Arrival of
the Bees
When the buzzing in my brain meant stroke
This is not the story it was supposed to be, not by a long shot. It was supposed to be about brain research, with an emphasis on the Emory Healthy Aging Study. But then a blood clot unleashed a beehive in my brain. This story begins with the bees.

A few minutes before 7 p.m. on August 5, 2018, a day before my son Joe’s 17th birthday, I was watching a repeat of Seinfeld with my wife, Jane, and Joe, when the laugh-track faded sharply, giving way to the shrill buzz of what felt like electric bees deep inside my right ear, a sudden sonic swarm, the sound of a brain starving to death.
While Jane gave Joe (who is fed through a G-tube) his supper a few feet away, there was a hemoglobin traffic jam clogging one of the arteries that supplies nutritious blood and oxygen to my cerebellum. I was having a cerebellar stroke.
The buzz went away after a few seconds, leaving an all-consuming dizziness and nausea in its wake. My personal universe spun in the opposite direction of everything else. So began a vomit marathon and then several days of hell involving: A trip to the hospital emergency room and a stay of several days; a camera down my throat and the discovery that I had a hole in my heart, which may or may not have caused the stroke; the tangible realization that I was old enough to drop dead in a second; oh, and my second MRI in two weeks.

Jerry Grillo plays guitar as his wife, Jane, and son, Joe, listen in their north Georgia home. “It’s harder to play a B-minor bar chord now,” he says, after his stroke. “But it’s all gotten better with repetition.”
Jerry Grillo plays guitar as his wife, Jane, and son, Joe, listen in their north Georgia home. “It’s harder to play a B-minor bar chord now,” he says, after his stroke. “But it’s all gotten better with repetition.”
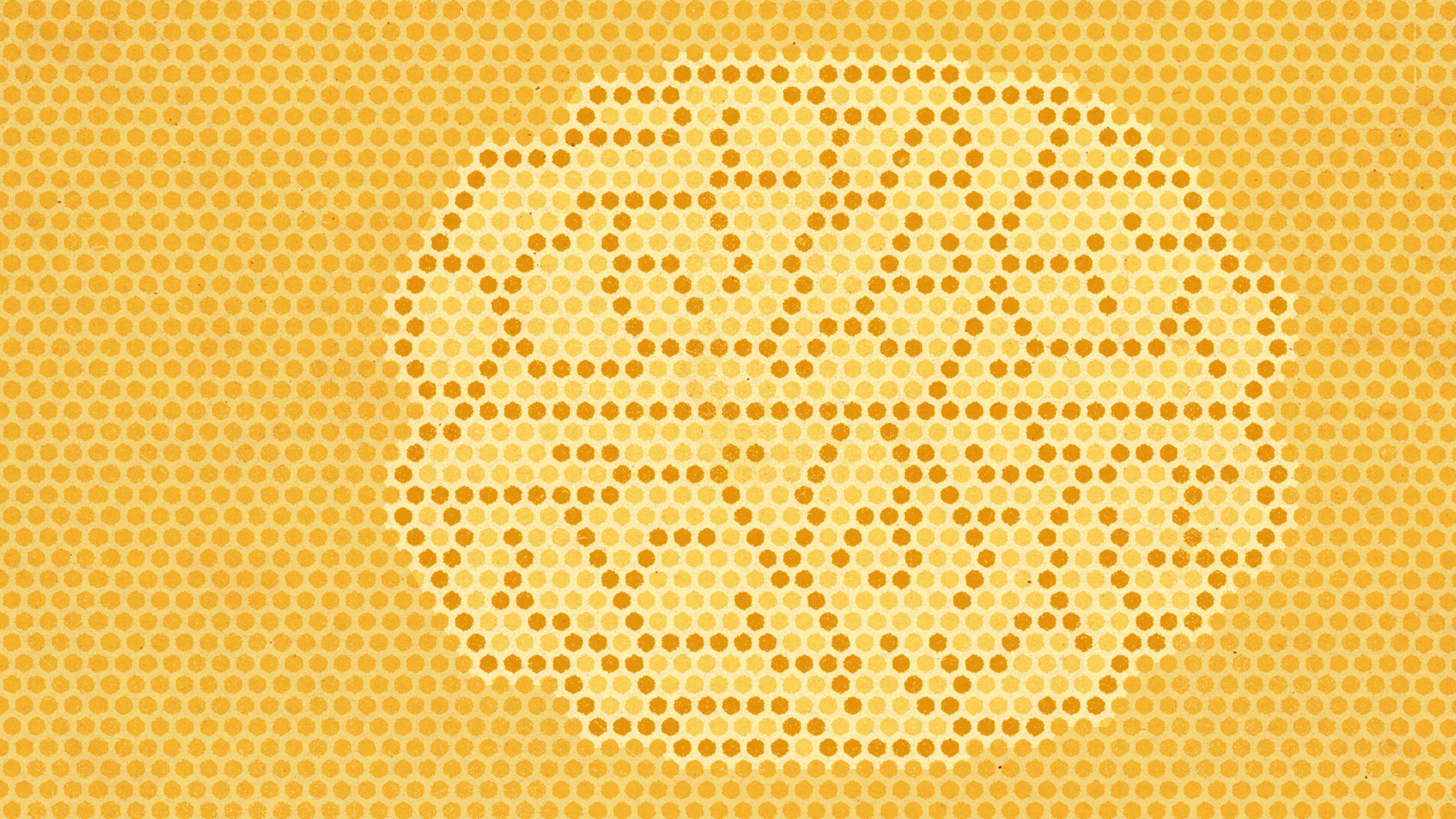
About that first MRI
Two weeks earlier I began work on the story this was supposed to be. I paid a visit to Jim Lah, an Emory neurologist and principal investigator for the Emory Healthy Aging Study. The plan was to undergo an MRI procedure so I could write about the study while going through what a typical participant would. My ears were plugged to muffle the intense racket caused by vibrating metal coils carrying rapid pulses of electricity. As I lay on my back in the snug tube, I stared up at a computer screen with a slide show of calming, bucolic images, glad this was just research.
James Lah, associate professor of neurology and principal investigator of the Emory Healthy Aging Study.
