THE TWO TRAMAS
At the collision point of health and social justice

Healing from Our 'Two Traumas'
Dr. Kevin L. Gilliam II and Dr. Iesha Galloway-Gilliam delivered the 17th annual Hamilton E. Holmes Memorial Lecture on Feb. 17, 2021, part of Emory's commemoration of Black History Month.

When the brutal death of George Floyd stirred national protests in the midst of the COVID-19 pandemic, these alumni physicians found themselves at the collision point of health and social justice.

ON THE LAST SATURDAY IN MAY, after a week in which he helped test dozens of patients for the coronavirus, Kevin L. Gilliam II 09MR, a Family medicine doctor at the NorthPoint Health & Wellness Center in Minneapolis, put his well-trained hands to work at another urgent task. He used a power drill to screw sheets of plywood over the windows of his church.
Gilliam attends Liberty Community Church with his wife, Iesha Galloway-Gilliam 10MR, whose parents co-pastor the Presbyterian congregation. Liberty had received warnings that African American churches in the Twin Cities might be targeted for vandalism or worse.
After George Floyd was killed in police custody on a street in south Minneapolis, the city boiled with protest and burned with anger.
Post offices and a police station were destroyed. Government sources told the church that white supremacist groups were filtering into the city to fan the flames. The congregation didn’t want to take any chances.

