POWER & PRECISION
Proton therapy arrives in Georgia

With the opening of the Emory Proton Therapy Center, a first in Georgia and one of fewer than 30 in the nation, Winship Cancer Institute adds a powerful radiation therapy option to its broad array of cancer-fighting tools.

Combining the latest advances in radiation technology, engineering, and medical physics, Winship physicians will employ proton therapy to deliver a treatment precisely where needed—with less spillover to adjacent healthy tissue. That means less radiation exposure to normal tissues and the potential for fewer side effects and complications, especially for cancers near sensitive organs, and for children whose tissues are still developing.
The new three-story, 108,000 square foot Emory Proton Therapy Center officially opened with a ribbon-cutting ceremony on Dec. 6.
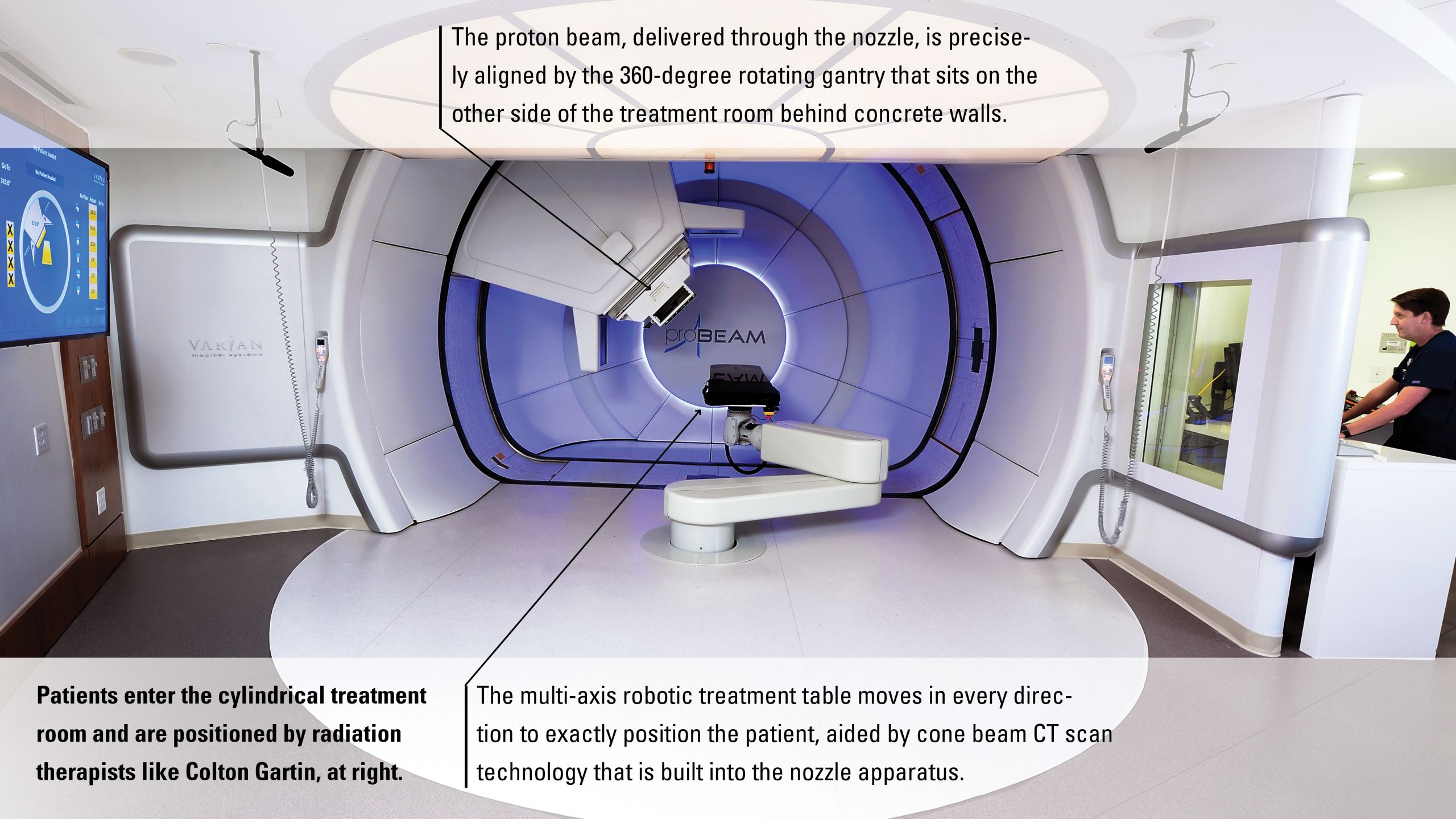
With the main entrance located on Ponce de Leon Avenue down the street from Emory University Hospital Midtown, it had to be big. The cyclotron that gets the subatomic protons whirling, gaining the energy they need to destroy cancerous cells, weighs 90 tons, equivalent to a loaded 757 jet. The vacuum tube that transports the accelerated protons from the cyclotron through the facility at nearly two-thirds the speed of light, guided by magnets, is about 100 yards long, and runs the length of Juniper Street.

