MAN ON FIRE
Jalen Richardson survived a fiery motorcycle crash. Then came the hard part.

SEPT. 4, 2016 By all predictions, Atlanta’s long Labor Day weekend was going to be a scorcher, with temperatures soaring toward the 90s and air that hung swampy and still, offering little promise of relief.
To Jalen Richardson, it didn’t matter. He knew how to create his own breeze.

Even as he left his shift at UPS that warm Sunday afternoon, Richardson was mentally mapping his ride—a quick cruise downtown to grab a burger at The Varsity before rolling east toward Atlanta’s Edgewood neighborhood.
Pulling on protective gloves, his helmet and a heavy, padded jacket, Richardson knew his first stop would be to meet up with friends at the QuikTrip near Interstate 20 and Panola Road in Lithonia, a popular spot with local riders.

Jalen Richardson was 18 when he bought his first motorcycle, quickly graduating to a super sport bike. His Suzuki GSX was a powerful machine — sleek, agile and quick.
Jalen Richardson was 18 when he bought his first motorcycle, quickly graduating to a super sport bike. His Suzuki GSX was a powerful machine — sleek, agile and quick.
Richardson was 18 when he bought his first motorcycle. It was small, salvaged from a local flea market, but he loved everything about it—the ease, the power, the way a bike could mirror your every move. It was man and machine working as one, a heart-pounding sense of freedom that, short of sprouting wings, was the closest he could come to flying.
The following year, he graduated to a bigger, faster ride: a flashy blue-and-white 2003 Suzuki GSX. Weighing around 350 pounds, it was a powerful machine—sleek, agile, and quick.

Richardson enjoyed meeting up with his riding group — a handful friends who cruised around Atlanta several times a week.
It had taken time to find his riding group, a handful of guys in their 20s who cruised around metro Atlanta together two, three times a week. As they fueled up that evening, a larger pack of bikers rumbled into the gas station, opting to tag along with Richardson’s crew. More than a dozen bikes strong, the riders merged onto Highway I-20 heading west. Richardson found his place between the two groups, his friends pulling ahead, the others trailing just behind.
No one knows where the Kawasaki EX-250 came from—an outsider, wedging his way into the pack. Traffic was slowing near the Wesley Chapel Road exit when the Kawasaki suddenly darted behind Richardson, striking his back tire.
The shuddering impact was abrupt and violent, instantly toppling the heavy Suzuki and Richardson with it. Hitting the asphalt hard, his right hand reflexively squeezed the throttle, sending the engine screaming and wheels spinning even faster. Body and bike skidded down the highway in a fiery shower of sparks.
For Richardson, a Georgia Army National Guardsman in top physical condition, the moment played out simultaneously at high-speed and in slow-motion. Driven by a monster surge of adrenaline, he fought to free the left side of his body, now pinned under the full weight of his bike. He didn’t know his gas tank was punctured or notice the long, oily streak of fuel smeared behind him, a dark, combustible stain on the pavement.
Hearing a boom, his friends turned back to gasp at the resulting explosion—a flaming mushroom cloud that grazed traffic signs 20 feet above the highway.