A burned-out Minneapolis post office that Kevin Gilliam photographed with his smart phone.
A burned-out Minneapolis post office that Kevin Gilliam photographed with his smart phone.
Gilliam and other members had to finish covering the windows in time to get home before the citywide curfew of 8 p.m. The boards stayed up through most of June.
A memorial to Floyd at the corner of 38th Street and Chicago Avenue, near where he was killed, continued to grow as Black Lives Matter protests spread across the nation.
Tex over media
“That killing shocked us,” Iesha Galloway-Gilliam says. “It was like we were in a house fighting a fire and then a bomb goes off. You can’t hear for a while.”
Being doctors, they use medical terminology to describe the public health emergency and the social uprising that dramatically intersected so close to their home, and then spread across the country. “We think of them,” Gilliam says, “as the two traumas.”
RACISM AND A RUNAWAY VIRUS
At first glance, persistent racism and a runaway virus might not seem related.
But to these two doctors—who did their residencies at Emory, who have spent their careers studying the links between health and poverty, between well-being and ethnicity—the momentous events of 2020 bear a telltale resemblance.
It’s one they’ve learned to recognize, and made efforts to rectify, over the course of their lives and careers.
Galloway-Gilliam decided she wanted to be a doctor when she was six years old. Born in Minneapolis, where her father has roots, she moved with her family to Atlanta at a young age so her parents could pursue their seminary education at the Interdenominational Theological Center. When a younger sister, Iyana, was born with severe, life-threatening jaundice, they took Iesha to visit her in the hospital.
“Iyana had tubes in her head and her arm, and that really made an impression on Iesha,” says their father, the Rev. Ralph Galloway. “She could sense our fear and grief, and she was powerless to do anything about it. She announced right then that she wanted to be a doctor. We thought she’d grow out of it, but she stayed focused.”
Gilliam had a more casual early brush with his future profession. His mother, Jackie Gilliam, worked as a medical assistant and took him to her hospital for bring-your-child-to-work day. Just nine years old, he donned a lab coat and stethoscope. But he didn’t seriously consider medicine until he was in high school and took part in an Upward Bound program at Howard University in Washington, D.C., near his family’s home outside the district in Maryland. “I like working with my hands, and I like teaching, and doctors do both,” he says.
Both were exemplary students in high school, winning scholarships to attend historically Black colleges in the South—Tennessee State University in Nashville for him, Stillman College in Tuscaloosa, Alabama, for her. They went on to the University of Cincinnati College of Medicine, where they met at a picnic with an opening line worthy of a romantic comedy: “He came up to me and said, ‘You’re tall. I like tall girls,’ ” Galloway-Gilliam remembers, “and he had this big smile on his face.”
They began studying together and have been a couple ever since, marrying after they graduated from med school 13 years ago. They did their residencies at Emory, Gilliam in family medicine (2009) and Galloway-Gilliam in internal medicine (2010), splitting their time between various hospitals around Atlanta. The experience that left the deepest mark was at Grady Memorial Hospital, where they came face-to-face with the reality of health care inequalities.
Galloway-Gilliam remembers one patient, an indigent African American woman who had to be hospitalized with pneumonia. “When we sent her home with antibiotics, she started to cry and said, ‘I get medicine? You mean I can have some medicine?’ I’ve never forgotten that. Some people in the United States don’t know what it is to have medicine. That’s the effect of poverty closely tied to racism. I saw that sort of thing day-to-day at Grady.”
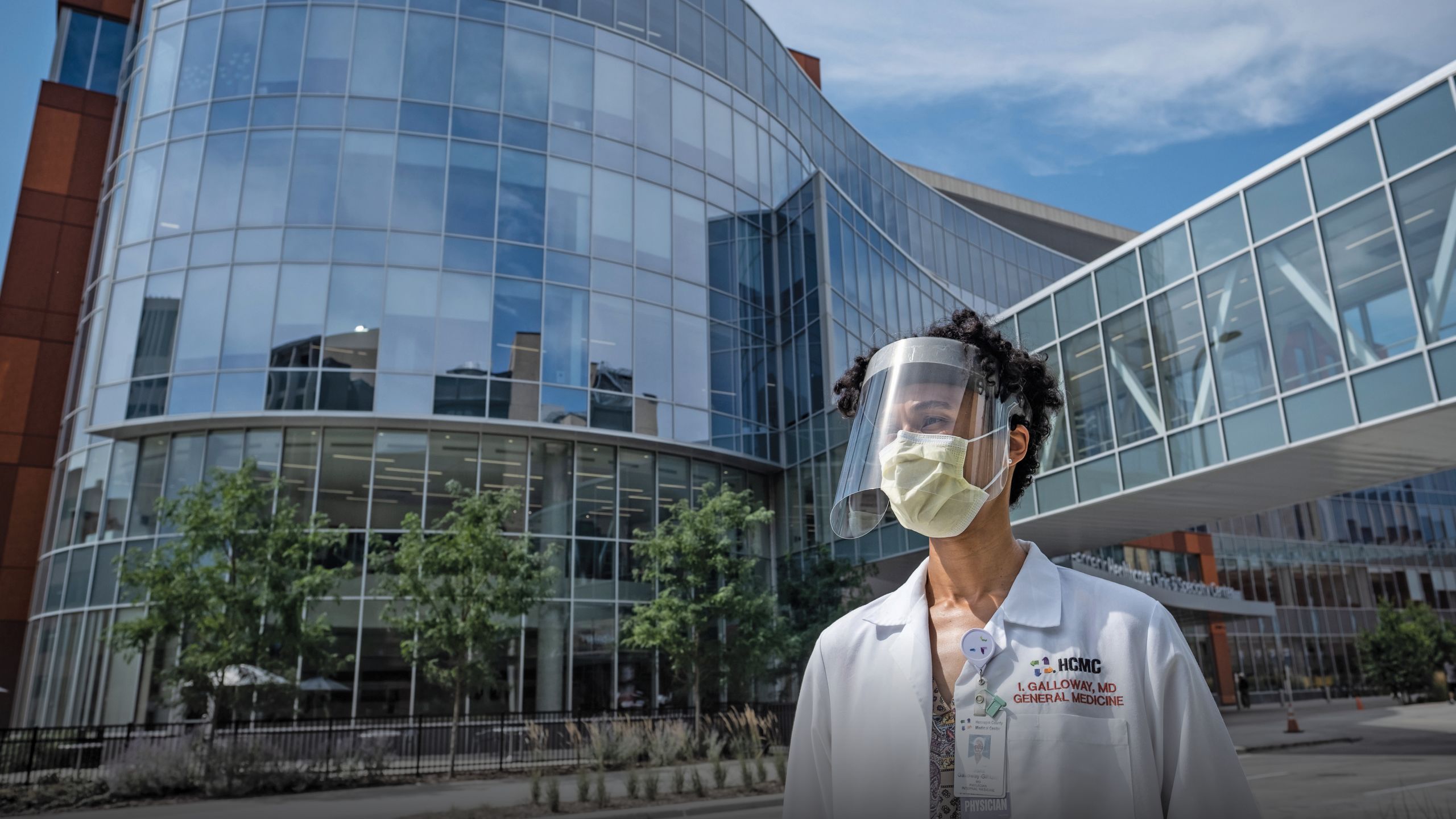
After their residencies, the couple moved to Minneapolis, where Gilliam became a family doctor at NorthPoint, a county clinic that treats mostly minority patients, and Galloway-Gilliam landed a position at Hennepin County Medical Center, a downtown safety-net hospital not unlike Grady. She runs an integrative medicine primary care clinic and is codirector of the Comprehensive Weight Management Center.
They live close to Gilliam’s clinic in a 1926 house on the Near North side. They’re not too far from Galloway-Gilliam’s parents’ church, where Gilliam serves as an elder and they help in outreach ministries. They have an eight-year-old daughter who was in the second grade when the pandemic struck earlier this year, suddenly disrupting their busy lives.
Black Lives Matter protests spread across the country after George Floyd’s death in Minneapolis.
‘WHAT IF WE BOTH GET SICK?’
The physicians had read about pandemics in medical school—especially the gre at influenza of 1918—but now they were living through one as health care professionals in the middle of their careers. It was surreal and frightening when they considered how it could affect their family.
“My nightmare was, what would happen if Kevin and I both got sick?” Galloway-Gilliam says. “You go through loops of panic, and you think of the worst-case scenario. We didn’t want to leave our daughter without us.”
The couple decided to mitigate their risk. Since Gilliam couldn’t avoid seeing COVID-19 patients, Galloway-Gilliam tried to limit her exposure at the hospital, where she teaches residents in addition to her other roles. She still encounters coronavirus patients in other settings but does not work in the viral screening clinic.
Since March, Gilliam has tested patients for the coronavirus twice a week in NorthPoint’s walk-in clinic and in a drive-through testing center set up outside on a parking ramp.
He armors himself in full PPE—scrubs, booties, gloves, gown, N95 respirator covered by a surgical mask, and a face shield. NorthPoint doctors wore masks over their respirators in the early days of the pandemic, when there were shortages of precious N95s and they were trying to reuse them.
“It’s uncomfortable and it’s hot,” he says, “but it’s not different from what I had to wear when I saw some patients at Grady.”
The most unpleasant part of the experience came when the clinic was training nurses to do tests and Gilliam served as a guinea pig, his nasal passages swabbed repeatedly to demonstrate how it was done. His own tests have come back negative, as have Galloway-Gilliam’s.
The pandemic has changed the family’s lives, as it has for millions of Americans.
They haven’t dined inside a restaurant for months, which they really miss, since they consider themselves foodies and once took a pizza tour of Italy. They haven’t been to the movies or the theater. They haven’t attended church services since March, settling for virtual worship. They haven’t socialized with family members for many weeks, except online or through drive-in encounters when Galloway-Gilliam’s parents visit with their granddaughter from their car.
They both turn forty this year and had planned to celebrate Gilliam’s milestone birthday in May with a trip to Hawaii; they settled for a Zoom meeting with family and friends.
“We like to walk, and I like to ride my bicycle,” Gilliam says. “I’ve been taking long rides just thinking about things.”

