REPLACEMENT (BODY) PARTS
3D-printed anatomical structures are growing in popularity

Heart tissue, joints, tracheas, and knees are just a few body parts that can now be custom-made.
Model Hearts, Bones, and Tracheas
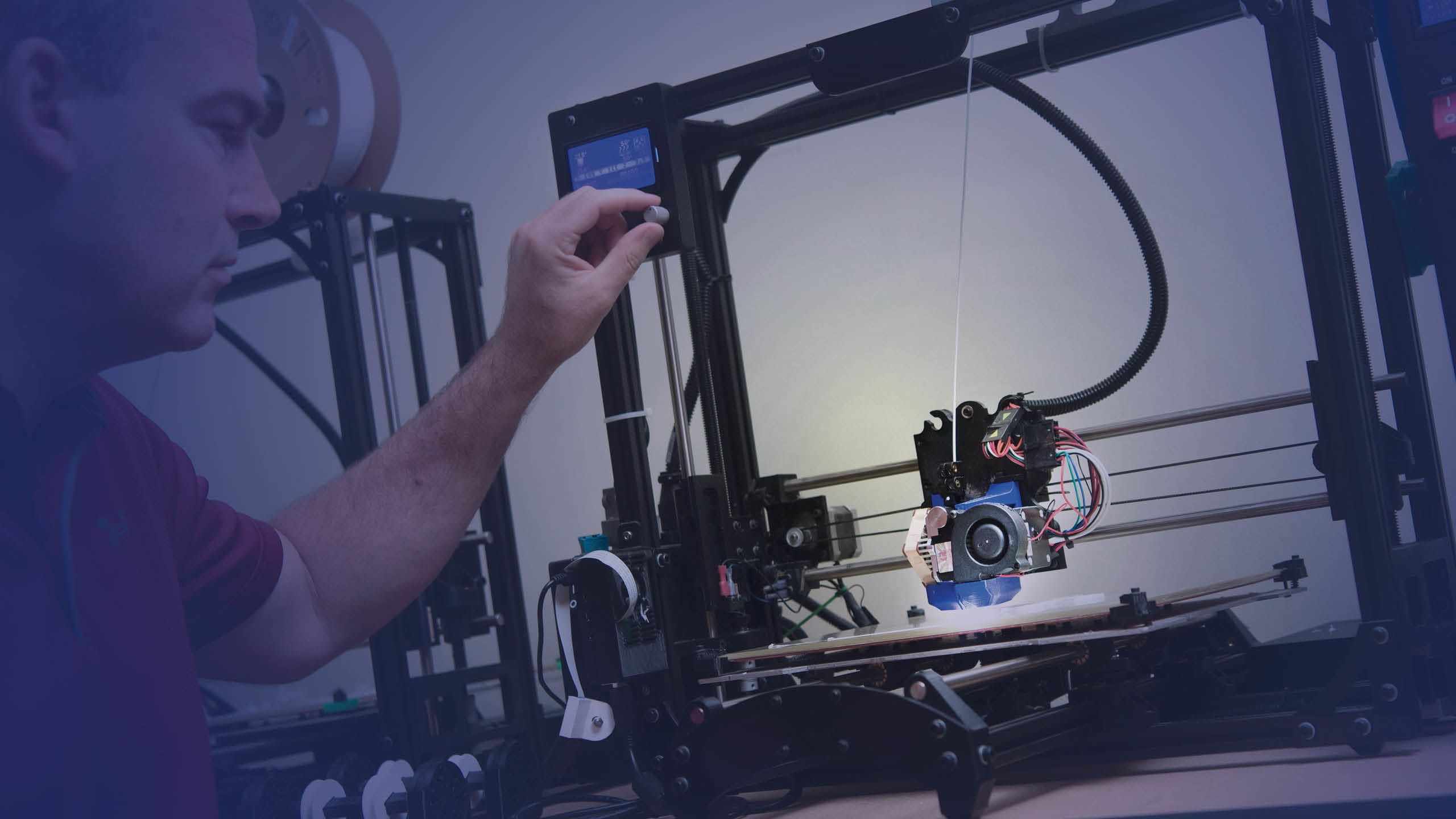
As a medical illustrator, Andy Matlock fuses two worlds that are often seen as dichotomous: science and art. But his work, housed in the Center for Surgical Anatomy and Technique, is critical for educating a new generation of surgeons and medical students. His job? To make intricate anatomical structures leap off the page, literally.