Hearing a boom, riders looked back to witness a fiery explosion; somewhere deep within the inferno was Richardson. A witness captured this cell phone image.
Somewhere within the inferno was Richardson.
Blown from his bike, he felt himself fall hard against the pavement. There was no awareness of being engulfed by fire, only the roar of a hard, driving wind. Within moments, Richardson was the epicenter of a sudden clamor, as panicky motorists doused him with bottles of water and Big Gulps, tossing a blanket over his smoldering riding gear.
Hearing low, guttural groans—like an old man trying to get out of bed, he thought—Richardson slowly realized the sounds were coming from him.
Against the protests of bystanders Richardson tried rising to his hands and knees, unable to comprehend how badly he was hurt. The flames had seared his gasoline-soaked left arm so quickly, so deeply, the blood supply to his muscles was already restricted, leaving his fingers numb and tingling.
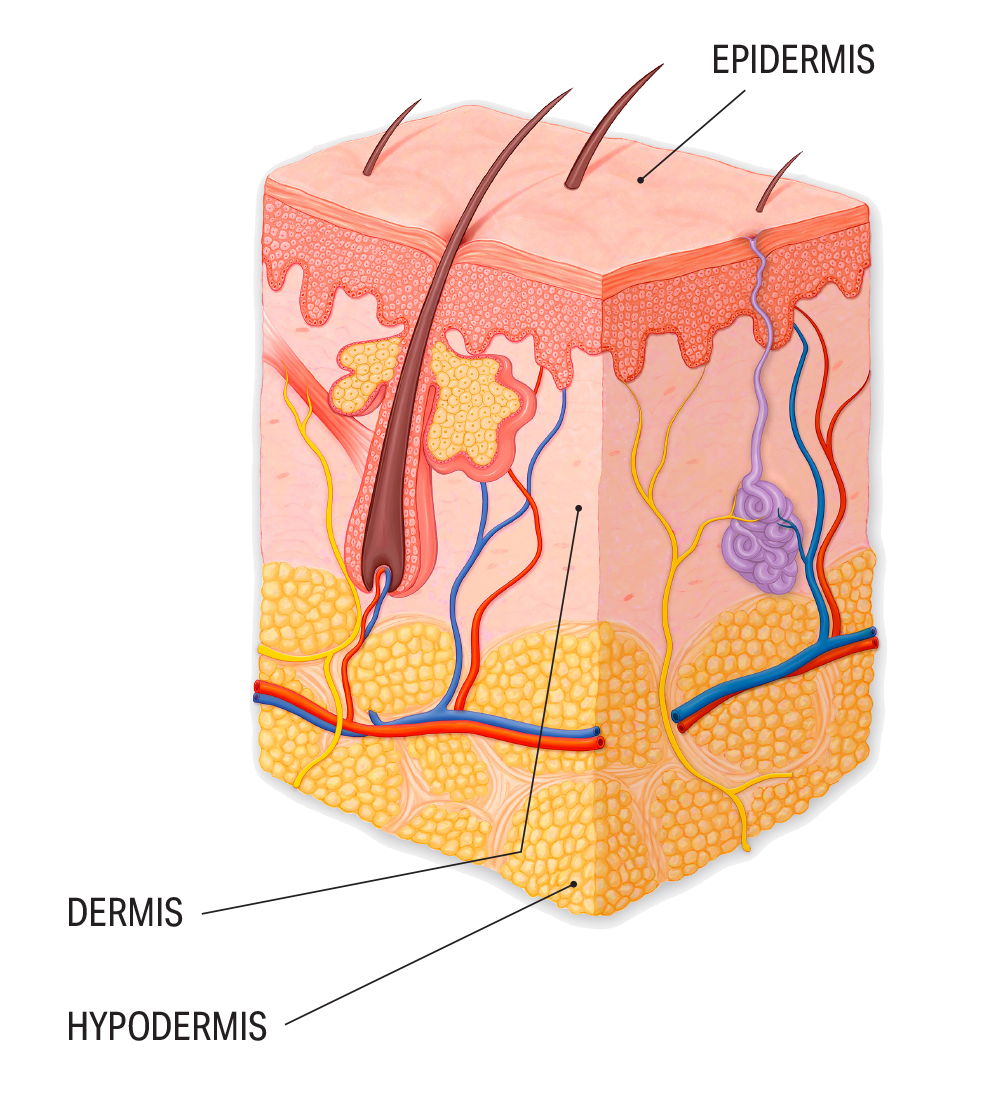
Softened by industrial-strength heat, the top of his motorcycle helmet was melting, collapsing like a soufflé. Strangely, he felt almost no pain—many of the superficial nerve endings that laced his dermis had been incinerated.
In fact, an astonishing amount of his skin was simply gone.

Richardson enjoyed meeting up with his riding group — a handful friends who cruised around Atlanta several times a week.
Richardson enjoyed meeting up with his riding group — a handful friends who cruised around Atlanta several times a week.

Hearing a boom, riders looked back to witness a fiery explosion; somewhere deep within the inferno was Richardson. A witness captured this cell phone image.
Hearing a boom, riders looked back to witness a fiery explosion; somewhere deep within the inferno was Richardson. A witness captured this cell phone image.
‘MELTED TO THE ASPHALT’ The call came to DeKalb Fire Rescue Station 21 shortly after 8 p.m. A collision had left two motorcycles ablaze on Highway I-20 with reports of multiple injuries.
Captain Jeff Daniels and two members of his company—firefighter Michael Gales and driver-operator Travis Owens—were wrapping up a nearby call on Fairington Road when they spotted rising plumes of thick black smoke.

(Left to right) DeKalb Fire Rescue first responders Travis Owens, Captain Jeff Daniels, and Michael Gales were on a nearby call when they observed columns of black smoke.
(Left to right) DeKalb Fire Rescue first responders Travis Owens, Captain Jeff Daniels, and Michael Gales were on a nearby call when they observed columns of black smoke.
They arrived to find twin fireballs—two motorcycles, still burning. Grabbing hoses, Daniels and Gales quickly extinguished the flames while Owens, an emergency medical technician, assessed injuries. There was a woman who had broken her arm falling from her motorcycle, Richardson, and the rider who had struck him.
Owens focused on Richardson, who was clearly in the worst shape. Preparing him for transport, he discovered that Richardson’s nylon-and-mesh riding jacket had melted and hardened, affixing him like a barnacle upon the highway.
Using trauma shears, first responders carefully cut the jacket away from the pavement, leaving a sooty crime-scene outline of Richardson’s torso.
“I’ve worked a lot of motorcycle wrecks out of Lithonia,” Owens says. “Two bikes on fire with a rider melted to the asphalt? That doesn’t happen every day.”
As the body’s largest, most visible organ, skin is our first line of defense—a protective barrier sealing precious fluids in and harmful microbes out. Given all the skin Richardson was missing, Owens knew his condition was critical.
In the ambulance, Richardson’s vitals were hard to assess, there was so much damage. Attempting to administer an IV, Owens found he couldn’t access veins via neck or arms. Instead, he drilled into a shin bone, inserting an intraosseous IV to pump fluids directly into Richardson’s bone marrow—a non-collapsible point of entry.
Within minutes, the ambulance was rolling, with Gales—a medically trained first responder—still aboard. “I just wanted to stay with the patient,” he recalls.
THE ULTIMATE TRAUMA Following early evening rounds, Emory surgeon Juvonda Hodge had just left the Grady Memorial Hospital Burn Center, heading home to chill out, when a call brought her scrambling back to work.
Paramedics were reporting a 20-year-old patient with flame-related burns en route to Grady Hospital’s Marcus Trauma Center, and Hodge was still on call.
Rushing back to the hospital, her thoughts raced ahead. Burns often appear by seasons—space heaters in the winter, fireworks in the summer, campfires in the fall.
But from boiling water to trash fires, thermal (direct heat) burns happen year-round, the most common injuries treated at the center. Every burn is classified by the degree of injury (how deep the damage extends) and the percentage of total body surface area (TBSA) affected. In Richardson’s case, paramedics warned, the damage looked extensive.