Drs. Kevin Gilliam and Iesha Galloway-Gilliam bicycle with their daughter through their Minneapolis neighborhood for some stress-reducing family time.
Drs. Kevin Gilliam and Iesha Galloway-Gilliam bicycle with their daughter through their Minneapolis neighborhood for some stress-reducing family time.
No one in their family has contracted COVID-19, but they know many friends and church members who have been touched by the virus. They are not the least bit surprised that the pandemic has affected communities of color disproportionately.
CDC statistics show that the infection rate for African Americans and Latinos is triple what it is for white Americans, a disparity they see among patients in Minneapolis. It fits an old pattern in which minorities are more affected by diabetes, hypertension, asthma, and many other afflictions related to environment and poverty.
“Social constructs often affect health,” Gilliam says. “The more we’ve practiced medicine, the more we’ve come to see that these chronic conditions are related to inequalities.”
STAGES OF GRIEF
On the evening of Memorial Day, a convenience store employee in south Minneapolis phoned 911 to report a man he suspected of buying cigarettes with a counterfeit $20 bill. Police responded quickly. Seventeen minutes later, the man lay unresponsive on the pavement. George Floyd, 46, was pronounced dead at Hennepin—the hospital where Iesha Galloway-Gilliam works. An autopsy showed that he was positive for the coronavirus.
Galloway-Gilliam was on vacation that week, sheltering at home, and didn’t hear about the incident until the following day. She couldn’t bring herself to watch the graphic videos of Officer Derek Chauvin pressing his knee into Floyd’s neck for an extended period of time, bearing down as he pleaded and repeated, “I can’t breathe.”
“Watching that would not have been good for my mental health,” says Galloway-Gilliam. She did see the still photos from the encounter: “As a physician, I know what death looks like, and I was viewing a dead man.”

