Kristan Langdon 04N 06MSN 18DNP moved from Colorado to Atlanta twice to attend Emory’s School of Nursing. The moves paid off for her and her patients as she found a way to improve Emory’s health care system while working on her Doctor of Nursing Practice (DNP) degree.
As clinicians around the country are well aware, reducing hospital admissions is one of the fastest ways to improve patient care and reduce health care costs. On average, 15 to 25 percent of people discharged from hospitals are readmitted within 30 days or less, many of which are preventable, notes the Center for Healthcare Quality and Payment Reform on its website.
Langdon tackled the problem in her own practice and dramatically reduced hospital readmission rates and costs for cardiology patients at Emory Clinic. The key: putting nurse practitioners in charge of transitional care mangement—including post-discharge clinics—for patients.
“There was a big disconnect between people coming out of Emory University Hospital (EUH) and getting into the clinic for follow-up care,” says Langdon. “When patients got out of the hospital, they sometimes couldn’t get back to see their physician for a month or two.”
Langdon closed that loop. Cardiology patients now see a
nurse practitioner within two weeks of their hospital discharge. Hospital nurses coordinate with Emory Clinic nurses to contact patients within 24 hours of discharge to schedule a follow-up appointment.
“We wanted nurses at time of discharge to make sure this was done,” says Langdon. “We wanted the hospital nurses to have ownership.”
Results from the first year of data collection were significant. Thirty-day hospital readmissions for cardiology patients decreased by 11 percent, and 58 percent of those seen in post-discharge clinic were less likely to visit the emergency department or be rehospitalized in the same timeframe. The nurse-led post-discharge clinic potentially could save $1.06 million annually in health care costs.
The results are proof of what Langdon’s School of Nursing education helped her accomplish. In particular, her DNP degree amplified her ability to improve health care quality and decrease costs by avoiding duplicate care, using resources more wisely, and working collaboratively across professional lines.
“My degree gave me a platform to try to solve problems within our health care system,” she says. “I have a better understanding of finance, which allows me to speak to both sides of an issue instead of just the care side.”
RISING TO THE TOP
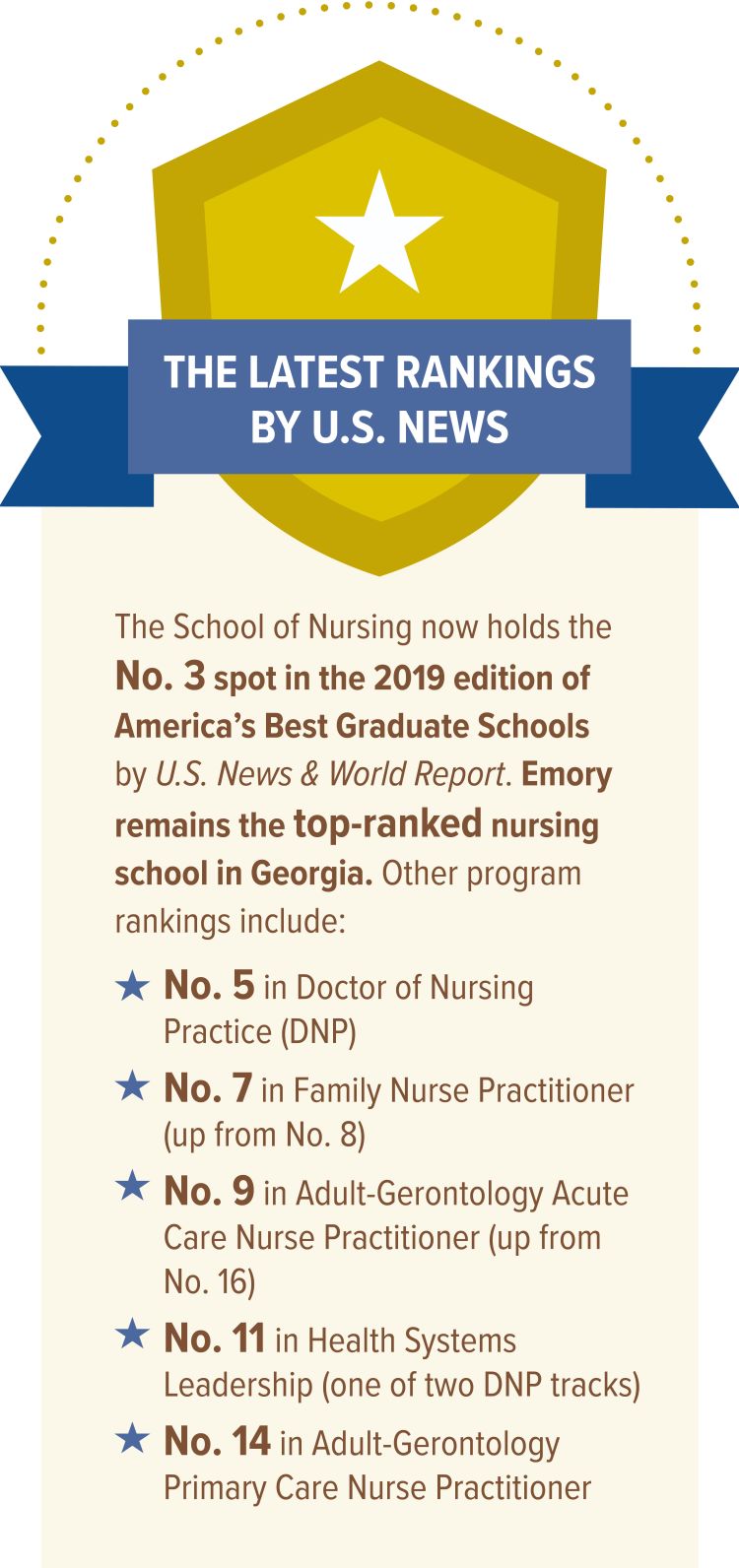
Like Langdon, Emory’s DNP program has come into its own. This year, the program was ranked No. 5 for the first time by U.S. News & World Report. The School of Nursing also rose once again in the latest rankings. It now stands at No. 3 among the 552 nursing schools with graduate and doctoral programs surveyed and remains the top-ranked school in Georgia.
