RECALIBRATE
The Making of a TACTICAL PHYSICIAN


One summer when he was almost 45, Jeremy Ackerman enrolled in a police academy near his home in Atlanta.
On the first day of class, the instructor asked students to introduce themselves with the nickname they preferred. Ackerman’s sounded like something from an old movie: Doc.
“Why do they call you Doc?” the instructor asked.
“Because I’m a doctor,” Ackerman answered.
“We’ll talk later,” the instructor said, not sure whether he was being pranked or looking at one of his best-educated recruits.
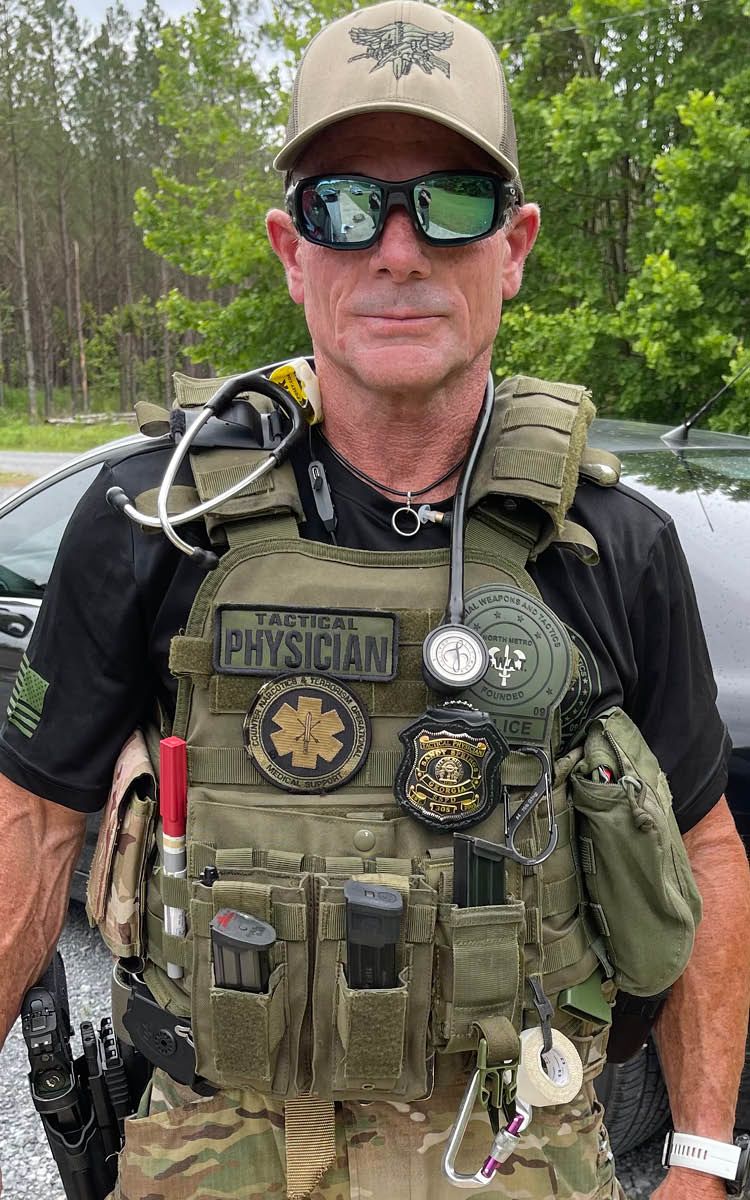
Jeremy Ackerman is indeed a doctor and an associate professor of emergency medicine at Emory’s School of Medicine, who works three or four shifts a week in the Grady Memorial Hospital Emergency Care Center in downtown Atlanta. He’s also a tactical physician, a sworn police officer who deploys with a SWAT team and has received a medal of honor for taking part in an operation.
Ackerman can go from scrubs to body armor in the course of 24 hours.
Students in his class on designing medical devices at Georgia Tech, where he has an appointment in the department of biomedical engineering, have grown used to announcements like the one he made from the podium one afternoon this spring.