“There’s something you get out of a 3D space, seeing a real model, that you can’t really get from a 2D image,” he says, holding up a 3D-printed heart and pointing out the coronaries wrapping around the organ. Then he opens the heart like a locket, revealing carefully shaped cavities and tiny, flapped valves.
Most of his products end up in the Anatomy Lab and Suture Lab courses, where students can examine the models up close. Using 3D-printed materials helps to reduce the demand for organs harvested from pigs and cadavers. And printed bones, unlike the real thing, can be handled more freely and even taken home for further study.
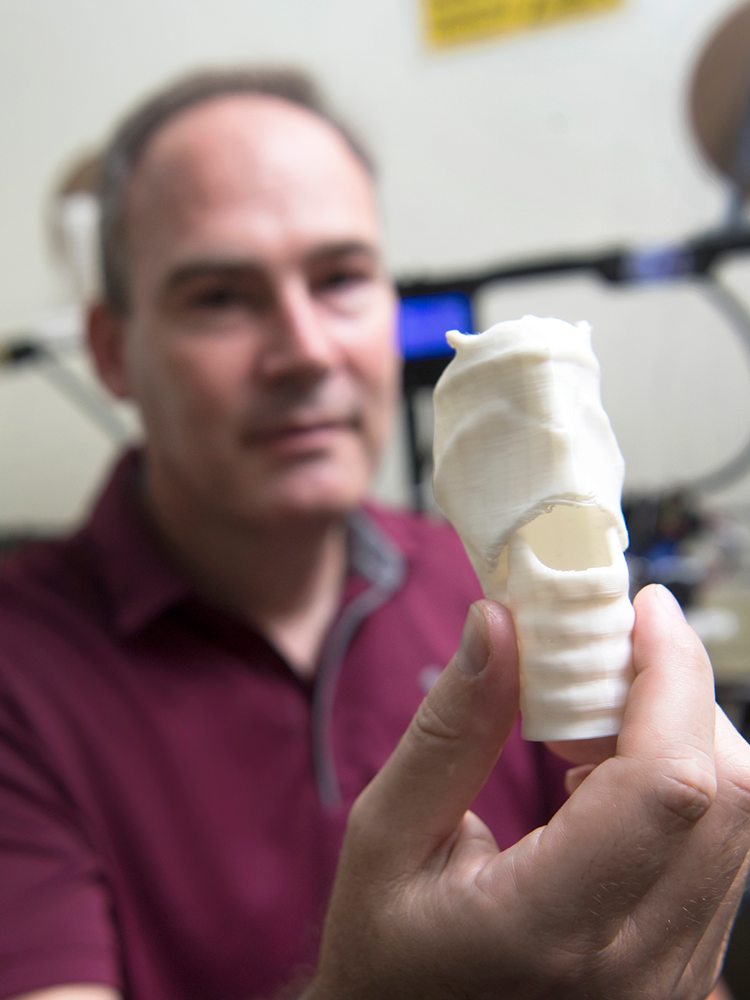
Medical illustrator Andy Matlock holds up a model trachea that was created on a 3D printer.
Medical illustrator Andy Matlock holds up a model trachea that was created on a 3D printer.