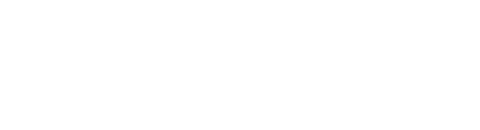
Richardson suffered third-degree burns over 60 to 70 percent of his body, as depicted on the Lund and Browder chart (above) used by the Grady Burn Center.
Estimating the TBSA helps pinpoint not only a patient’s risks, but how much healthy skin remains—a crucial resource down the road, says Hodge, an Emory assistant professor of surgery, trauma, and surgical/critical care at Emory School of Medicine and assistant medical director at the Grady Burn Center.
And Richardson was presenting as a “big burn,” with third-degree burns (damage to all three layers of skin) covering 60 to 70 percent of his body—a TBSA seen in only a fraction of the 700 new patients admitted to the Grady Burn Center each year.
By the time the ambulance arrived, Hodge and her team were waiting. Cutting away Richardson’s charred clothing revealed a lean, healthy young man who was marveling over his melted helmet, although he would have no memory of that later.
“Tell me what happened,” she urged. “Can you move your arm? Your hand? Can you feel me?”
After first evaluating Richardson for trauma—amazingly, there were no broken bones, no major organ injuries—her focus immediately shifted to his damaged skin. A sprawling pattern of burns meandered across his body, etched in random streaks and broad swaths. Much of his torso and back, his face, both arms and his thighs were already an angry, peeling patchwork of pink, tan, and brown.

Emory physicians Walter Ingram and Juvonda Hodge treat thousands of patients each year at the Grady Burn Center, where they help teach the next generation of healers.
But it was his left arm that quickly commanded Hodge’s attention. Typically, the deeper the burn, the drier a wound appears. From Richardson’s left bicep to his fingertips, Hodge could see damage into the muscle, his flesh pearly, tight and hard—literally cooked. When he couldn’t flex his fingers, Hodge grew even more concerned.
Richardson was intubated, given IV fluids, and eased into a medically induced coma to manage his pain. Once stabilized, he was transferred to the burn center’s intensive care unit for cleaning and debridement—the painstaking removal of debris and dead tissue—and a closer assessment of his wounds.
When a deep, full-thickness burn encircles a limb, damaged skin loses elasticity, stiffening like a rigid cast. So Hodge performed an escharotomy— incisions resembling little tiger stripes—along his arms and legs to relieve pressure, improve circulation, and allow Richardson’s underlying tissues to rehydrate, preventing further damage.
When she stepped out to speak with his family, Hodge chose her words carefully.
Burns are the ultimate trauma, stressing every system of a patient’s body. The road to recovery is long, painful, and never straight, she told them, a journey navigated in halting, hard-fought stages. From pneumonia to stubborn infections and potential graft rejection, there was no predicting what complications might arise.
“As long as we keep moving forward, I am going to push forward,” she promised. “If there is a point in time I cannot move forward, I will tell you.”
It was hard to hear. Impossible to imagine this athletic young man—once a scrappy wrestler and football player at Southwest DeKalb High School who enjoyed running anywhere, everywhere—suddenly stilled.
Richardson suffered third-degree burns over 60 to 70 percent of his body, as depicted on the Lund and Browder chart (above) used by the Grady Burn Center.
Richardson suffered third-degree burns over 60 to 70 percent of his body, as depicted on the Lund and Browder chart (above) used by the Grady Burn Center.

