagascar's baobab trees are endangered due to the encroachment of agricultural land. "Even though I've painted these trees, I've never gotten to see them for real," Miarinjara says. The local name for the tree, "renala," means "mother of the forest."
Madagascar's baobab trees are endangered due to the encroachment of agricultural land. "Even though I've painted these trees, I've never gotten to see them for real," Miarinjara says. The local name for the tree, "renala," means "mother of the forest."

A rural village scene. "Most of my paintings are done from photos I've taken during fieldwork," Miarinjara says.
A rural village scene. "Most of my paintings are done from photos I've taken during fieldwork," Miarinjara says.
Miarinjara began her higher education in Mahajanga, but when protests shut down the local college for a year, she moved to the University of Antananarivo in the capital. A cousin who is a paleontologist, Sabine Tombomiadana, and her husband, André Raveloson, an entomologist, inspired Miarinjara to get a PhD in medical entomology.
“I was lucky to have them as unofficial mentors,” she says. “In Madagascar, the idea of being a scientist is not very popular and it’s even less popular among girls and women. It helps to have someone that you look up to say, ‘You can do it!’”
While still a graduate student, Miarinjara began working at the Pasteur Institute in Antananarivo. Founded more than a century ago in Paris by Louis Pasteur, the institute is a nonprofit, private foundation studying infectious diseases with branches worldwide, including Madagascar, a former French colony.
Miarinjara’s work at the institute focused on plague.
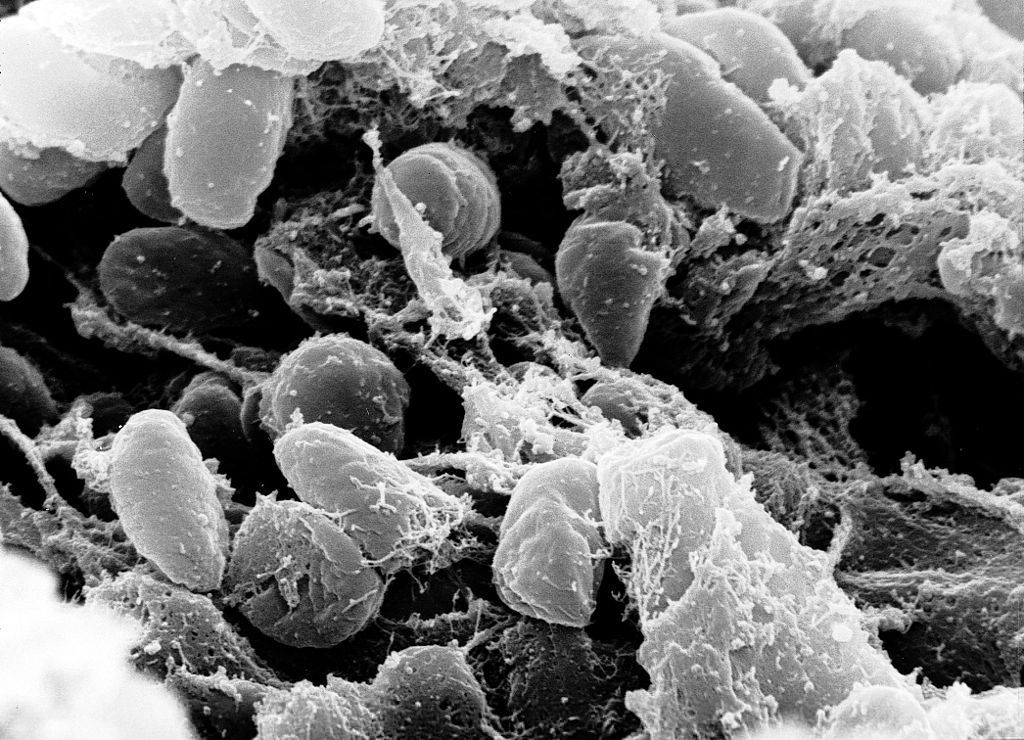