Radiation therapist Ndipnu Lima makes sure patients are correctly positioned.
That’s long enough to reach all five treatment rooms and strong enough that the powerful protons can penetrate almost a foot into the body, reaching the deepest tumors. The three-story building is tall enough to accommodate hidden 240-ton gantries in four of the treatment rooms. These can rotate 360 degrees to aim beams to the precise spot needed while the patient lies on the table without having to move. The fifth room has a fixed beam for treatments not requiring rotation.
One of the advantages of being one of the newest proton centers in the country, says Medical Director Mark McDonald, is that “we are opening with enviable technology.” He’s particularly pleased that every treatment room has “pencil beam scanning” that delivers small “spots” of radiation that match the shape of the target and adjust to the different depths and contours of a tumor in a plan personalized for each patient. The system also uses cone beam CT technology. While most facilities position patients before treatments using X-rays that see only bones and dense matter, cone beam CT scans show soft tissue and internal anatomy. This allows precise positioning of the patient based on the location of the tumor, and it enables monitoring for any changes in the patient or in the tumor itself which would necessitate changes in the treatment plan.
Like X-ray radiation therapy, McDonald says proton therapy is invisible and painless. “While any treatment can have risks and side effects, our goal with proton therapy is to reduce or eliminate some of the side effects associated with other radiation treatment options.” Treatment decisions will be made on a case-by-case basis by a multidisciplinary Winship team, says McDonald. For some patients, other radiation approaches—external beam radiation, stereotactic radiotherapy, gamma knife radiosurgery, and brachytherapy (treatment in which radiation sources like seeds are placed in the body)—will remain the best option. A mock-up comparison of different radiation approaches may be done to compare the benefits and risks. McDonald says that proton therapy is not usually used to manage patients whose disease has spread or metastasized or to treat conditions for which other types of radiation either work equally well or better.

Medical Director Mark McDonald (left) and pediatric radiation oncologist Bree Eaton.
As with other types of radiation, patients receiving proton therapy may also undergo surgery, chemotherapy, and/or immunotherapy, each modality potentially enhancing the effectiveness of the other. McDonald anticipates the patients most frequently treated at the Emory Proton Therapy Center will be those with tumors of the brain and spine, head and neck, or lung, or children with many types of cancers for which proton therapy is particularly likely to offer substantial benefit. Proton therapy may be used as part of a clinical trial, in which it is compared against other types of radiation or as a means to collect information on the long-term benefits and side effects and determine the advantages and risks of different options.
Winship physicians have been consulting with appropriate patients at all Winship sites for months, and the first treatments started in December. The center will begin with a single treatment room in operation, another opening approximately three months later, then another and another until all five treatment rooms are up and running. In the first full year of operation, the center anticipates treating close to 400 patients, with the number increasing over time.