Emory physicians Walter Ingram and Juvonda Hodge treat thousands of patients each year at the Grady Burn Center, where they help teach the next generation of healers.
Emory physicians Walter Ingram and Juvonda Hodge treat thousands of patients each year at the Grady Burn Center, where they help teach the next generation of healers.
Grady Burn Center care team From skin grafts and wound care through rehabilitation, burns demand a labor-intensive, cohesive team approach

MARATHON OF ENDURANCE Burn care is a carefully calibrated exercise in rebuilding what is lost—assessing damage, removing dead tissue, and growing or transplanting new skin to replace it.
An excruciating process, it demands time, patience, and fortitude. Deep, extensive burns can require months of treatment and rehabilitation; a full recovery can take years. “The pain is severe and sustained, probably one of the worst types of pain we can go through. And recovery is a marathon, not a sprint,” says Walter Ingram, associate professor of surgery at the Emory School of Medicine and trauma/surgical critical care at Grady.
Ingram, who left a career as a NASA aerospace engineer to pursue medicine, completed his general surgery residency and a trauma/burn fellowship at Emory. In 1992, the year his fellowship concluded, he was named medical director of the Grady Burn Center, which has nearly doubled in size under his leadership.
He now leads the only comprehensive burn center in Atlanta, one of the largest and most highly rated in the country. The center’s medical staff treats some 3,500 adult and pediatric burn patients each year, and teaches the next generation of healers.
Ingram knows the legacy of burns can last a lifetime. It’s not unusual to treat someone as a child and see them return 20 years later with new health issues—skin grafts stretched from weight gain, scars that contract.
Within that long arc of care, from emergency room visits through years of reconstruction, Ingram finds both focus and fulfillment.
In Richardson, Ingram saw three advantages: he was young, fit, and healthy.
Patches where his skin was missing were cleaned and covered with Integra, a clear bio-film made from cow-tendon collagen, shark cartilage, and silicon that acts as a temporary bandage, guarding against infection and restricting heat and moisture loss. An outer layer shields the wound; an inner layer provides a porous scaffolding to encourage skin cell regeneration.
“Artificial skin offers a template,” Ingram says. “Cells will grow into the template to construct a new dermis, then you can come back and replace it with a thin layer of epidermis.”
Without skin, burn patients lose fluid at astronomical rates. So Richardson was inundated with fluids, continually monitored for small changes that could foreshadow bigger problems. Hodge also kept a wary eye on Richardson’s left arm. “We try at all costs to save a limb, especially where a loss could be life-altering,” she says.
But dead tissue amplifies the risk of infection. A little over two weeks after the accident, Hodge determined that his forearm would need to be amputated. Burned to the bone, there was simply no functional blood supply. When he awoke months later, she would tell him, “We were trying to save your life. We just couldn’t save that part of it.”
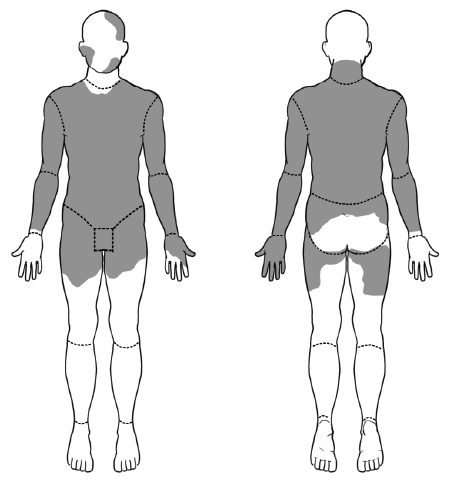
Next, the focus turned to skin grafts, removing healthy tissue from Richardson’s body to replace missing skin, a progression managed over weeks and months. With such extensive damage, most of the grafts would have to come from his buttocks and legs.
To maximize coverage, small, thin pieces of Richardson’s healthy skin were removed, then meshed—fed like a sheet of paper through a machine that punches it with tiny, uniform holes. The result? A grid-like pattern that allows skin to expand, stretching to cover a much larger area.
Skin grafts involve removing small, thin pieces of skin from a patient's body which are fed through a machine that creates tiny, uniform holes, allowing the graft to expand to cover a larger area.
Skin grafts involve removing small, thin pieces of skin from a patient's body which are fed through a machine that creates tiny, uniform holes, allowing the graft to expand to cover a larger area.
Once in place, the expanded graft offers a latticework to support new skin growth, sometimes leaving a net-like texture as it heals. Within days, a successful graft develops blood vessels, connecting to surrounding tissue. Using a patient’s own skin lowers the chance of rejection. With a limited supply of healthy skin, Hodge sometimes had to remove grafts, let the donor site heal, and return later for yet another graft.
Essentially, Richardson became his own skin farm. Only the burns on his face and right hand would heal on their own.
Replacing skin can seem like a raw, bloody business, as surgeons create a new wound to heal another. But among the Grady Burn Center team, Hodge’s grafts are admired for their artistry. “She’s so graceful we call her ‘The Ballerina of Burns,’ ” says Nicholas Ringfield, a member of the team of nurses who cared for Richardson. “Burns aren’t pretty, but her suture lines are like brush strokes, just immaculate.”
Slowly, Richardson was pieced back together, sedated throughout the nearly three-month grafting process—about 14 surgeries, all told. Meanwhile, his care team changed dressings and attended to wound care, monitored vital signs, checked for infection, and addressed his soaring nutritional needs. Growing new skin creates huge metabolic demands, requiring a surge of calories. “People with a big burn don’t leave here fat,” Hodge says. “Without good nutrition, muscle can start breaking down, which can leave them weaker and further compromised, launching a dangerous cycle.”
Through it all, his family waited, wondering what version of Jalen Richardson would return to them.
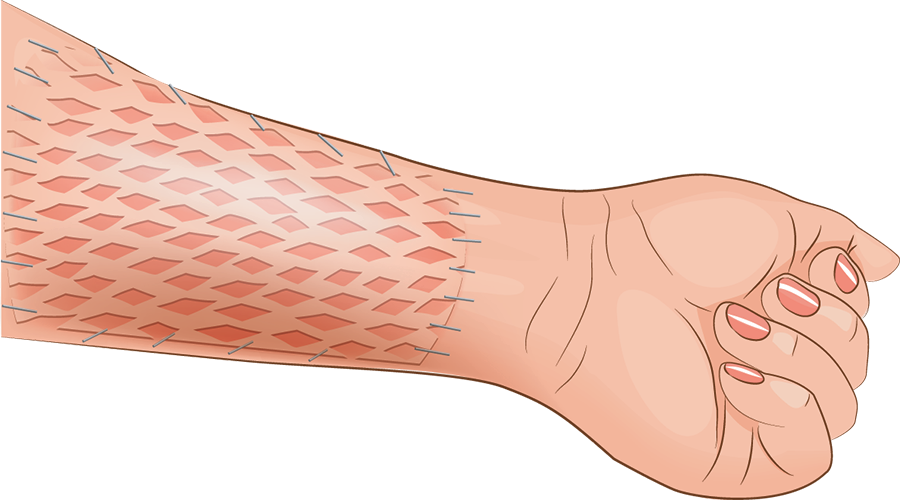
Skin 101
Our largest, heaviest organ, skin serves three critical roles: protection, regulation, and sensation. A burn wound affects each of those functions.
• Consists of three primary layers: the epidermis, a flexible, protective outer layer–the deepest strata produces pigment, which controls skin color; the dermis, a tough, elastic middle layer that cradles sensory nerve endings, hair follicles and sweat glands and helps regulate body temperature; and the hypodermis, the deepest fatty layer, which helps insulate, cushion, and anchor internal organs.
• Serves as our central sensory organ for touch, pressure, temperature, and pain.
• Plays a key role in metabolism, including the synthesis of vitamin D from sunlight.
• Offers a waterproof barrier to help restrict loss of fluids.
• Communicates with our immune system to actively help fight infection.
• Possesses the ability to produce and release hormones.
• Provides protection from harmful UV light.
FACING THE BIG UNKNOWN The last thing Richardson remembers from the accident was the wail of an approaching ambulance. When he awoke, it was November.
Easing out of sedation, Richardson absorbed new sensations: tubes and gauze dressings; an inflatable burn recovery bed; waves of naked, aching pain. Engulfed in bandages, he felt more like a mummy than a man.
Told what had happened, Richardson could only listen. “With a tube in my throat, I couldn’t talk,” he recalls. “I just had to lay there. It was almost like being a sculpture. People would look at me like I was a painting in a museum.”
It took him two weeks to realize his left arm was missing from the elbow down.
In December, Richardson got his cell phone back. Doctors were planning to remove some bandages, and his mother had urged him to document the progress. Turning on his camera phone, he discovered it had been left in selfie-mode. Staring back at him was a face he didn’t recognize, a crazy quilt of spattered pigment.