The Yersinia pestis bacterium can infect fleas. When an infected flea bites a mammal, such as a rat or a human, it can pass on the bacterium. In humans it causes bubonic plague — a devastating disease marked by pus-filled swellings on the body, fever, headaches and a high fatality rate if left untreated.
The plague has afflicted humans at least as far back as the Bronze Age and has persisted globally through the centuries. The most well-documented outbreak wiped out one-third of the population in Europe in the 14th century, spawning the term “the Black Death” and iconic images of plague doctors in beaked masks.
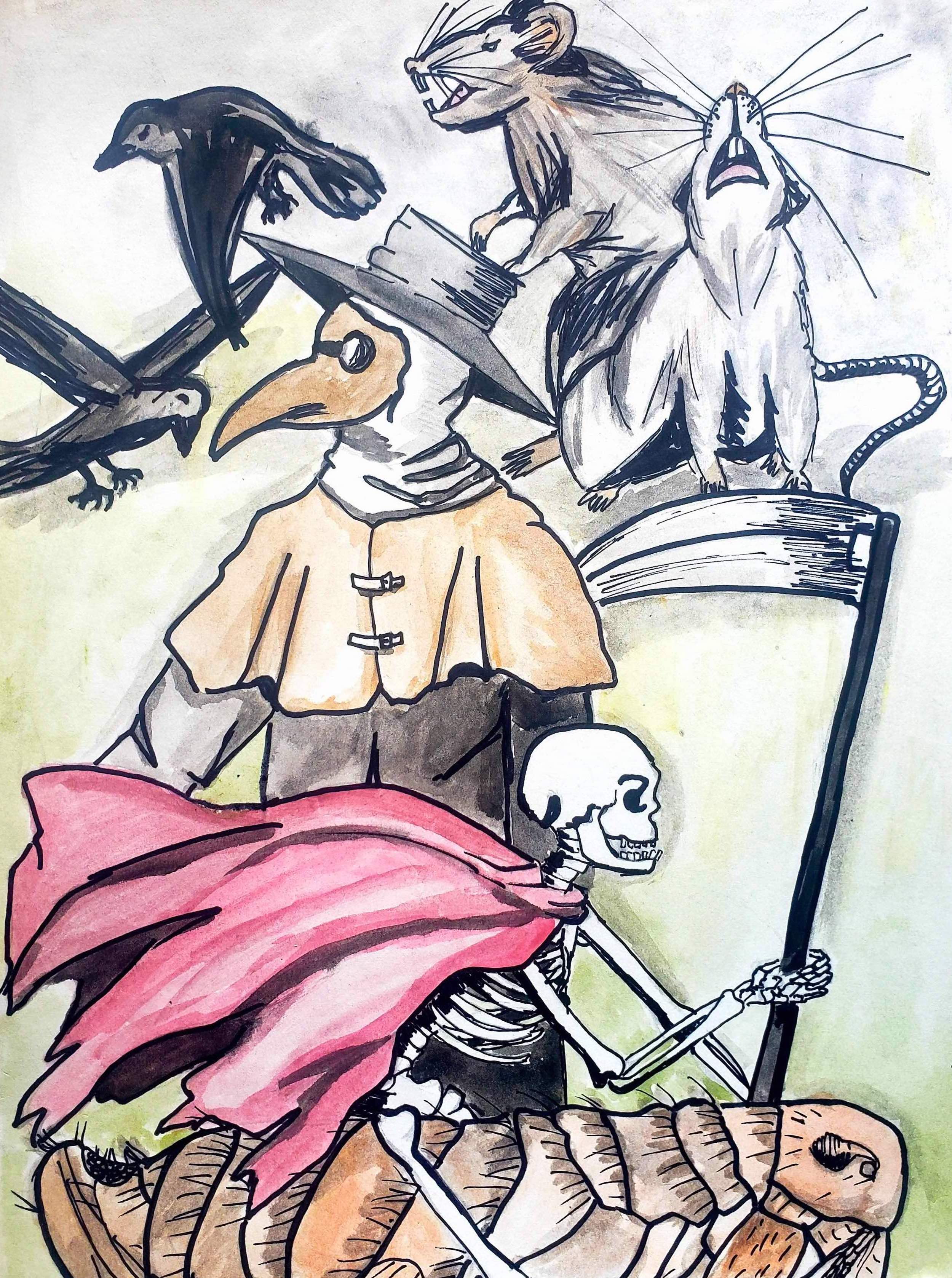
Miarinjara's depiction of iconic plague images from the Middle Ages.
Miarinjara's depiction of iconic plague images from the Middle Ages.
Modern-day health care systems and the advent of antibiotics — which can effectively treat plague — turned the disease into a horror story from the past for much of the world.
In Madagascar, however, plague returns regularly to claim new victims. Cases typically originate in the rural rice-growing region of the central Highlands during the rainy season.
“Plague outbreaks in Madagascar,” Miarinjara explains, “are associated with agriculture, degraded forests and the black rat — an invasive species that is present in people’s homes.”
Bubonic plague is the most common form of the disease. But if the infection goes untreated, it can enter the lungs and morph into pneumonic plague, a more virulent form that can spread through coughing.
In 2017, Madagascar recorded 2,348 confirmed, probable and suspected cases of plague leading to 202 deaths — a case-fatality rate of 8.6%, according to the World Health Organization.