Medical physicists calibrate the system to deliver proton therapy with precision.
“One of the best summers of my life.”
As the Emory Proton Therapy Center begins treating patients, Carie LaFond knows just how treatment will go.
In 2006, the Michigan external affairs professional was diagnosed with a rare tumor called a clival chordoma near the base of her brain, pushing on her brainstem. Clival chordomas are known for high recurrence rates; twice, a skilled Detroit neurosurgeon removed her tumor.
When the tumor regrew in 2011, her neurosurgeon recommended proton therapy as having a higher probability of tumor control and better protection of nearby vision and hearing centers and the brainstem. He referred her to McDonald, then at the proton center at Indiana University. LaFond says McDonald was “kind and honest about potential benefits and risks, while also being sensitive to our nine-year-old son’s fears.” The family’s decision was quick and unanimous. Placing their lives on hold, the couple and their two children moved 300 miles to Bloomington where LaFond began almost nine weeks of daily radiation, a longer duration than usual needed to cover every spot of the kiwi-sized tumor and lower the chances of it coming back.
LaFond says that summer remains one of the best of her life. True, every day she went to the center to don a personalized mesh mask and lay down on the table for treatment. As the gantry revolved around her, aiming the beams to her brain as programmed, she felt nothing and heard only the Michael Jackson music her technicians jokingly selected. The radiation itself lasted just a few minutes. The whole session, including set-up, was over in under an hour. LaFond spent the rest of the day biking, swimming, spending time with family and friends who came to visit.
After nine weeks, she went home and back to work, playing basketball with her kids and training for a half marathon.
Today, almost eight years later, LaFond considers herself “the most grateful person on earth.” She serves as a certified American Brain Tumor Association mentor, her way of paying back. She’s pleased that McDonald remains active in proton therapy, the treatment she credits with saving her life.
Falling in love with proton’s possibilities
Like all Winship radiation oncology residents, Mark McDonald’s training was rich in how to calculate and deliver radiation to tumors as precisely and accurately as possible, sparing healthy tissue. When his professors described proton therapy, he knew he wanted to learn more.
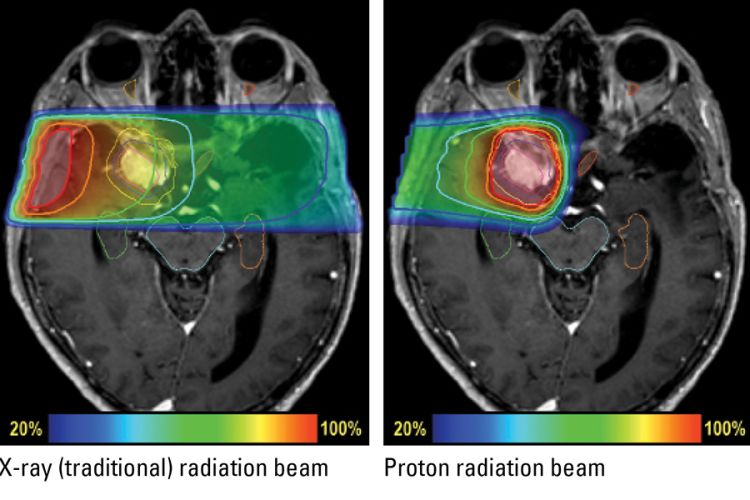
On this MRI of a patient with a meningioma, a slow-growing non-cancerous tumor of the lining of the brain, the tumor appears white and is outlined in magenta while the radiation target is outlined in yellow. The image on the left shows an X-ray beam delivering radiation to the targeted tumor, but also exposing a section of normal brain to low and moderate does of radiation. A proton beam (right) delivers less radiation on the way to the target and concentrates the dose inside the tumor. After reaching the target, the protons stop, delivering little radiation beyond.
In 2009, he joined Indiana University, where a well-established physics laboratory cyclotron had been repurposed to create the first proton therapy center in the Midwest. After intensive training, he “fell in love all over again with the technology’s capabilities.” He treated patients like LaFond, served as principal investigator for a new proton therapy patient registry, and conducted research on outcomes and side effects.
In 2015, the former Winship chief resident was recruited as medical director of Emory’s new center. Begun in 2013, the Emory Proton Therapy Center had been put on hold after a terminated relationship with the original developer. In 2015 it was back on track as a not-for-profit center, a good fit, says McDonald, with Winship’s mission. The Georgia ProtonCare Center owns the facility and manages financial operations. Winship and Emory Healthcare are responsible for all medical care.
While treating patients with cancers of the head and neck, brain and spine, gastrointestinal system or lung, McDonald also began organizing operating procedures and helping recruit and train faculty and staff for the new center. He will spend most of his time at the center but continue to see patients at Emory University Hospital Midtown. Other Winship radiation oncologists will spend part of their time at the new center, but continue to treat patients at other Winship sites. This back and forth is important, McDonald says, because other radiation treatments will be the best option for some patients and because physicians working in the new freestanding facility need to stay connected with their peers.
Staying close to home
Now Georgians like Barry Elson no longer have to be referred out of state.
In 2004, a team of Winship doctors eradicated the cancer that had begun at the right base of Elson’s tongue and metastasized to lymph nodes on the right side of his neck. Between lymph node surgery, chemotherapy, and intensity modulated radiation therapy (IMRT), Elson telecommuted to England, where the long-time Atlantan was CEO of a global telecommunications company. Treatment was successful. For seven years, follow-up scans were negative. Then, in 2011, the cancer came back, crossed the mid-line to the left tonsil and went north to the left internal carotid artery, which delivers blood to the brain.
Referred by Winship oncologists to M.D. Anderson, then one of very few proton therapy centers in the country, Elson moved to a Houston high-rise apartment for three months. His wife and grown children took turns flying there to spend time with him. For eight weeks, Monday through Friday, Elson donned the personalized mask while proton radiation was directed at the tumors in his head and neck.
That referral saved my life, says Elson. Seven years later, he has mentored 50 newly diagnosed patients, urging them to get a second opinion at a National Cancer Institute-designated comprehensive cancer center like Winship. While traveling out of state for care was difficult, Elson notes “This is not a disease of convenience.” He says the Emory Proton Therapy Center will make life considerably easier for patients like him and for doctors who refer them. As a 14-year patient and survivor, he is pleased to see Winship taking advantage of the knowledge and experience generated at existing proton centers and integrating proton treatment into its existing strong and multidisciplinary programs.
How Protons Work
All radiation treatments work by damaging the DNA of cancerous cells. Traditional therapy does it with X-rays or gamma rays, part of the spectrum of electromagnetic waves that includes radio, microwave, and visible light at one end and the more damaging ultraviolet, X-rays and gamma rays at the other. As these rays – sometimes referred to as photons, with an h– head toward the targeted tumor, tissues before and after the target also receive some radiation. While many advances have lessened the unnecessary radiation delivered to healthy tissues, there is still some radiation delivered outside of the target.
Protons (with an r) are different—and work differently. The positively-charged proton is extracted from the nucleus (center) of a hydrogen atom and accelerated to two-thirds the speed of light inside the cyclotron.
Medical physicist Yuting Lin (pictured right) says the subatomic protons move so quickly and with so much energy that they have few interactions with anything in their path until they reach the tumor, where they slow down and deposit most of their energy abruptly in a phenomenon called the “Bragg peak.” A proton beam concentrates the radiation dose in the target, then stops at the target, avoiding a radiation exit dose and associated damage.
Lin is one of a team of medical physicists recruited from top proton centers around the country. Their work begins before the patient starts treatment, making sure the proton beam is controlled with precision.