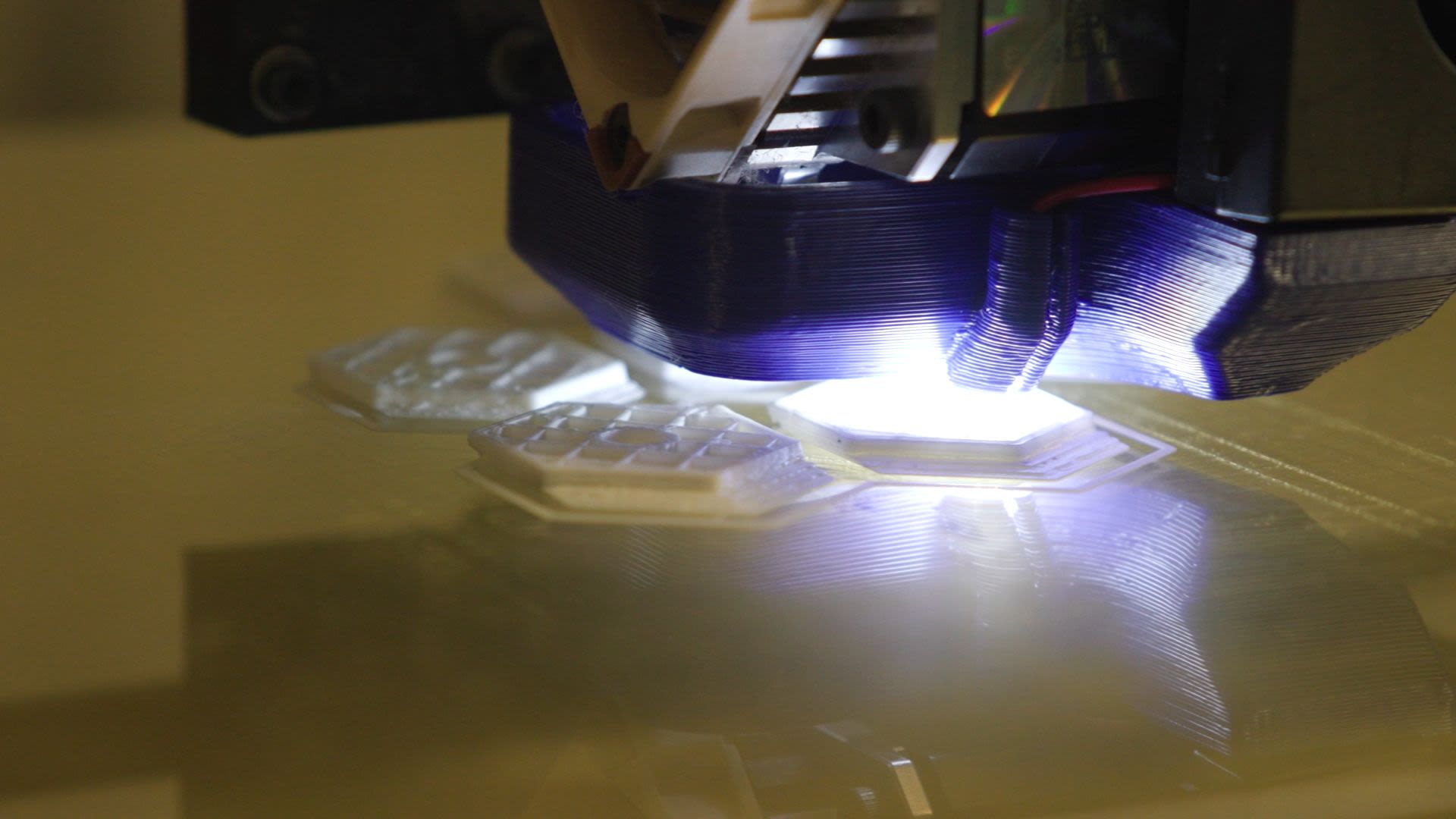
A synthetic trachea, one of his most popular models, allows students to practice tracheostomies. The 3D-printed plastic is covered by a thin silicon skin made of the same material used for special effects gore in movies. Matlock recalls the challenge of building the perfect design for the model—not only did he have to search for a material that could simulate cartilage, he had to maneuver the material through different types of extruders and printer heads. He also built an online blueprint for the model and decided where to incorporate structural supports so the trachea wouldn’t fall apart during the printing process into a “spaghetti of extruded plastic.”