After that, we went over the images of my brain to understand what researchers can learn from high-tech imaging. It was Lah, me, and another journalist, Jaye Watson, who was working on a GPB television segment that was going to dovetail with my story. Lah pulled the images up on a monitor and said, “Your brain looks brand new, like it’s never been used, right out of the package.”
That joke was all I remembered from the interview. I had forgotten everything else from that day until I found the gumption to listen to the recording five months later, in January 2019, and heard something that gave me chills: Lah is going over images of my brain and says, “I just want to make sure there’s nothing scary here, or unexpected.” Jaye responds lightheartedly, “The story might not happen at all if that were the case,” and then adds an imaginary explanation to an imaginary boss, “We were going to do the story, until he became a patient.”
Lah concludes with, “Until he had to go to the emergency room.” On the recording, I was laughing.
But it’s not so funny anymore. Turns out, neither Jaye nor I did the stories we were supposed to do.
Cerebellar strokes account for about 10 percent of all strokes and they’re not easy to diagnose. Indeed, they are often misdiagnosed as migraines, gastritis, meningitis, even inner ear infections. But if not recognized and quickly treated as the stroke they actually are, they can ruin your life—or end it.
I was lucky. Lucky because, even as my brain raged, I had the presence of mind to take an aspirin. Lucky because, like 88 percent of strokes, mine was an ischemic stroke, in which a blockage or clot in an artery to the brain causes reduced blood flow. Aspirin thins the blood and can break up a clot.
On the other hand, if this had been a hemorrhagic stroke, the kind where a blood vessel bursts in the brain, the aspirin makes the bleeding worse.
Location, location, location
“All things considered and in the grand scheme of things, if you had to choose a stroke, the kind you had would be near the top of the list,” Lah told me in January 2019, the second time we met. “When it comes to damage in the brain, the same three rules apply as the first three rules of real estate. Do you know those? Location, location, location.”
The same rule also applies to neurologists, which is why I wound up at the Emory Clinic in the care of Fadi Nahab, medical director for the stroke program at Emory University Hospital and Emory University Hospital Midtown. After looking over my MRI from the night of the stroke, Nahab told me that I’d actually had two strokes. He saw evidence of not only the cerebellar stroke, but an earlier episode closer to the front of my brain.