Scott and Erica Seaborn were grateful their daughter Kennedy, now four, was able to be treated with proton therapy when she needed it, at age one.
The youngest patients
Thanks to extensive clinical experience and research (including by Winship radiation oncologist Bree Eaton), proton therapy has emerged as a standard of care for young patients with brain, spinal, and certain other tumors. Most insurance companies cover the costs of treatment for children (as does Medicare for older patients)—but the costs of accessing it are born by families, as the Seaborns well know.
Days after her first birthday, Kennedy Seaborn began vomiting sporadically. After nine days with no response to anti-nausea medication, worried parents Scott and Erica carried the lethargic youngster to the emergency room at Scottish Rite, part of Children’s Healthcare of Atlanta (CHOA). Almost immediately, their sweet Kennedy was pumped full of steroids to reduce swelling in her brain. Emergency surgery removed a brain tumor characterized as glioblastoma, and Emory pediatric oncologist Tobey MacDonald started Kennedy on chemotherapy. Reducing the high risk of recurrence required radiation, however, and that was a challenge. While unnecessary radiation to an adult's fully-formed brain can cause some toxicities, in children, it can halt development and cause life-long medical and social problems.
Their pediatric oncologist referred the family to Eaton, who had trained at Massachusetts General Hospital (MGH), the country’s largest center for pediatric proton therapy. Eaton believed the little girl would benefit from proton therapy, and MacDonald agreed. Her parents were fully on board, whatever it took.
And it would take a lot. With the Emory center not yet open, Kennedy was referred to MGH. Erica quit her job and Scott took time off from his family business to stay with Kennedy. On the plane, they shuddered at every cough and sneeze, knowing Kennedy had a weakened immune system. “Treatment here would have been much easier and less stressful,” says Erica. And less personally expensive. The Seaborns were fortunate they could handle travel, housing, and lost-work costs, but Eaton is relieved she now can offer young patients treatment nearer home. “Having proton therapy available in Atlanta makes it a practical option for many more Georgians who would benefit from the treatment,” says Eaton.
Eaton and Natia Esiashvili, another Winship radiation oncologist trained in pediatric proton therapy, will treat children at the proton center while continuing to care for children at Winship. Eaton estimates the two doctors will treat 75 to 100 pediatric patients with proton therapy in the first year, with that number growing as the center ramps up.