His favorite project modeled a small section of the bronchiole. Using PET/CAT scans from a cancer patient, he created a model that showed precisely where the tumor was in the lung. Surgeons took the model into the operating room and used it as a guide to ensure that they removed the entire mass while preserving as much healthy tissue as possible.
Tissue for Heart Patches
At the Wallace H. Coulter Department of Biomedical Engineering, Martin Tomov builds technologies with an eye toward clinical applications. Using bio-inks, or specialized formulas that can support living cells, he creates realistic tissue replicas that can be used for research or patient care. His job is to “make something that both resembles the tissue in three-dimensional space and has a lot of the functionality of the tissue.”
One project he works on in the Serpooshan Lab is a cardiac patch, complete with blood vessels, that can be applied to a patient’s heart after a heart attack or other major trauma. The patch delivers drugs and provides anatomical support that heals the muscle and prevents further tissue damage.

At the Wallace H. Coulter Department of Biomedical Engineering, Martin Tomov builds technologies with an eye toward clinical applications.
At the Wallace H. Coulter Department of Biomedical Engineering, Martin Tomov builds technologies with an eye toward clinical applications.
“We are really trying to not treat the symptoms, we want to be able to treat the causes,” says Tomov. He highlights the importance of the interdisciplinary nature of the work. “If you focus only on the engineering side, you might lose sight of what you’re actually making and you’ll have this great platform that’s not usable. Or if you’re just looking on the other side, at the clinical aspects, you may come up with a great concept that is still 50 years into the future because we don’t have the engineering capability to create it. Communication between the two sides is very important for the field and that’s what’s going to move it forward faster and more efficiently.”
Pediatric Heart Defects
Assistant Professor of Pediatrics Holly Bauser-Heaton works with 3D models of the heart, specializing in models of pulmonary vein and artery defects. Many children are born with these defects, which often require surgical correction. But Bauer-Heaton noticed a recurring problem: even if the surgery went smoothly, scar tissue would sometimes develop, causing the corrected vein or artery to narrow.
Bauser-Heaton uses 3D-printed models to test whether different surgical techniques, such as tweaking the angle or diameter of a vein, might prevent scarring. “I work with the surgeons a lot with pulmonary artery reconstruction and it’s really challenging when you say, ‘Oh, can you move this a half a millimeter over?’” she says. “They’ll say, ‘No, not really.’ ”
The 3D-printed models allow surgeons to analyze, plan, and test different techniques, all without any risk to the patient. After surgeons have tested a new technique, Bauser-Heaton hooks the 3D-printed models up to a machine that simulates blood flow. By pumping synthetic blood through the models, she can measure the changes in flow patterns, vein stiffness, and dilation. These models are beneficial because they don’t just replicate the anatomical structure of the heart; they also capture cell behavior. The cells in the model can expand, dilate, and react to different environments just like the cells in a person’s heart. This characteristic makes the models ideal for studying pharmaceutical interventions. Bauser-Heaton can make several copies of the same heart, treat them each with a different drug, and see which drug produces the best results in a specific patient.
Bauser-Heaton is meticulous about producing models with realistic textures and consistencies. “We use something called gelatin methacrylate as our ink,” she explains, “We almost make a gummy-bear consistency by using methacrylate to give it structure. Then you’re able to print it in whatever shape you want and alternate the stiffness. I can make it harder or like jelly.” She can add the cells to the ink before the printing process or insert them into the gelatin structure afterward.
Custom Knees
Mathew Pombo, an orthopedic surgeon and director of Emory’s soccer medicine program, uses 3D printers to design custom replacement knees for patients. The technology offers quicker recovery, less blood loss, easier range of motion, and better long-term wear for patients.