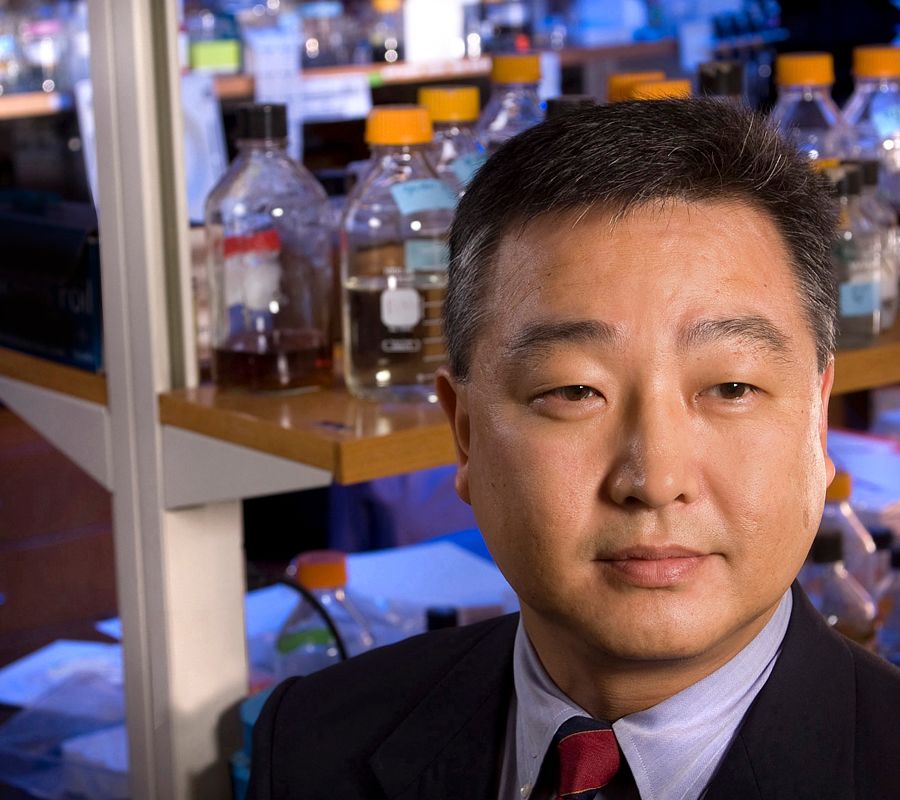
Fadi Nahab, associate professor of neurology and pediatrics and medical director of several Emory hospitals’ stroke programs.
At some point, it seems, I’d had some type of minor stroke, probably while sleeping. I have no memory of it, but learned of something called a silent stroke, which often has no symptoms but still causes damage to brain tissue.
We still don’t know exactly when that first, mysterious stroke happened, but we finally know why the cerebellar stroke happened. We’ll get to that in a moment.
The risk factors for stroke are high blood pressure, high cholesterol, heavy smoking, alcohol and drug abuse, and a sedentary lifestyle.
I had high blood pressure that I wasn’t treating, but the cholesterol was under control with medicine. Everything else was off the table. I’m not a smoker, not a heavy drinker, and I was in great physical shape—I thought.

Jane, Jerry, and son, Joe, Grillo out for a walk in the woods near their home.
Jane, Jerry, and son, Joe, Grillo out for a walk in the woods near their home.
Brain-heart connection
While I was in the hospital following the episode, doctors found a patent foramen ovale (PFO), a hole between the left and right atria of my heart, that I’d lived with, blissfully unaware, for 57 years. We all have PFOs in utero, but they usually close shortly after birth. For about 25 percent of us, they stay open and, in some circumstances, a PFO will allow a clot to pass through the heart and travel up to the brain.
In some cases, the PFO together with another condition, like atrial fibrillation (an irregular heartbeat), can increase the risk of stroke. So, three months post-stroke, in November, an Emory physician implanted a loop recorder in my chest to record my heart rhythms for the next three years, monitoring for atrial fibrillation, or some other sign that the PFO was responsible. A few months after the device (which is smaller than a thumb drive) was installed, we found it was working just fine. It recorded atrial fibrillation, probably while I was playing basketball. I never felt a thing, but that’s not uncommon with AFib, I was told.