A typical Malagasy house in the countryside. Animals are often kept on the bottom floor.
A typical Malagasy house in the countryside. Animals are often kept on the bottom floor.

Miarinjara, left, and her colleagues. "Every scientist should go into the field," she says. "You need to see with your own eyes what's going on."
Miarinjara, left, and her colleagues. "Every scientist should go into the field," she says. "You need to see with your own eyes what's going on."

Members of a rural community gather to learn about the fieldwork activities of Miarinjara and her colleagues.
Members of a rural community gather to learn about the fieldwork activities of Miarinjara and her colleagues.

Malagasy cattle, known as zebu, are prized livestock.
Malagasy cattle, known as zebu, are prized livestock.
In much of rural Madagascar, people may have to walk for more than a day on an unpaved trail to access the closest hospital. In addition to poverty, lack of infrastructure and health services, cultural considerations make plague difficult to combat.
“It’s very delicate to approach people with a suspected case of plague in their family,” says Miarinjara, who goes into the field to collect biological specimens from fleas, rats and people during an outbreak. “People associate plague with a lack of hygiene so sometimes they feel ashamed. Some people even believe that plague is a curse.”
While many factors are involved in the complex process of plague transmission, Miarinjara’s work is primarily focused on the role of fleas.
“There are 48 species of fleas in Madagascar,” she says, “but only a handful can be found in a human environment.”