Last year, the school was ranked No. 4 overall, and the year before it was ranked No. 8, both well above its No. 21 ranking in 2015.
A lot has happened in less than a decade to propel the school upward. For the past three years, the School of Nursing has ranked among the top five U.S. nursing schools in research funding from the National Institutes of Health, marking a notable uptick in NIH funding since 2009, when the school was ranked No. 38.
Enrollment is at an all-time high with nearly 1,000 students, twice the number from five years ago. And they do remarkably well. In 2017, new graduates achieved an overall pass rate of 97.5 percent on the National Council Licensure Examination (NCLEX), the final hurdle in obtaining a nursing license. As of August 2018, graduates raised their NCLEX pass rate to 99 percent overall.
Dean Linda McCauley 79MSN PhD RN FAAN FAAOHN attributes the school’s success to several factors. One is Atlanta’s appeal as a vibrant, diverse city where young adults want to study and live. Another is Emory University’s academic reputation and its attractive, walkable campus. Then there’s the School of Nursing itself.
“There are more than 700 schools of nursing in the United States, so students can get an education in many places,” McCauley says. “Students come to study with us because of our faculty, who are at the top of their profession and recognized nationally. When students see the level of excellence in terms of research and clinical faculty, coupled with the phenomenal learning environment at Emory, they come.”
The School of Nursing’s proximity to Emory Healthcare (EHC) hospitals and clinics is also a draw for students. EHC is the most comprehensive health system in Georgia and the largest component of the Woodruff Health Sciences Center (WHSC). Today, more than 7,000 nurses work at EHC hospitals and clinics in Atlanta and surrounding counties. Three of the 10 hospitals in the EHC system have attained Magnet status, the gold standard in nursing excellence.
Other partnerships—Children’s Healthcare of Atlanta, the Atlanta VA Medical Center, the Centers for Disease Control and Prevention (CDC), among them—are equally important. The school offers special programs for students interested in veteran populations, and some of the 200 nurses who work at the CDC often lecture at the School of Nursing.
“These health institutions are our teaching laboratory,” says McCauley. “This is where our students see and feel and touch what they will spend their careers doing. They see and experience these connections. That’s why the nursing school has soared.”
EHC is looking to bring more Emory nursing graduates into its fold. In recent years, the school and EHC have taken steps to bolster Emory’s workforce pipeline by smoothing the transition from student to professional nurse and tweaking the school’s curriculum as needed to meet workforce demand.
“The school’s success benefits Emory Healthcare by providing us with graduates who understand how to be outstanding clinical nurses and where they fit into the patient continuum of care—not just acute care but also ambulatory care and primary care and prevention,” says Sharon Pappas PhD RN FAAN, chief nurse executive for EHC. “They also understand what it means to practice as part of an interprofessional team. They understand a lot of those very important skills and abilities when we hire them.”
Pappas recognized that potential when she joined EHC as chief nurse executive in 2016. Previously a top nursing administrator with Centura Health in Colorado, she accepted the EHC role to lead nursing practice in an academic health system and be closer to family in her native state. “The people and the partnerships that I foresaw convinced me to relocate back to Georgia,” Pappas says.
She found a welcoming colleague in McCauley, whom she had come to know at professional meetings, and in Jonathan Lewin MD FACR, Emory’s executive vice president for health affairs, CEO of Emory Healthcare, and WHSC executive director. All shared a commitment to advancing nursing and patient care at Emory together. But how?