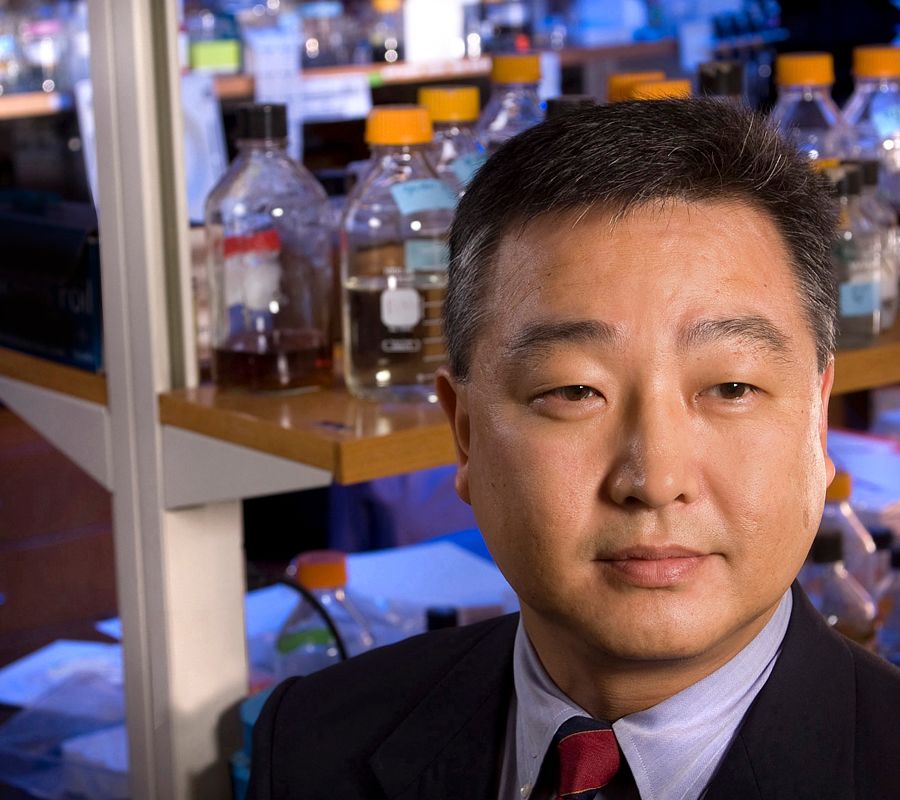
Even if the PFO wasn’t responsible, “having a stroke is a warning sign that your brain already sustained some kind of injury from a decrease in blood supply,” according to Ihab Hajjar, associate professor of medicine at Emory.
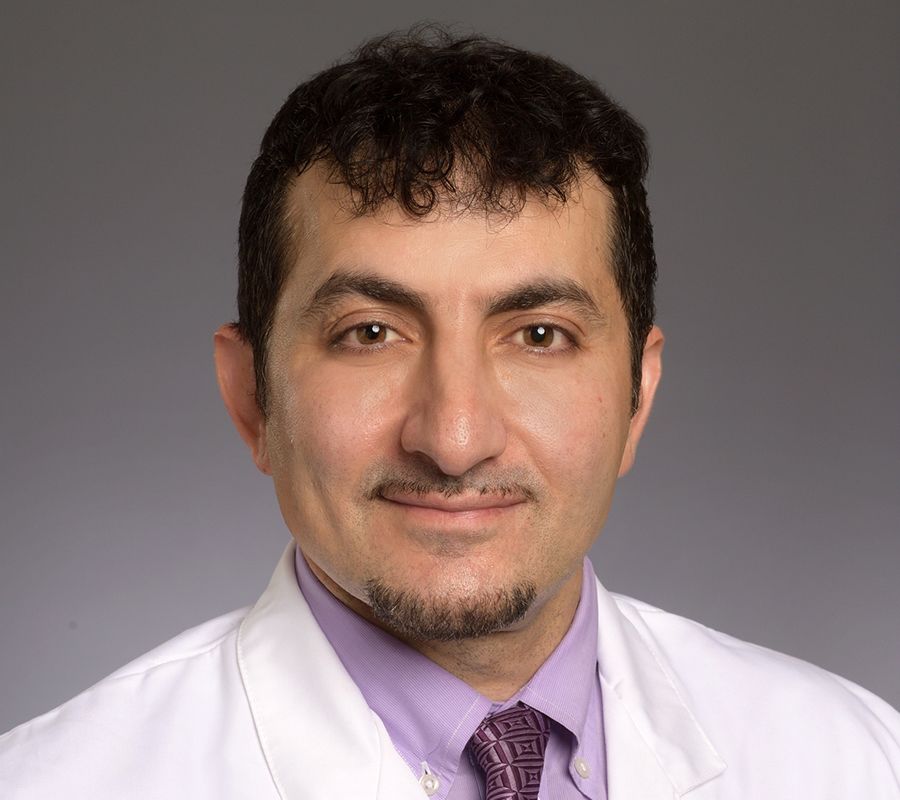
Ihab Hajjar, associate professor of medicine and geriatrics, leads Emory’s Brain, Stress, Hypertension, and Aging Research Program.