“No class this Thursday,” Ackerman said. “It’s SWAT Training day.”
Jeremy Ackerman can go from scrubs to body armor in the course of 24 hours.

Ackerman usually comes to the lecture hall wearing tactical pants with multiple pockets that might be hiding a pair of handcuffs. He’s often accompanied by his 75-pound greyhound, Donovan.
“He’s a pretty cool professor,” says Lama Bahanan, a fourth-year student at Tech.
Although Ackerman clearly relishes the excitement of police work, his motivation grows out of broader concerns as a doctor. In the Grady trauma center, he sees victims of gun violence almost every day.
Ackerman believes the discussion about guns in America has become politically treacherous. He also believes that anyone trying to make suggestions about firearm safety ought to know something about firearms.
“In school, they teach you that a doctor has a responsibility to meet patients where they are,” he says, “even if you have a problem with them.”
In Ackerman’s case, it wasn’t hard to empathize with gun owners because he is one. It all started because of a teenage crush.
•••
The way Ackerman talks about shooting, it almost sounds like yoga.
“People think it’s like what you see in action movies,” he says. “It isn’t. Competitive target shooting is a sport about standing perfectly still. You try to control every part of your body so that when you press a tiny lever of metal, a projectile gets launched with high precision through a piece of paper. It’s about being calm and controlling your breathing. We used to meditate and slow our heart rate so we could pull the trigger between heartbeats.”
When Ackerman discovered the zen of shooting as a teenager, no one was more surprised than his parents. The family lived in Bethesda, a relatively liberal suburb of Washington, and his parents supported gun control organizations.
Michael and Judy Ackerman both hold doctorates and achieved high academic positions—he as a biomedical engineer at the National Library of Medicine, she as a mathematics professor who became provost at Montgomery College in Maryland. Then their son came home from high school and said he wanted to learn about guns. He had met someone—his first girlfriend—who was a near-Olympic-level shooter. “Her pick-up line was, ‘You’re the least nerdy guy on the chess team. If you teach me how to play chess, I’ll teach you how to shoot,’” Ackerman says.
In 30 days, he went from never having touched a firearm to becoming a member of the varsity rifle team.
His parents were not overjoyed. “That probably wouldn’t have been the sport of choice in our household,” his mother says.
A fatal tragedy close to home weighed heavily on them. When Jeremy was young, one of his regular babysitters was out of town with her husband when their son discovered the couple’s handgun and started playing with it. He held the barrel to his head and pulled the trigger. It was loaded.
The Ackermans were confident their son would be safety-conscious, however, and as Jeremy grew more interested in shooting, his parents kept an open mind and bought him a competition rifle custom made for a left-handed shooter. He spent two years on the high school rifle team and then drifted away from the sport when he went off to college at Washington University in St. Louis.
Ackerman met a student there who became his wife, and they followed other martial pursuits. “He’s always been interested in different weapon technologies,” says Amber Ackerman. “In college, we did fencing and were on the karate team and did stage combat.”
In the coming years, Ackerman didn’t have time for shooting. He wanted to become an engineer but feared he might end up designing missile systems that killed people.
He remembered a high school friend’s mother who died of cervical cancer and decided he’d rather cure people. He earned two doctorates at the University of North Carolina—in biomedical engineering and medicine—and did his residency in emergency medicine at Stony Brook University Hospital in New York. By the time he took a post at Emory in 2007, he and Amber had started a family.
Their first child, a son, later joined the Boy Scouts and became interested in shooting at summer camp. Ackerman went to the attic and dug out his competition rifle, which he hadn’t touched in years. He restored it—woodworking and metalworking are among his hobbies—and took it to the range with his son.
“I didn’t realize how much I’d missed it,” he says.
•••
Ackerman knows all too well that people with guns can inflict unimaginable heartbreak. He has witnessed the bloody aftermath of firearm violence throughout his medical career. He finds it particularly hard to inform a family that their loved one has died, since gunshot victims are usually young and the death is often sudden and unexpected.