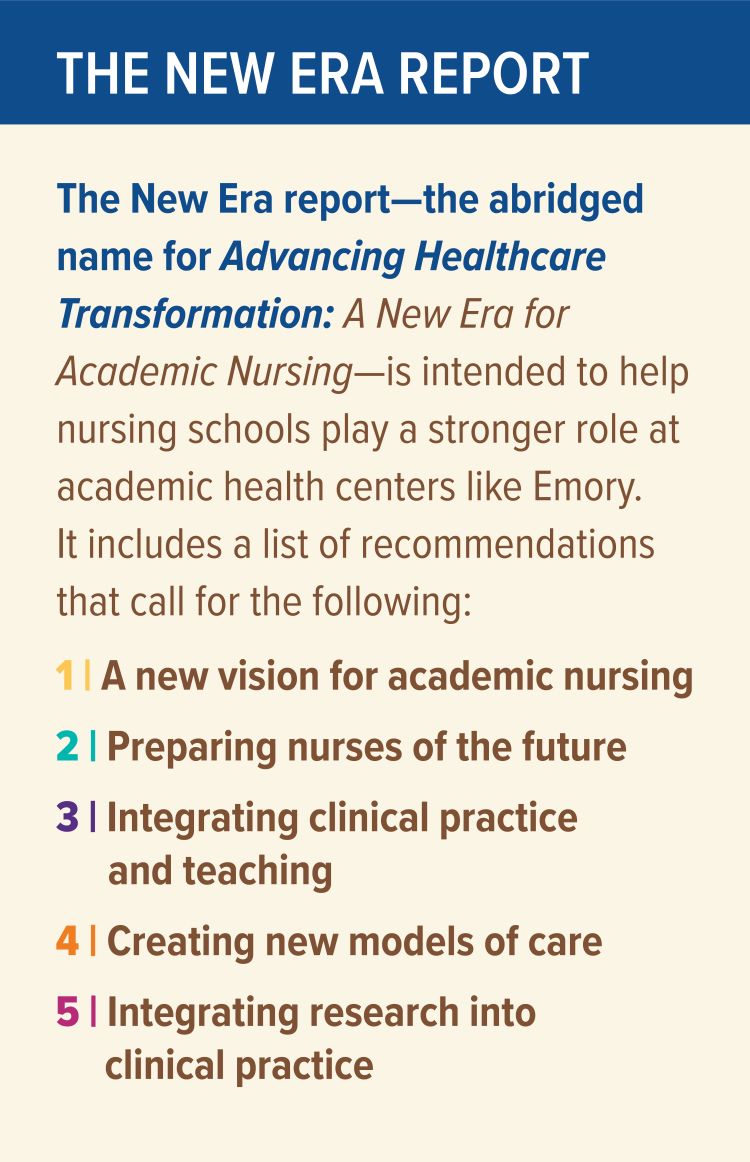
They found inspiration and guidance in a 2016 American Association of Colleges of Nursing (AACN) report examining the link between schools of nursing and nursing practice in academic health centers. When McCauley, Pappas, and Lewin read the report—Advancing Healthcare Transformation: A New Era for Academic Nursing—they embraced it as a roadmap for making the existing ties in nursing education, research, and practice more meaningful.
“Many of the changes we’ve seen here at Emory—a new nursing curriculum, achieving Magnet designation for three of our hospitals, strengthening the nursing workforce pipeline, and expanding continuing education for nurses—started before the report came out,” says Lewin. “We started working to better align nursing education and research with nursing practice at Emory Healthcare from the time we recruited Dr. Pappas. The New Era report validated that what we’re doing is in line with what leaders in the national community think nursing needs.”
Prepared for AACN by Manatt Health, the report is based on interviews with nursing school deans and other health and university leaders at 25 institutions, including Emory. From those interviews emerged a set of recommendations for linking nursing education and nursing practice at academic health centers in new ways.
The larger question, says McCauley, was “how do we work together with the ultimate goal of improving patient care and patient outcomes?”
In 2017, School of Nursing faculty and EHC nursing leaders attended a retreat to generate ideas for transforming health together as full partners in an initiative called “Emory Nursing.”
“It was a good place to start because many of those people have a different relationship today than they did a year ago,” says Pappas. “They have begun to promulgate many ideas.”

Examples abound:
- Noreen Bernard EdD MS RN, EHC vice president for professional nursing practice, and Carolyn Reilly 94MSN PhD CHFN FAHA, associate clinical professor in the School of Nursing, established a leadership scholars program for Accelerated BSN students. Each of the 10 students in the program is paired with an EHC nurse mentor and attends leadership seminars taught by Atlanta-based health care consultant Tim Porter-O’Grady DM EdD ScD(h) FAAN FACCWS.