An internist and geriatrician, Hajjar leads Emory’s Brain, Stress, Hypertension, and Aging Research Program (BSHARP), a team of researchers exploring the links between brain health and the cardiovascular system.
Hajjar is researching the connection between high blood pressure (hypertension) and cognitive impairment later in life. He’s found that drugs for high blood pressure (such as lisinopril, the drug that I’ve been on since the stroke) have an added benefit.
“Evidence has shown that when you treat hypertension, especially in the early stages, you potentially prevent cognitive decline later in life,” Hajjar says. This is positive news for me, since I’ll probably be treating my high blood pressure from now on.
With Nahab and Hajjar, I’ve found two biomedical heroes whose work I’m personally interested in. Nahab sees 2,000 patients a year and estimates that 200 of them have had cerebellar strokes. His research focus is on cryptogenic stroke of an undetermined cause.
Thankfully, data collected from the monitor in my chest helped clear up my mystery.
I’m back on the basketball court (though at a more cautious pace).
But sometimes my imagination takes me down some dark roads. For instance, every time I drive, I make a mental plan of what to do if the bees come back. I try to stay close to the shoulder or the median, due to this irrational fear of crashing while having a stroke and taking out some other poor motorist.
I wonder about dying suddenly, or becoming incapacitated. My responsibilities require a fully functioning (and breathing) Jerry. Chief among these are my son, Joe, who is profoundly affected by cerebral palsy. He needs his old Pop, at least for a few more years. The bottom line is, I must be physically and cognitively capable of lifting and caring for my son. Dropping dead or out are not options. I come by my high blood pressure honestly.
Fortunately, my physician is excellent. He’s also glad I’m his patient and was thrilled by the challenge of a mystery like the one my stroke presented. (Of course, I never really shared his enthusiasm.)
“Frankly, I get excited when I see patients who are told, ‘We don’t know what caused your stroke,’ ” Nahab says. “I know that they are going to the forefront of evaluation and treatment, and that I will most likely be able to give them peace of mind.”