Other cases left him perplexed. When he was a medical student at North Carolina, a man was wheeled in with abdominal bullet wounds that missed a critical artery by a millimeter. It was the sixth time he had been treated for gunshot or stab injuries.
A few days later, when Ackerman was giving him discharge instructions, the patient asked,
“Hey, should I quit smoking?” Ackerman looked at him in disbelief and said, “Sir, it’d probably be better for you to quit getting shot, and then work on the smoking.”
In his clinical rounds at Grady, Ackerman sees everything from sprained ankles and digestive troubles to strokes and heart attacks. He has delivered babies, treated inmates, and helped patients in mental health crisis. Most emergency patients suffer from chronic ailments that are not immediately life-threatening. About 20 percent require admission.
Ackerman prefers to work on trauma cases such as gun injuries. With his knowledge of firearms, he can often recognize injury patterns and reconstruct some of what happened: The type of gun. How the shooter was positioned. Which hand the shooter used to hold the weapon.
“Gunshot wounds can be deceptive,” Ackerman says. “Wounds from slow-moving rounds can look terrible but they’re probably less life-threatening. A wound from a fast-moving round can look like no big deal, but when you get inside, the energy from the bullet has caused much more serious damage.”
Ackerman has made safe handling and storage of firearms a particular cause. He took a gun safety course from the National Rifle Association and became an NRA instructor without joining the organization because he has qualms about some of its political positions. When he treats gunshot victims who have accidentally wounded themselves, he can be blunt. “If you own a firearm and end up shooting yourself, I think that really calls into question whether you should own a firearm,” he says.

Lauren Hudak is an emergency medicine physician at Grady and assistant director of the Injury Prevention Research Center at Emory.
Lauren Hudak is an emergency medicine physician at Grady and assistant director of the Injury Prevention Research Center at Emory.
Ackerman found a kindred spirit in an emergency medicine resident he helped mentor. Lauren Hudak earned a master’s from the Rollins School of Public Health at Emory while pursuing a medical degree. She wanted to study firearm safety and violence prevention, subjects that have interested her since an early job with an organ donor network in Tennessee. She drove organs to the Knoxville airport, many of them harvested from people who had died in car crashes or from gunshot wounds.
When Hudak told Ackerman she wanted to bring a public health approach to studying firearm safety, he advised her to learn about guns so she’d know what she was talking about.

Hudak is now an ER doctor at Grady, an associate professor at Emory School of Medicine, and assistant director of the Injury Prevention Research Center.
When she told Ackerman she wanted to bring a public health approach to studying firearm safety, he advised her to learn about guns so she’d know what she was talking about.
Their conversation led to a research project in which they and other investigators interviewed patients at Emory-affiliated hospitals about their firearm practices. As part of the preparation, the doctors invited their surveyors and other medical students to visit the QuickShot range near the Emory campus and shoot guns themselves.
Hudak and Ackerman have published a paper with other Emory researchers about patients’ firearm safety knowledge in the Western Journal of Emergency Medicine, and they plan to do more. But events in the spring of 2022 convinced Hudak that it wasn’t enough just to study the issue.
Mass shootings that killed three dozen people in New York, Texas, and Oklahoma made her resolve to speak out for more stringent gun laws.
“Unfettered access to guns is a risk to our society,” Hudak says, “and we have to do something about it.”
Ackerman believes in a measure of regulation, that not everyone should own a gun and that there needs to be a better system of background checks.
In his view, an epidemic of gun violence is exactly when more academic study of guns is needed. “If you want to solve a problem,” he says, “you start by defining it.”
Mass shootings like the ones that came in rapid succession in 2022 make him value his SWAT team experience even more. “If something happened here,” he says, “I at least have the training to do something about it.”
•••
Ackerman and Hudak wondered whether their work on firearm safety might benefit from a partnership with law enforcement. Ackerman would meet officers in the ER and float the idea. One force in metro Atlanta invited him to come along with its SWAT team to help their efforts in return for providing medical assistance and training. He jumped at the chance.