- Mary Gullatte 81MSN PhD RN AOCN FAAN, EHC corporate director for nursing innovation and research, and Elizabeth Corwin PhD RN FAAN, associate dean for research at the School of Nursing, jointly plan conferences and symposia to encourage more EHC nurses to gather, analyze, and use scientific data in their practice. The latest offering, a one-day symposium, was held at Emory Johns Creek Hospital in June.
- Deena Gilland 18DNP 07MSN RN, EHC vice president and chief nursing officer for ambulatory care services, and Caroline Coburn DNP MS RN, assistant clinical professor, are writing a textbook on ambulatory care to use in the course they co-teach for BSN seniors. The course complements a nurse residency program Gilland established to attract more Emory BSN graduates to the ambulatory care field.
- And there is a concerted effort to hire more Emory-trained nurses to care for EHC patients and families and lead EHC nursing into the future.
“If our school is nationally ranked and also the top-ranked school in Georgia, with stellar graduates who achieve a 99 percent pass rate on the NCLEX, why wouldn’t we work with Emory Healthcare to set a goal for hiring a certain percentage of our students as part of their recruitment goal?” says McCauley.
Recruitment is one of the many points on which McCauley and Pappas see eye to eye, albeit from different perspectives. “We share ownership of each our individual successes,” says Pappas. “We want all boats to rise. That’s the way partnership should work.”
Lewin seconds that belief. “When we recruited Dr. Pappas as chief nurse executive for Emory Healthcare, one of the goals we had in mind for her was to take fuller advantage of the expertise, talent, compassion, and commitment in the School of Nursing and bring it into Emory Healthcare,” he says. “Dr. Pappas and Dean McCauley have worked together to take that from an aspiration to a reality. I don’t think any other nursing school or health care system can claim the same level of synergy between those two parts of the organization as we can here at Emory.”
Langdon is among the many Emory Nursing students and nurses who benefit from that synergy. “The partnership between the School of Nursing and Emory Healthcare is beautiful,” she says. “The support I’ve had from faculty and nursing leaders like Dr. Pappas have made me a bolder person in my statements and vision for what health care could be.”

Enrollment at the School of Nursing is at an all-time high. Nearly 1,000 nursing students will attend Emory this fall.
Enrollment at the School of Nursing is at an all-time high. Nearly 1,000 nursing students will attend Emory this fall.
Interprofessional values
Being part of an academic health center has its advantages for nursing students and nurses.
At Emory, the School of Nursing is part of the Woodruff Health Sciences Center (WHSC), which includes Emory Healthcare (EHC), the School of Medicine, Rollins School of Public Health, Winship Cancer Institute, Yerkes National Primate Research Center, and Emory Global Health Institute.
“Clearly, academic health centers have an edge because they have a formal partnership structure,” says Dean Linda McCauley. “A lot of other nursing schools don’t have that. Emory’s got a well-stocked kitchen in terms of nursing, medicine, allied health, and public health to cook this gourmet meal of how nursing and interprofessional education should take place.”
Jonathan Lewin, executive vice president for health affairs, recently announced a strategic plan that will carry WHSC into the future. The plan revolves around five key themes: constructive culture, interprofessional education and collaborative practice, transforming models of care, innovative discovery, and data science. All relate to WHSC’s partners, including the School of Nursing and EHC.
Of all the assets that nursing faculty and students and EHC nurses and nursing leaders bring to WHSC, one in particular tops Lewin’s list.
“What nurses do remarkably well is connect with patients,” he says. “The compassion they bring to their work is so important at any level across the nursing spectrum. It’s not just about numbers, budgets, or staffing levels. It’s about patients and families.”
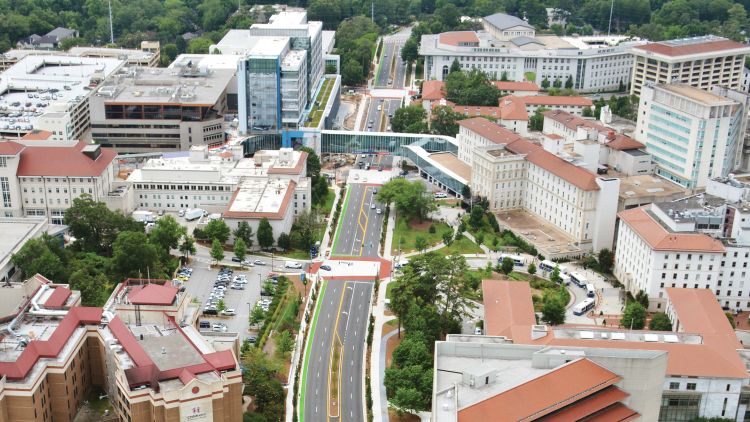
Photo: The Woodruff Health Sciences Center on Clifton Road

Want to know more?
Please visit Emory Nursing Magazine, Nell Hodgson Woodruff School of Nursing, Emory News Center, and Emory University.