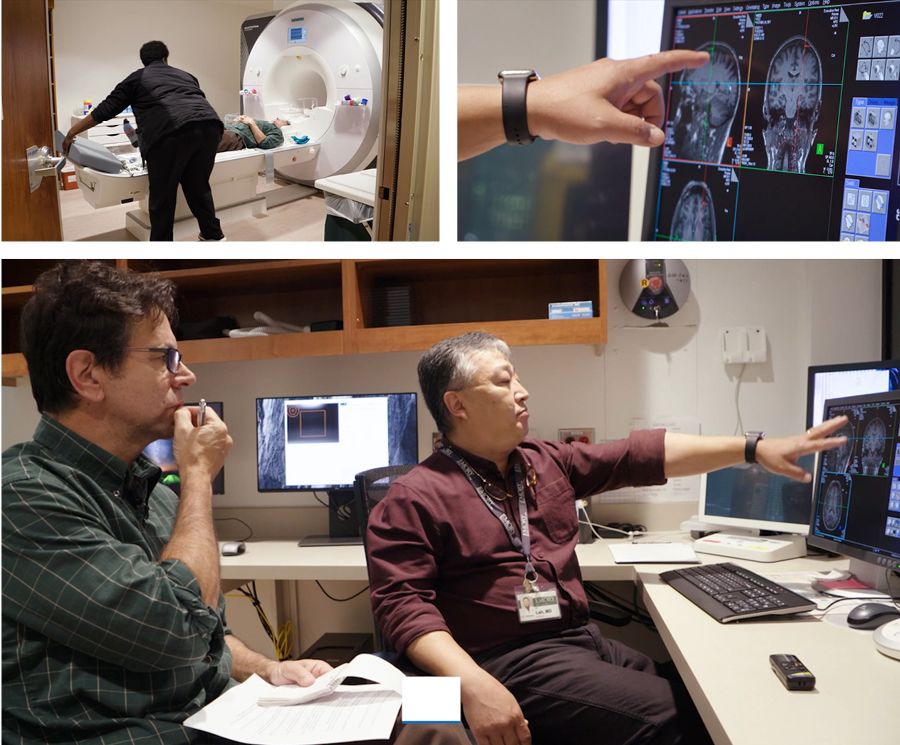
Writer Jerry Grillo gets an MRI of his brain, and goes over the resulting scans with neurologist James Lah.
Writer Jerry Grillo gets an MRI of his brain, and goes over the resulting scans with neurologist James Lah.
James Lah, associate professor of neurology and principal investigator of the Emory Healthy Aging Study.
James Lah, associate professor of neurology and principal investigator of the Emory Healthy Aging Study.

Fadi Nahab, associate professor of neurology and pediatrics and medical director of several Emory hospitals’ stroke programs.
Fadi Nahab, associate professor of neurology and pediatrics and medical director of several Emory hospitals’ stroke programs.
Ihab Hajjar, associate professor of medicine and geriatrics, leads Emory’s Brain, Stress, Hypertension, and Aging Research Program.
Ihab Hajjar, associate professor of medicine and geriatrics, leads Emory’s Brain, Stress, Hypertension, and Aging Research Program.

Doug Bremner, professor of psychiatry and radiology and director of the Emory Clinical Neuroscience Research Unit.
Doug Bremner, professor of psychiatry and radiology and director of the Emory Clinical Neuroscience Research Unit.
Andrew Miller, professor of psychiatry and behavioral science, is director of the behavioral immunology program.
Andrew Miller, professor of psychiatry and behavioral science, is director of the behavioral immunology program.
Looking to the future
Nahab collaborates with colleagues in hematology and neurology on his research, which focuses on a blood biomarker that may be an appealing target for identifying how best to treat a cryptogenic stroke. “Studies completed more than a decade ago basically put patients on an aspirin and wished them good luck,” Nahab says. “But we’ve known for a while that patients who have had a cryptogenic stroke may have issues that necessitate blood thinning medicine that is stronger than aspirin.”
Nahab wants to remove “cryptogenic” from the equation, as he did with me. He and colleagues have pinpointed blood biomarkers that identify patients most likely to develop clotting and are conducting clinical trials to determine which patients respond to which treatments. “The goal is to get patients the appropriate treatment before they have a recurrent stroke,” he says.
My biomarker numbers didn’t reveal any overwhelming coagulation activity, so I didn’t qualify for a clinical trial. Before the AFib was discovered, I was taking an aspirin every day as part of the post-stroke, new-life regimen. But I’ve since been prescribed an expensive blood thinner called Eliquis.
For several months, when the loop monitor wasn’t showing an irregular heartbeat, I hoped for a definitive answer, wondering if and when another bomb would go off. Now, I sometimes wonder if and when my heart will clock out. But honestly, I’m way too busy to give worry and fear much time and energy.
And besides, my recovery has been spectacular. Did I say that I was lucky? Cerebellar strokes, of course, attack the cerebellum, which sits in the back of your skull at the bottom of your brain, where it controls movement and balance. It has symmetrical left and right sides, each controlling movement for the corresponding side of the body. So while most strokes leave their marks on the opposite side of the body from where they occur in your brain, cerebellar strokes affect the same side.