The fiery accident left Richardson’s face a peeling patchwork of pink, tan and brown. “It was tough to see,” he said. “I knew it was going to be hard to live with.”
“Pretty much everything was 50 shades of pink and brown,” he says. “It was tough to see. I knew it was going to be hard to live with.”
His once-chiseled 170-pound frame had withered to 113 pounds, his body a tender landscape of healing grafts. Before the accident, Richardson was a wheeled vehicle mechanic with the Georgia Army National Guard, taking health and fitness classes at Clayton State University, and posting workout tips on YouTube.
Now he was too weak to roll onto his side, much less stand and walk.
Healing would take time. His days narrowed to a painful cycle of wound care: removing bandages, cleaning and redressing grafts. “It can bring you down,” he admits. “All you are thinking about is going through this pain every single day with no relief in sight.”
Soon, his caregivers began to see sparks of personality. Even while intubated, Richardson would scribble funny quips on paper to coax a smile. Within him, a light seemed to be flickering back on.
Hodge was optimistic. Aside from his arm, Richardson was presenting a textbook recovery. And though he faced a long rehabilitative road, he was making solid progress.
Plans were made to release him shortly before Christmas, a departure typically marked by balloons and cheering. Yet for Hodge, it’s a bittersweet moment. “You know that you’ve done the best you can do, and that the rest is up to them,” she says. “It’s like, ‘I’ve gotten you to the fourth quarter, but you have to finish.’”
“That’s always the big unknown,” she adds.
BURN CENTER 2.0 After just a few weeks, Richardson was back.
Physically, he was decompensating—malnourished, still unable to stand. Some of his wounds were breaking down, a few donor sites opening back up. Returning to the hospital felt like a setback, leaving him depressed and disengaged.
His care team diagnosed a “failure to thrive.” Richardson’s nutritional intake just couldn’t keep pace with his soaring metabolic needs.
Hodge was stunned; Richardson had shown so much promise. “For a burn surgeon, to go back and close wounds that you created is disheartening,” she admits. “My first thought was ‘What went wrong? What can we do to support him? How are we going to bring him back?’ ”
“For patients who are here a long time, it’s hard,” Hodge acknowledges. “Progress is slower, and it’s an emotional journey. It was a matter of ‘How can I help this kid realize he’s strong enough to get through this?’ ”
Every patient defines their own recovery, says Ingram, who chose burn care in part because of the lifelong relationships it offers. Along the healing continuum, it’s not uncommon to see depression and frustration, he adds, especially in young people.
So they started over: Repairs and daily wound care; scar management; nutrition; pain control and rehab. “Burn care demands a very labor-intensive, cohesive team approach,” Ingram says.
This time, Richardson didn’t want his blinds open or the television on. The pain made him feisty. Some days, he refused to shower, didn’t want his sheets changed, resisted therapy. He begged to be sedated again, to sleep through the pain.
It was, he acknowledges, the darkest chapter of his journey.
Wound care that should have taken under an hour could drag on all day. To Richardson, it felt like reliving the accident all over again. “They see progress, but I was just seeing these big bloody wounds, every day,” he says. “All I could think about was day after day of more wound care. I was giving up on myself.”
Once, while Ringfield was redressing Richardson’s wounds, he was startled to hear a strange voice on speaker phone: “Hello, 911, are you safe?”
Looking up, he realized Richardson was calling the police.
It was a first, but the nurse understood. “Here’s a 20-year-old, just coming into himself, with all decision-making capacity stripped away,” he says. “With wound care, there can be anguish, depression, and anxiety. We step out of the room and patients are left with their thoughts. Why me? Who will love me? Will I look the same? Will I go back to work? All the Kübler-Ross stages of grief are there.”
That’s when Hodge stepped in. Some days, after working a full shift she would stop by to change Richardson’s bandages herself. “Every patient is different, with different needs,” Ringfield reflects. “She brings what I call individualized compassion.”
At 5’11”, Hodge is a formidable presence: strong, capable, and direct. Working with Richardson became a daily battle of wills. But she could be stubborn, too. “God told me to keep pushing,” she says. “Some days I would have to shut the door and say, ‘Jalen, this needs to happen. It’s going to happen…’ ”
Richardson came to see it as tough love, a firm push forward. “She would come in and give me that look,” he laughs. “She would not let me give up on myself.”
In time, he was calling her “Mama Hodge.”