Miarinjara brushes the coat of a rat to remove fleas. A colleague uses a glass vacuum tube to suck up the insects, which will be taken to the lab for analysis. (Photo by Soanandrasana Rahelinirina)
Miarinjara brushes the coat of a rat to remove fleas. A colleague uses a glass vacuum tube to suck up the insects, which will be taken to the lab for analysis. (Photo by Soanandrasana Rahelinirina)
Different flea species may feed on a variety of organisms if they are hungry enough, but they have evolved to prefer the blood of one animal over another. Of particular interest to Miarinjara is the so-called “rat flea,” or Xenopsylla cheopis, and the “human flea,” or Pulex irritans.
“Just one bite from one rat flea carrying Yersinia pestis can transfer enough bacteria to infect a rat with plague,” she says. “That makes the rat flea what we call ‘a good vector’ for plague transmission.”
Her research has shown that the human flea can also transmit plague. But it requires several bites from human fleas to spark an infection, making it a less effective vector.
“Pulex is an interesting flea; it’s so abundant,” she says. “You cannot avoid getting bitten by these fleas when you visit most rural households. Personally, my skin is not that sensitive to the bites, but some of my co-workers will be unable to sleep at night due to the itching.”
Miarinjara and her team members take antibiotics before responding to a plague outbreak to prevent becoming infected themselves.
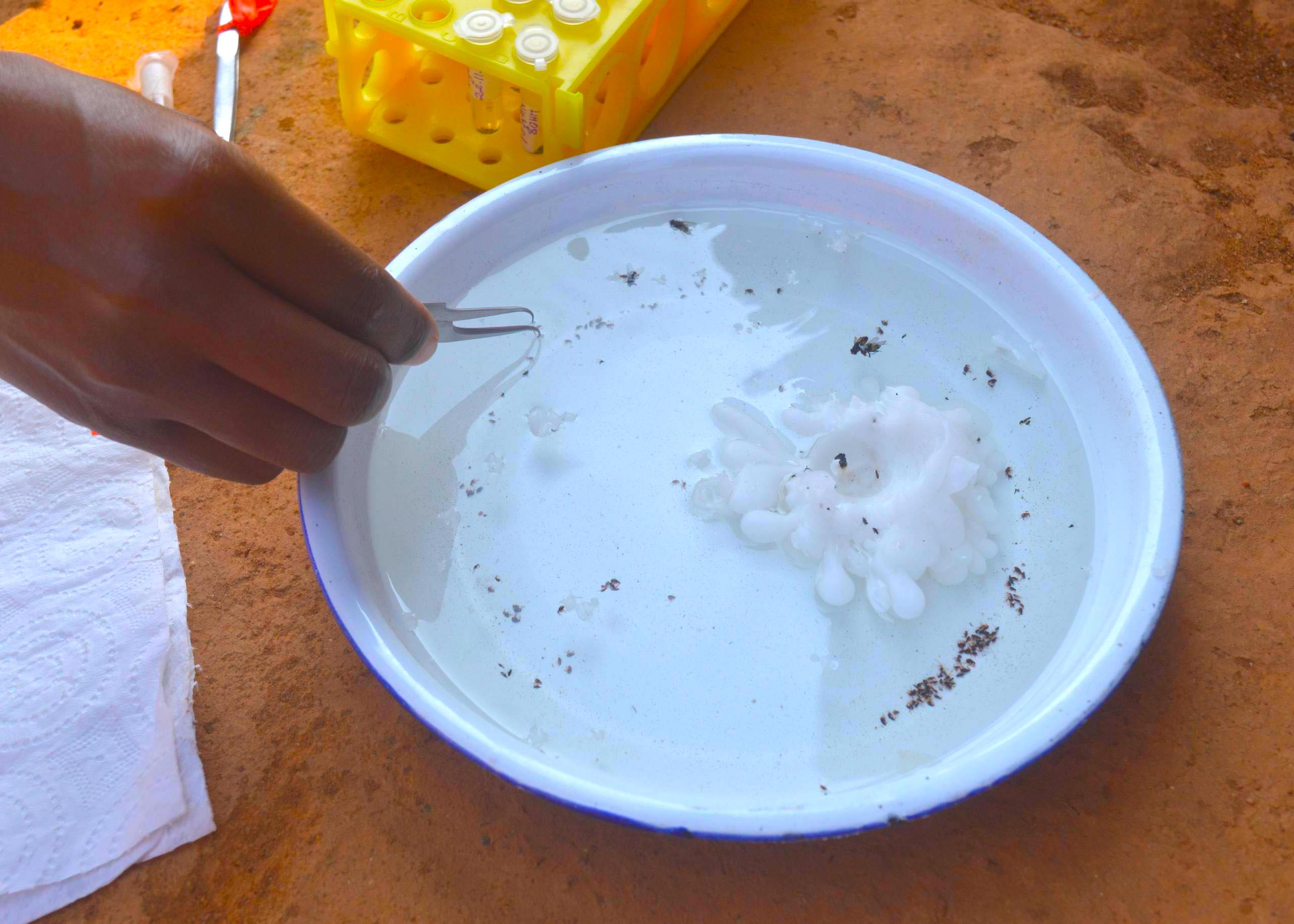
They collect fleas from the rats they trap. They also collect fleas from households using simple traps — a lit candle placed in the middle of a dish of soapy water and set on the floor in the evening.




Invasive rat species are abundant in rice-growing regions.
Invasive rat species are abundant in rice-growing regions.

Preparing rat traps.
Preparing rat traps.

Community members crowd around Miarinjara and a colleague as they count fleas captured in a trap. A single trap may catch 300 fleas overnight, while a trap in another house may catch only 20.
Community members crowd around Miarinjara and a colleague as they count fleas captured in a trap. A single trap may catch 300 fleas overnight, while a trap in another house may catch only 20.
A flea trap consists of a lit candle in the middle of a dish of soapy water that is left on the floor of a home overnight.
A flea trap consists of a lit candle in the middle of a dish of soapy water that is left on the floor of a home overnight.
Miarinjara developed a painstaking technique to get the information she needs from these pesky insects. She slits open a flea abdomen with the tip of a needle and teases out a tissue sample. That sample can then be tested to determine whether it carries the plague bacterium.
It’s also important to learn the species of the fleas which, externally, appear the same. One way to distinguish them is to look at their genitalia. But in addition to being extremely tiny, flea sex organs are internal.
Miarinjara bleaches the dark brown cuticle encasing the fleas until it becomes transparent. Then she uses a microscope to view their sex organs and determine their species, one by one.
“I’ve spent years looking at flea genitalia and I’m still doing it,” she says. “When you know the purpose of what you’re doing, even the most mundane task becomes fascinating. Motivation is everything.”