Radiation oncologist Bree Eaton with one of her patients, 8-year-old Michael.
Very young children, typically below age seven, may need to be sedated to hold still for treatment. Parents stay with them during setup, hold their hands until they fall asleep, leave for the few minutes of treatment, return as they wake up. If sedation is needed, medical care can take an hour or more. Daily treatment lasts four to seven weeks depending on diagnosis.
It’s a partnership. Pediatric oncologists and radiation oncologists work together to follow young patients and monitor for tumor response and side effects. With parents’ permission, children (like adults) are entered into a database combining outcomes information from 13 centers across the nation. As children with cancer become young adults, they transfer their overall care to Winship and a long-term survivorship program headed by Esiashvili.
Three years later, physical and speech therapy are erasing the slight delay caused by Kennedy’s cancer. She returns to CHOA for regular MRIs, images shared with MGH, but her grateful parents often swing by Winship with chocolates.
Looking ahead
Winship Executive Director Walter J. Curran, Jr., himself a radiation oncologist, watched with excitement as proton therapy developed and proved its benefit at centers around the world. What particularly excites him about the Emory Proton Therapy Center is that it opens day one at a whole different level, with new technology simply not available at existing facilities.
That new technology, along with Emory’s clinical and research reputation, has catalyzed recruitment of extraordinary physicians and medical physicists from some of the most experienced proton centers in the country, joining “an outstanding pool of radiation and medical oncology physicians already here.”

Patients at the Emory Proton Therapy Center will be treated by a specially-trained staff of radiation oncologists, therapists, and nurses.
Patients at the Emory Proton Therapy Center will be treated by a specially-trained staff of radiation oncologists, therapists, and nurses.
Research at the center is already underway on how to improve proton therapy, broaden its applications, and expand the understanding of which patients will benefit most from this therapy. Many Winship patients will have access to clinical trials of approaches not available outside National Cancer Institute-designated cancer centers. Moving forward, research will seek to develop treatments that are not just general to a tumor type or location but also personalized specific to individual patients’ biological features.
Proton therapy is here now, in Georgia, and its role in treating patients with cancer is only just beginning.

Debra W. Lockwood (left), president and CFO of Provident Resources Group and Steve Hicks (right), CEO of Provident.
Debra W. Lockwood (left), president and CFO of Provident Resources Group and Steve Hicks (right), CEO of Provident.
How it came to be
Construction started with pouring 36,000 cubic yards of concrete for the 14-foot thick walls that encase the equipment. After the building’s structure was in place, then came delivery of the equipment. Patients will never see this amazing equipment, but they will know from the moment they walk into the Emory Proton Therapy Center that this is not an ordinary treatment facility.
All patient care is handled by Winship physicians and Emory Healthcare staff, but the Emory Proton Therapy Center is owned, operated, and maintained by the Georgia ProtonCare Center, a wholly-owned subsidiary of Provident Resources Group, a national nonprofit organization operated for charitable purposes, including the advancement of healthcare and medical research.
From the moment of its groundbreaking in 2013, the Emory Proton Therapy Center has been heralded as a boon to Georgia’s medical community and to the development of Atlanta’s Midtown neighborhood. Provident and Georgia ProtonCare Center took over the project in 2017 and have overseen the completion of the building and its financial operations.
“Provident is committed to supporting the proton center and making these advanced treatment options available to cancer patients throughout the greater Atlanta region and the state of Georgia,” says Steve Hicks, chairman and CEO of Provident.

Need to know more?
Please visit Winship Magazine, Emory News Center, and Emory University.