The fiery accident left Richardson’s face a peeling patchwork of pink, tan and brown. “It was tough to see,” he said. “I knew it was going to be hard to live with.”
The fiery accident left Richardson’s face a peeling patchwork of pink, tan and brown. “It was tough to see,” he said. “I knew it was going to be hard to live with.”
CANINE CONNECTION For weeks, Richardson seemed at a plateau. Until one day, a dog waddled into his room. Peaches was a low-slung Basset hound with droopy ears and a two-toned face, among the first certified therapy dogs to visit patients in the burn center.
“She was a mood booster, always genuinely excited to see me,” he says. “You can’t fake that. A dog doesn’t fake emotions.”
Soon, Peaches was joined by others: Honey Duke, a yellow mixed-breed retriever, and Mocha, a chocolate lab. It was the first time Richardson’s nurses had seen him smile in months.
His care team noticed: If visiting dogs could do that, how would he progress with his own service dog? That’s when they consulted Kimberly Brenowitz, founder of Animals Deserve Better/Paws for Life, a Marietta-based nonprofit that rescues and trains service, assistance, and therapy dogs.
On her first visit, Brenowitz arrived with a therapy dog only to learn that Richardson hadn’t walked in seven months. “The only place the dog could actually greet him was the big toe of his right foot—everything else was covered in gauze,” she says. “At the time, they didn’t know if he would walk again.”
With his permission, she began searching for a big, sturdy dog that could pull for him, maybe help pick things up. One day, she brought a photo of a young Native American Indian Dog, noted for their strength and intelligence. “It was love at first sight,” she says.

With support from the Semper Fi Fund, a nonprofit that aids American service members and their families, Brenowitz began training Hakon. (His littermate, Finn, is a therapy dog with Emory’s Counseling and Psychological Services program.)
Initially, Hodge was cautious. Dogs bring responsibility, and with all Richardson had been through, she didn’t want to set him up for failure. Still, it was worth a try. “Sometimes, you just want to feel normal,” Hodge says. “A dog offers unconditional acceptance.”

A LONG ROAD BACK In time, Richardson and Hakon became inseparable, partners in recovery. While healing, skin grafts can contract, restricting movement. At first, Richardson couldn’t even straighten his torso to sit in a wheelchair, so that became a goal. Next, he began extending his legs in physical therapy, reaching to touch Hakon’s soft, shaggy coat with his toes—small, slow movements that left him sore and exhausted.
Sometimes, the dog would sniff the bandages where Richardson’s left forearm had been. “When I was in pain, it was like he could sense it and would be closer to me,” he says.