This male Paractenopsyllus goodmani flea has been bleached so that its internal organs can be viewed. Its genitalia, long but thin, consists of the two hair-like structures curling upward in its lower abdomen.
This male Paractenopsyllus goodmani flea has been bleached so that its internal organs can be viewed. Its genitalia, long but thin, consists of the two hair-like structures curling upward in its lower abdomen.
Determined to expand her knowledge to fight plague in her homeland, Miarinjara traveled to Hamilton, Montana, after getting her PhD to do a postdoctoral fellowship at the NIH’s Rocky Mountain Laboratories. Her mentor was B. Joseph Hinnebusch, chief of the plague section of the NIH Laboratory of Bacteriology, and a leading expert on the interactions between Yersinia pestis and its flea vectors.
Although human cases of plague are rare in the United States, the burden on wildlife in some Western states is significant. Plague infections can wipe out entire populations of prairie dogs. These outbreaks, in turn, lead to fatal infections in animals that prey on the prairie dogs — such as the endangered black-footed ferret, mountain lions and lynx — threatening entire ecosystems.
Miarinjara was bilingual in Malagasy and French but had little experience speaking English when she arrived in the United States.
“Adjusting to doing science in English was the biggest challenge of my life,” she recalls. “My lab mates were wonderful, patient people, but I sometimes felt isolated. Besides struggling with English, I was adjusting to new weather, a new landscape and a new way of life.”
To relieve the stress, she hiked and began to paint scenes from the trail with watercolors, learning from YouTube tutorials.
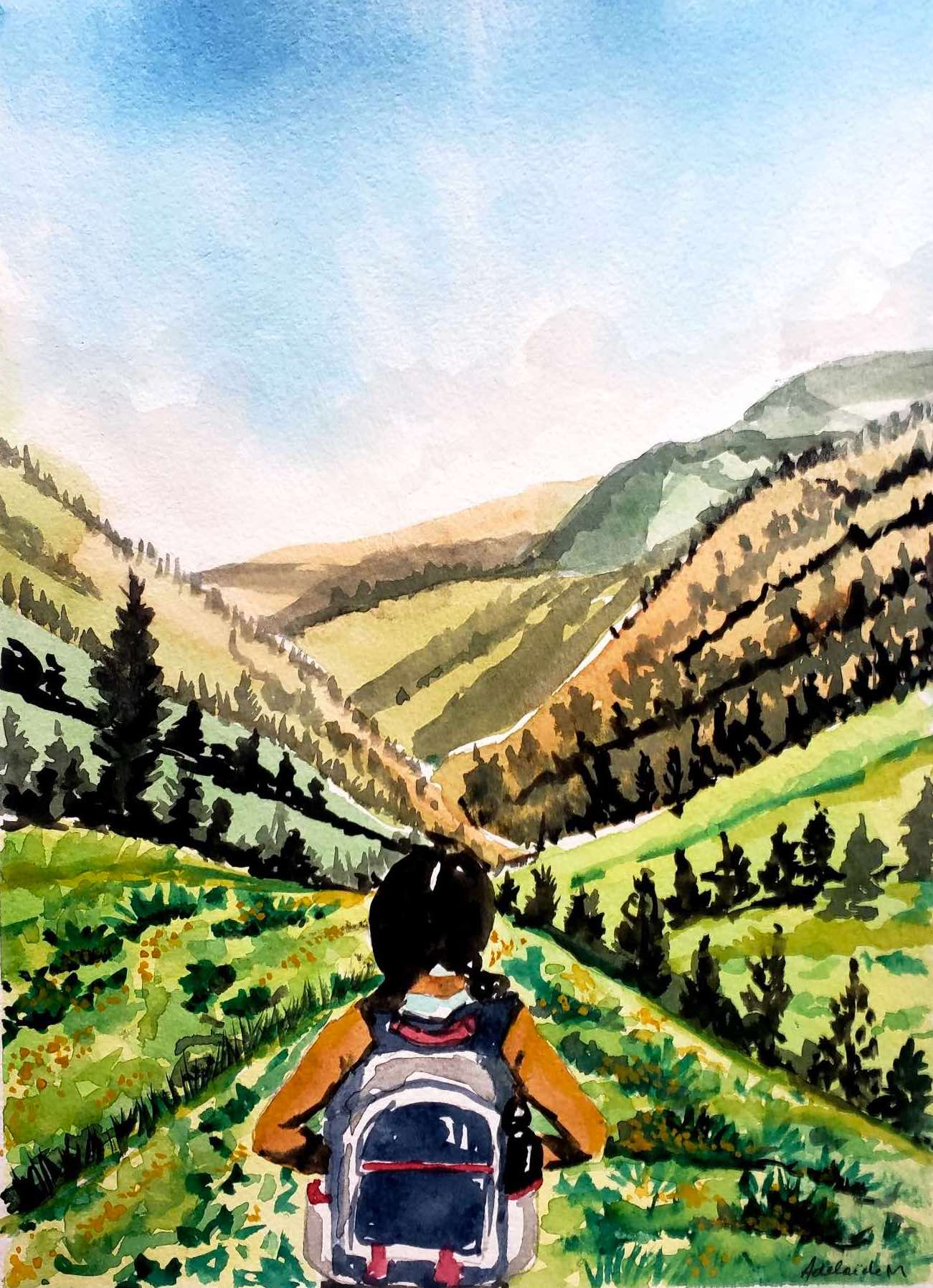
A Montana scene by Miarinjara. She recently sold some of her artwork in an auction to raise funds for Ikala STEM, a program in Madagascar she works with to support girls interested in science, technology, engineering and math.
A Montana scene by Miarinjara. She recently sold some of her artwork in an auction to raise funds for Ikala STEM, a program in Madagascar she works with to support girls interested in science, technology, engineering and math.