For months after George Floyd's death, people came to this makeshift memorial to leave flowers, signs, and cards under a mural of Floyd near the spot where he was killed.
‘NOT AN EASY TIME’
They were appalled but not surprised. Though African Americans make up less than 20% of Minneapolis’s population, police records show that they are much more likely to be pulled over on the roads, arrested, or subjected to force than white residents. A number of fatal police shootings have occurred in the Twin Cities in recent years, making martyrs of African Americans such as Jamar Clark and Philando Castile and feeding the rise of the Black Lives Matter movement.
During the protests and disturbances that followed the Floyd killing, Gilliam’s parents in Maryland worried about the safety of their sons and families.
Text over media
“It was not an easy time for us,” says Gilliam’s father, Kevin Gilliam I. “Both our sons are young Black males, and they have to be careful. I’ve always told them if the police pull them over, they need to roll down the windows, put their ID out where it can be seen, and keep their hands on the steering wheel.”

Gilliam assured his parents that they were safe, but in truth, they were profoundly unsettled.
“We wanted to get out in the community and protest,” Galloway-Gilliam says, “but we had to weigh doing that in the middle of a pandemic. We’re doctors and parents, and we didn’t want to be getting out in those crowds and putting our daughter or our patients at risk. We went through a lot of inner turmoil about it.”
As the protests spread and sometimes got out of hand, looting and violence struck the West Broadway commercial district near the family’s home.
They had to explain to their daughter why businesses were burned out or had smashed glass and why their church windows were covered with plywood. Gilliam’s clinic was boarded up as well because it was considered a possible target as a county facility.
While they ultimately decided not to attend the protests in person, many of their fellow church members did, including Iesha’s parents, both in their sixties, who drove as close to the action as they could and cheered from their cars. Gilliam drove past the scenes of the disturbances and took pictures with his cell phone, texting a snapshot of a gutted Minneapolis post office to a friend in Texas.
Wayne Baudy 03MPH, an administrator and physician at Houston Methodist Hospital, attended college with Gilliam at Tennessee State and then earned a master’s of public health at Emory.
“There’s a group of us from college who have stayed close, and Kevin is sort of our elder statesman, the one we reach out to when we need to talk,” Baudy says. “This time he was reaching out to me. He sounded burned out and a little sad. It didn’t seem like him. I think he was going through the stages of grief.”
HOLISTIC MEDICINE
Since the pandemic started, Gilliam has been speaking about the virus at online community meetings. In the sessions held after the George Floyd killing, he found himself speaking less about guarding against respiratory infection and more about the psychic and physical burdens of racism. He found it easy to pivot from one trauma to another because he and his wife believe in a holistic approach to integrative medicine.

Drs. Kevin Gilliam and Iesha Galloway-Gilliam met at a picnic during medical school, and began studying together. They both did their residencies at Emory, Gilliam in family medicine and Galloway-Gilliam in internal medicine.
Drs. Kevin Gilliam and Iesha Galloway-Gilliam met at a picnic during medical school, and began studying together. They both did their residencies at Emory, Gilliam in family medicine and Galloway-Gilliam in internal medicine.
“We both work in the middle of underserved communities and realize that the answers to our problems are often found beyond what we learned in medical school,” he says. “In thinking about how we can be more impactful, we felt that something was missing. We as doctors often separate the physical body from the mind and the spiritual, and they’re quite integrally connected.”
In addition to his work at the clinic, Gilliam has decided to pursue a master’s of divinity at Luther Seminary, a Lutheran institution across the Mississippi River in St. Paul.
He isn’t sure exactly what he’ll do with a theological degree, but he believes it could be critical in ministering to the greater wellness of the community he and his wife have committed themselves to serving.
LOOK FOR THE HEALERS
Dealing with disease and social injustice have deepened their religious faith.
None of this surprises Galloway-Gilliam’s mother, the Rev. Alika Galloway. “Most of what Jesus did was heal,” she says. “Churches talk a lot about heaven and hell, but Jesus didn’t really talk about them that much. Mostly he gathered people together, taught them, and healed them.
“That’s who they are,” she adds. “That’s who we all are: healers.”
By Jim Auchmutey, Photos Caroline Yang, Design Peta Westmaas
Learn more:
Emory Medicine Magazine | Emory News Center |Emory University