When visiting therapy dogs helped Richardson progress, his care team suggested he might benefit from his own service dog. Enter Hakon, who became a partner in his recovery.
His therapists tied a leash to the left side of Richardson’s wheelchair, allowing 108-pound Hakon to pull him down the hallway while Richardson steered with his right hand—the most mobility he’d known in months.
As a kid, Richardson loved to run, sometimes racing his mother’s car to the grocery store for fun. Now, walking was a distant goal. “Walking was tough,” Richardson says. “It brought a lot of pain—something you once did so naturally, now you have to re-strengthen your body and learn all over again.”
A missing forearm ruled out crutches. Instead, Richardson would bend over the back of a rolling chair, leaning on his right arm and anchoring the stub of his left elbow, slowly sliding forward, one step at a time. Each success left him wanting more.
“There was no way I felt I could do this dog justice sitting in a chair,” he says. “All the dogs I’ve ever had wanted to run and play. I knew that if I learned how to walk again, I was going to run again.”
Once, Richardson had refused physical therapy; now, he was begging for bigger challenges.
After 14 months in the Grady Burn Center, Richardson was released to a rehabilitation facility in Newnan, Georgia.
As he left the hospital, blaring across the intercom that normally paged doctors was “Eye of the Tiger,” the theme song from Rocky III. At the rehab center, a physical therapist asked about his goals. “I told her I wanted to walk out of there,” he says. “She said in the amount of time we had it would be a stretch, but every day I gave it my all, and we got close.”
Once home, Richardson secured his own rolling chair. “Every step I took, Hakon was there to take a step next to me,” he says.

When visiting therapy dogs helped Richardson progress, his care team suggested he might benefit from his own service dog. Enter Hakon, who became a partner in his recovery.
When visiting therapy dogs helped Richardson progress, his care team suggested he might benefit from his own service dog. Enter Hakon, who became a partner in his recovery.

A desire to return to his Georgia National Guard unit — Charlie Company 151, part of the 78th Aviation Troop Command — drove Richardson throughout his long recovery.
A desire to return to his Georgia National Guard unit — Charlie Company 151, part of the 78th Aviation Troop Command — drove Richardson throughout his long recovery.
THE FINAL TEST Ultimately, Richardson yearned to return to his unit—Charlie Company 151, part of the 78th Aviation Troop Command, the aviation arm of the Georgia National Guard, which had supported him throughout his long recovery.
During company drills inside an aircraft hangar at Dobbins Air Reserve Base “they would literally be pushing me in a wheelchair,” he says. But a return to full duty meant Richardson would have to pass a standard physical fitness test.
Balancing on a prosthetic arm, Richardson could do pushups, and he could even handle sit-ups. But the test included a timed two-mile run—eight long laps around a track. Once, it would have been easy. Now, simply finishing would be a victory.
In April 2018, Richardson decided to give it a shot, his first full-out attempt at running in two years. Racing against the clock, each stride tugged at his grafts, bringing sharp pains. “My legs didn’t work like they were supposed to, my skin was all contracted,” he says. “I was doing a bunch of waddling, a bunch of crying. But I got it done.”

A desire to return to his Georgia National Guard unit — Charlie Company 151, part of the 78th Aviation Troop Command — drove Richardson throughout his long recovery.
His unit was stunned: Richardson completed the two-mile run in 17 minutes and 30 seconds, about a minute over the maximum time allowed. Weeks later, he would be back, clearing the required time with room to spare.
As his workouts progressed, Brenowitz, the dog trainer, could see big, mellow Hakon struggling. Could the dog be holding him back? “As much as you love Hakon, he might not be right for you,” she told him. “He’s not built to go where you need to go. You need a dog who can give you a run for your money.”
Enter Shadow, a headstrong, high-energy Alaskan malamute.

As Richardson grew stronger, his first service dog struggled to keep up with him. His trainer recommended Shadow, a high-energy Alaskan malamute, who became his new training partner.
As Richardson grew stronger, his first service dog struggled to keep up with him. His trainer recommended Shadow, a high-energy Alaskan malamute, who became his new training partner.
“He was the cockiest, most independent, pain-in-the-butt puppy I’ve ever met, and I thought, ‘Jalen, you’ve met your match,’ ” Brenowitz says, laughing. “He became the shadow that followed him everywhere.”
Soon, Richardson was sprinting around Stone Mountain, Shadow by his side. Since then, he’s been on three National Guard deployments. Last summer, Shadow went with him.
Today, Richardson continues to train hard with friends who challenge each other. That two-mile run? He now holds the fastest time in his unit.

To stay in shape, Richardson enjoys running in parks throughout metro Atlanta with Shadow by his side.
To stay in shape, Richardson enjoys running in parks throughout metro Atlanta with Shadow by his side.
SOLDIER OF THE YEAR
Richardson is a flight operations specialist with the Georgia National Guard and in September was named the 78th Aviation Troop Command’s “Soldier of the Year.”