Miarinjara came to Emory in 2021 to further expand her research as a postdoctoral fellow. While she continues to investigate the plague bacterium in a bio-secure lab at the Pasteur Institute in Madagascar, at Emory she is developing a “one health” approach.
Gillespie, her Emory mentor, has deep experience in Madagascar. He is among the leadership of Centre ValBio, an international research station collaborating with communities surrounding the World Heritage Site of Ranomafana National Park. Gillespie helped to establish Pivot, a nonprofit incubated by Partners in Health and Centre Valbio, integrating infectious disease research with efforts to strengthen the health system in the region.
“Understanding people’s behavior is out of the scope of entomology, but it’s an important piece of the puzzle of plague in Madagascar,” Miarinjara says.
“There are so many things that we don’t know about plague transmission,” she adds. “The more we learn, the more we can help people to avoid it.”
Her most recent research has shown that a higher number of fleas in rural Madagascar households is associated with having a traditional dirt floor covered by a fiber mat and keeping livestock indoors at night. That knowledge opens the door to potential preventative measures.

A denuded landscape around a Madagascar farm community.
A denuded landscape around a Madagascar farm community.
She hopes to investigate the potential impact of household pesticides. “I was shocked to realize that there is nothing in the scientific literature about the domestic use of pesticides in Madagascar,” she says.
Miarinjara’s research of an ancient plague may also help prevent outbreaks of emerging pathogens.
Most infectious diseases, from plague to COVID-19, can spread from animals to humans, she notes. And shrinking natural habitats boost the risks of germs jumping species.
Gillespie stresses the need for more research into ways to prevent the next pandemic.
“Globally, we’re going to have to deal with the public health effects of environmental degradation, climate change and growing populations,” he says. “Madagascar is just one extreme example.”
Story and design by Carol Clark.
Related Stories:
Madagascar: An Island on the Brink
Valuing Natural Capital Vital to Avoid the Next Pandemic
Media Contact:
Carol Clark, carol.clark@emory.edu, 404-727-0501
Learn more about Emory:
Emory News Center | Emory University