“After performing a CT scan, we use an automated design that maps the size and shape of the joint in 3D,” says Pombo, assistant professor of orthopedic surgery at the Emory School of Medicine. “The software allows us to precisely match implants and instrumentation to the model of the knee.”
The unfortunate reality is that all athletes “transition from their prime into the aging athlete category where you can see the impact from a lifetime of sports and activity,” says Pombo, who has performed more than 500 3D knee-implant surgeries. “The patient-specific 3D knee implant is ideal for an aging athlete who suffers from an arthritic knee and is considering surgery.”
Patients’ hospital stays have been reduced by this procedure, which allows surgery to be performed as an outpatient procedure with patients returning home on the same day.
A Stent That Fits
When COVID-19 and a fungal co-infection destroyed part of Judina Taylor’s windpipe, the situation seemed dire. A month after contracting the disease in January 2021, she was still having difficulty breathing, speaking, sleeping, and swallowing. She sought treatment at Emory Hospital Midtown, where pulmonologists Abesh Niroula and Wissam Jaber took on her case.
“When I met Dr. Jaber and the team back in 2021, I felt like I was going to die,” she said, “COVID-19 really took over my body with no remorse. I will never forget Dr. Jaber saying, ‘You fight, we fight!’ ”
But the fight was not easy. Upon seeing that Taylor’s left airway had collapsed, the doctors implanted a stent to help her breathe. There was one problem: the stent didn’t fit.
Traditionally, stents are made to be one size fits all, an approach that works well in straight airways. Taylor’s airway, however, was misshapen from extensive inflammation and scarring. As a result, the stent kept moving out of alignment, creating tiny gaps where bacterial infections could take hold. Every three weeks or so, she would end up in the emergency room, where she would text Jaber, “Hey, I’m here.”
Over the course of the next year, she underwent up to 18 bronchoscopies to clean or replace the ill-fitting stent. Then Niroula had an idea: Why not customize a stent for Taylor?
The physicians uploaded copies of Taylor’s CT scans into software from the Vision Air company based at Cleveland Clinic. The Emory doctors designed the stent, placed the printing order, and within a few weeks, received a stent designed to perfectly fit Taylor’s airway.
In February 2022, Niroula and Jaber implanted the new, custom-made stent. The results were incredible.
Not only did Taylor finally clear the persistent infection that had haunted her for a year, but she experienced significant improvements in breathing, coughing, and sleeping. Eventually she will need surgery, but in the meantime this development has enhanced her quality of life. “Since the placement of the present silicone stent, I have been truly optimistic and 100-percent hopeful about my recovery,” she says.
Repairing an Ankle Joint
After a severe car accident, Natasha Bass wondered if she would ever walk again. With both legs and ankles broken in multiple spots, healing was complex. She developed talar avascular necrosis, which meant her ankle bone was losing blood supply and dying.
She was referred to the Emory Orthopaedics & Spine Center, inside the Emory Musculoskeletal Institute building in Brookhaven. Rishin Kadakia, an orthopedic surgeon, suggested they try a 3D-printed talus implant coupled with an ankle replacement and the surgical fusion of several bones.
In August 2021, Bass received a custom, 3D-printed cobalt chrome talus implant. “I was really excited to have something so new,” she says. “And it was going to give me the best quality of life so I could go back to work and be able to do things I used to do.”

Natasha Bass with the 3D printed talus replacement.
Natasha Bass with the 3D printed talus replacement.
Careful patient selection and counseling is key to 3D-printed implants, says Kadakia: “They are not for every case—but in some instances they can provide an innovative option when there are limited surgical solutions.”
Bass has been dedicated to her rehabilitation and recovery since day one. She’s getting back to visiting her friends and family and taking daily walks. She enjoys riding her bike and being in nature “to have that peaceful time for myself and calm my nerves. Nature makes you realize you’re alive.”
Written by Deanna Altomara, Photography Jack Kearse, Design Peta Westmaas