Tactical physicians are doctors who embed with law enforcement so they can be on the scene during police actions in case officers or others need medical care. Some go through police training and earn a badge, usually on an unpaid volunteer basis, as is the case with Ackerman. Many other medical professionals—nurses, paramedics, physician assistants—also serve in tactical roles.
No one knows exactly how many tactical physicians there are in the United States, but one indication comes from the American College of Emergency Physicians, whose Tactical Medicine Section counts 500 members.
“It’s a slowly growing field,” says the group’s chair, John Wipfler, a tactical physician in Peoria, Illinois, who also works in an ER and teaches at the University of Illinois College of Medicine. “Most doctors don’t want to support their community by stepping into the line of fire.”
Mark Rosing, Emory assistant professor of emergency medicine and ER doctor at Emory University Hospital, deploys with the North Metro SWAT team as a tactical physician.
Mark Rosing, Emory assistant professor of emergency medicine and ER doctor at Emory University Hospital, deploys with the North Metro SWAT team as a tactical physician.
Emory currently has one other tactical physician, Mark Rosing, an assistant professor of emergency medicine and ER doctor at Emory University Hospital who deploys with the North Metro SWAT team. He made the news in 2018 when he testified in the highly publicized trial of Tex McIver, an Atlanta attorney accused of killing his wife. Rosing treated McIver after the incident.
The day he showed up for court, Rosing was in camouflage pants and a SWAT team hoodie, prompting the judge to ask, “May I assume you are not coming from the hospital?” He wasn’t. He had been on a SWAT call. “I would have come dressed as a doctor, but they didn’t tell me I was needed in court until an hour beforehand,” Rosing says.
•••
Ackerman started training with the police but realized when his unit was assigned to provide security for the Super Bowl that he might be a liability in a crisis because he couldn’t carry a gun. The only way to do that legally was to become an officer.
In summer 2019, he juggled his crowded calendar to allow for 408 hours of police academy training. “That’s what he did for his summer vacation,” Amber Ackerman says. “Some of our friends teased him about it. They’d say, ‘What kind of midlife crisis is this?’ ”
Ackerman was not the oldest recruit—a handful of recently retired veterans were older—but he was the most unusual one. That was obvious when he failed the academy’s written exam for cardiopulmonary resuscitation (CPR) because he was absent due to being a speaker at an emergency medical conference in Las Vegas on the day of the test.
At first, Ackerman drove his Nissan Leaf to SWAT team training and had some Georgia Tech students help fabricate a gun safe in the back after a fellow officer pointed out that it probably wasn’t wise to store police property in a hatchback. As his gear and personal weapons increased, Ackerman purchased a retired Ford Interceptor SUV from a police department and installed secure storage.
His SWAT training has brought him perspective about how and when firearms are used. He talks about “trigger discipline,” the way police and soldiers are taught not to keep their fingers on the trigger but close by instead, so they don’t fire reflexively.
In a first-person article for the AMA Journal of Ethics, Ackerman described an experience that led him to believe he was doing some good. The SWAT team was sent to arrest a heavily armed suspect with a record of violent crime. After the police took the suspect into custody without incident, an officer told him, “Doc, when you’re here, it’s easier to keep my finger off the trigger.”
•••
Ackerman has participated in more than 90 SWAT team operations, typically high-risk warrants served in the pre-dawn hours when the chances of resistance and collateral damage are lowest.
In March 2022, Ackerman was awarded the department’s Medal of Honor, the highest honor the department grants. “This was in recognition of bravery and heroism while attempting to overcome a violent armed individual who had barricaded himself in a home with multiple firearms and explosives,” reads the notice from the American College of Emergency Medicine.
For the past two years, Amber Ackerman wasn’t sure which was riskier: her husband working in a public hospital ER during the coronavirus pandemic or him deploying with a SWAT team.
“I’m not sure he tells me everything,” she says. “I’m not sure I want him to.”
Written by Jim Auchmutey, Photography Jack Kearse, Design Peta Westmaas