My stroke was on the left side, so my left arm and left leg were affected. But not extremely and not forever. There is some lingering delay in my left-hand—my typing isn’t as fast and accurate as it used to be, and playing guitar is harder than it was (not that it was ever easy for me, but a B-minor bar chord should not be that difficult to play). It’s all gotten better with repetition.
Brainstorming solutions
Hope for patients with brain issues, like me—honestly, like most of us if we live long enough—rests with researchers like the ones I met at Emory while working on this piece.

Doug Bremner, professor of psychiatry and radiology and director of the Emory Clinical Neuroscience Research Unit.
Doug Bremner, a professor of psychiatry and radiology and director of the Emory Clinical Neuroscience Research Unit, is looking into electrical treatment for post-traumatic stress disorder using noninvasive vagus nerve stimulation, which also may be effective for other disorders, such as severe anxiety.
Andrew Miller, professor of psychiatry and behavioral science, is researching the link between brain inflammation and depression. “Our laboratory is particularly interested in the neurotransmitter systems that are affected by inflammation,” Miller says. “We’ve established quite a detailed map, if you will, of how the immune system can influence behavior in the context of inflammation.”
Andrew Miller, professor of psychiatry and behavioral science, is director of the behavioral immunology program.
Lah, of course, is helming the Emory Healthy Aging Study, which includes several sub-studies: the Healthy Brain Study, the Midlife Depression Study, and the Brain Imaging Project. The Healthy Aging Study was developed to understand and better treat dementia, Alzheimer’s disease, and other age-related disorders. “There is so much we still don’t know about brain diseases like Alzheimer’s,” says neurologist Allan Levey, co-principal investigator of the study and Goizueta Foundation Endowed Chair for Alzheimer’s Disease Research. “So it’s important to get as many people as possible to participate in research studies like this to increase our ability to prevent these diseases in the future.”
This relies on v0lunteers like Mary Jenks. “First, I’m obviously aging,” she quips. “I saw a notice about the Emory Healthy Aging Study and thought, ‘This could be interesting.’ ” Jenks went so far as to volunteer to get a lumbar puncture for research.
She took care of her aging mother and knew the cascading difficulties associated with cognitive decline. “I didn’t want to end up the same way,” says Jenks, who worked in special education for many years teaching deaf children in DeKalb County. She now teaches non-English speaking children: “It makes your brain grow.”
The Emory Healthy Aging Study (online) has registered 27,929 people, consented 22,136, and completed data collection on 14,989. The Emory Healthy Brain Study (face-to-face, blood, spinal fluid, cognitive testing, etc.) has completed 1,101 visits.

Jerry Grillo hopes to remain healthy and vital, after recovering from an unexpected stroke.
Jerry Grillo hopes to remain healthy and vital, after recovering from an unexpected stroke.
Happy 100th
Around the globe, centenarians are expected to number 3.7 million by 2050 (!), and one in five Americans will be 65 or older by 2040. The information gathered from the Emory Healthy Aging studies could bring out the glimmer in our golden years. I’m not sure what my chances are for reaching 100—or even 65.
Lah, my chief source for both the story I was supposed to write and the one you’re nearly finished reading, tries to be reassuring. “We can’t tell you what the exact likelihood of a recurrence is for someone in your situation,” he says. “But I can tell you it’s very, very low. The problem is, you know just enough to scare the hell out of you.” EHD
Illustration by Dan Page • Animation by Kirk Leitch

PAYING IT FORWARD

What if we could learn something from our aging bodies to help the next generation? This is the intent of Emory’s Healthy Aging Study, the largest clinical research study ever conducted in Atlanta. From people volunteering to participate in the study, researchers can learn vital information about the most common types of age-related diseases: Alzheimer’s, cardiovascular disease, diabetes, and cancer. “It gives us an opportunity to open up a huge group of participants that can be accessed by investigators in any aging-related field—whether it’s brain or heart or mobility health,” says James Lah, principal investigator.
To learn more or to join the study, go to: healthyaging.emory.edu, or call the Emory Brain Health Center at 404-727-4877.