SKIN THAT TELLS A STORY Burn care is more than replacing skin; it’s also about healing something even deeper.
Sometimes patients get well and you don’t know how, acknowledges Hodge. Sometimes, you learn the most from your setbacks, the struggle revealing a new way forward. And some patients, she says, you never forget. For the Ballerina of Burns, that’s what keeps her fingers dancing.
After a year-long stay in the burn center, Jalen came to see his care team as extended family. But lately, his visits have slowed for the best possible reason—an active life gets in the way.
At 24, Richardson now owns his first house, with a room dedicated to his reptile collection: three boas, a tortoise, and a five-foot-long Nile monitor lizard, at last count. It’s hard not to feel a kinship: Regrowing his own skin and the pebbled texture of his grafts makes him “a human version of a reptile,” he jokes.
Amid the trophies that line his fireplace mantle rests his partially incinerated helmet—a reminder, he shrugs. Not long ago, he had a motorcycle customized to operate one-handed, to prove he could ride again. Then he sold it. For now, he’ll stick with four-wheelers.

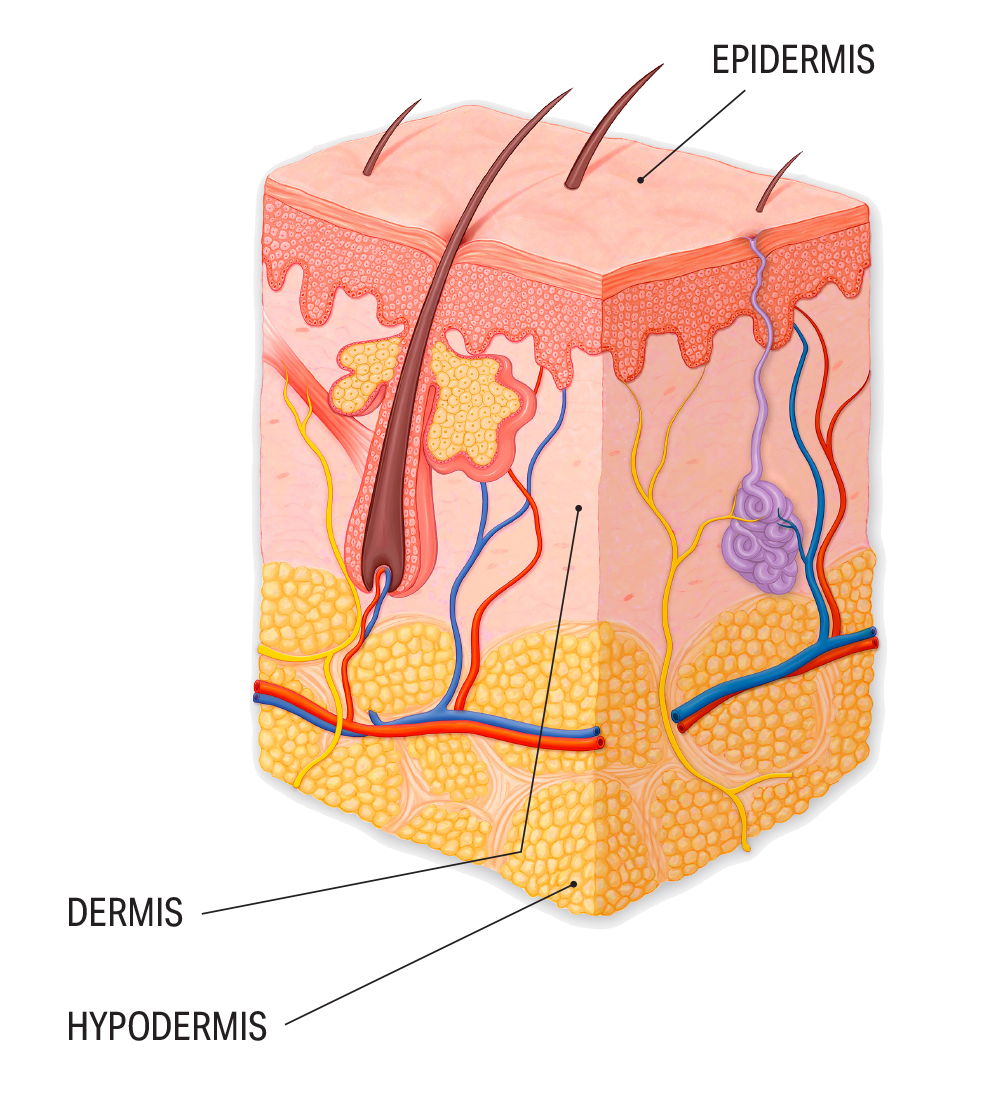
Motivational reminders encircle a stack of bracelets worn over the grafts on Richardson’s right arm.
To celebrate his recovery, Richardson attempted to get a tattoo on his right arm—a phoenix rising from the ashes. But the ink refused to stay, fading into his grafts. In the end, it didn’t matter.
“My skin is a tattoo in itself,” he’s decided. “My scars tell a story of their own.”
By Kimber Williams, Photos by Jack Kearse and Steve Nowland, Video by Damon Meharg
Watch the complete video

Motivational reminders encircle a stack of bracelets worn over the grafts on Richardson’s right arm.
Motivational reminders encircle a stack of bracelets worn over the grafts on Richardson’s right arm.