Zeroing in on a
mosquito menace
Emory scientists tap big data to target a tiny predator
and the viral diseases it spreads,
including dengue fever and Zika

Mosquitoes are often called humanity’s deadliest predator, since they transmit pathogens that have killed billions of people throughout history. These pervasive insects continue to spread pathogens that kill more than 800,000 people annually and cause many more to suffer debilitating illnesses — mostly in the developing world.
Scientists from Emory University are now leading a new strategy in humanity’s long-running war with the mosquito, using big data to target one species of this tiny disease vector. They have studied the behavior of the Aedes aegypti mosquito, pinpointing where it hangs out in homes. They are mapping cases over time of viral infections that this species can transmit when it bites a human — including dengue fever, Zika, chikungunya and yellow fever. They are zeroing in on high-risk neighborhoods for outbreaks of these diseases in sprawling urban areas of the tropics.
“We’re working on some of the boldest and biggest changes in decades for the surveillance and control of this mosquito,” says Gonzalo Vazquez-Prokopec, associate professor in Emory’s Department of Environmental Sciences.

“The ultimate goal is to give public health officials the power to do more effective and efficient mosquito control — even before an epidemic begins,” says Vazquez-Prokopec, shown with public health technicians in Merida, Mexico, who are preparing to apply a mosquito treatment in a home.
“The ultimate goal is to give public health officials the power to do more effective and efficient mosquito control — even before an epidemic begins,” says Vazquez-Prokopec, shown with public health technicians in Merida, Mexico, who are preparing to apply a mosquito treatment in a home.
The National Institutes of Health’s Division of Microbiology and Infectious Diseases awarded Vazquez-Prokopec a $6.5 million grant to lead a consortium in a randomized clinical trial in Merida, Mexico, as part of the quest to reduce Aedes-borne viral infections. The trial is testing a novel intervention that previous Emory research finds promising: Indoor residual spraying of insecticide, targeted to the places in homes where this mosquito tends to rest.
The Emory team is working closely with scientists from the Autonomous University of the Yucatan, led by Pablo Manrique-Saide, professor of biology, who was also integral to planning the project. The state of Yucatan’s Ministry of Health is another key collaborator.
Aedes aegypti
The researchers safely and successfully launched the ambitious five-year project in 2020, even in the midst of the COVID-19 pandemic.
“It was a huge challenge to adapt all of our procedures, due to COVID, but everything is going to plan, thanks to our outstanding collaborators in Mexico,” Vazquez-Prokopec says. “In fact, our methods may serve as a model for how to safely conduct field research and communicate public health messages during a pandemic.”
Emory co-investigators for the clinical trial for mosquito-borne diseases include Lance Waller, a professor of biostatistics at Rollins School of Public Health, and Matthew Collins, assistant professor in the School of Medicine Division of Infectious Diseases. An expert in viruses spread by mosquitoes, Collins is also on the faculty of The Hope Clinic and the Emory Vaccine Center.
Listen to Pablo Manrique-Saide, from the Autonomous University of the Yucatan, explain the project in Spanish.
Listen to Pablo Manrique-Saide, from the Autonomous University of the Yucatan, explain the project in Spanish.
“Our ability to collect, combine and analyze data is much easier now than in the past and it enables us to do these kinds of studies,” Waller says. “We’re trying to put all the pieces of a complex puzzle together — data on mosquitos, homes that receive and do not receive this method of insecticide treatment, and cases of infections.”
“We’re building on in-depth knowledge about how Aedes-borne disease outbreaks occur and spread in a population,” Collins adds. “Combining data from epidemiology and entomology in a randomized clinical trial will provide the highest level of evidence needed to determine the intervention’s effectiveness.”
The consortium also includes scientists from the University of Florida, the Fred Hutchinson Cancer Center, the University of Washington and the Centers for Disease Control and Prevention (CDC).
Vazquez-Prokopec is a disease ecologist, studying how pathogens jump between species. His work has helped Emory become a global leader in the development of novel tools for mosquito control and the epidemiology of mosquito-borne viruses. For more than a decade, he’s tracked outbreaks of these pathogens in tropical, urban areas in Australia, Peru and Mexico. He uses global information systems to record and map the movements of people, combined with blood tests to determine if they carry one of the viruses. He also maps the locations of the Aedes aegypti mosquito, studying its behaviors and whether it is developing resistance to particular pesticides.
Like the cockroach, the Aedes mosquito is perfectly adapted to live with humans in an urban setting. It feeds almost exclusively on the blood of people and it’s not a good flier, with a range of just 100 meters. The “couch potato” of mosquitoes, its preferred habitat is inside homes, where it rests on the backs of furniture and at the bases of walls. Even the bit of water held by an upturned bottle cap can serve as a nursery for this mosquito’s larvae, which cannot survive colder temperatures.
These characteristics mostly limit Aedes aegypti to tropical and subtropical regions with large areas of densely packed, substandard housing.
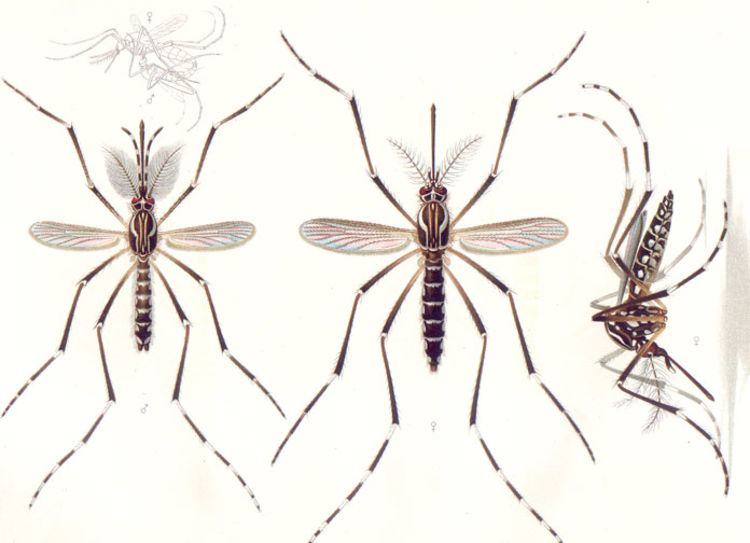
A 1905 scientific painting of Aedes aegypti, which has been a nuisance species in the Americas for centuries. It is sometimes called the yellow fever mosquito.
A 1905 scientific painting of Aedes aegypti, which has been a nuisance species in the Americas for centuries. It is sometimes called the yellow fever mosquito.
Aedes-borne viruses are complex. Many people infected with them do not show symptoms, although they can still play a role in transmission.
Dengue fever is further complicated by the fact that it occurs in four different types. Nearly one hundred million people a year are sickened by it, according to the World Health Organization (WHO). Symptoms can include fever, nausea, vomiting, rash, aches and pains. About 40,000 people die of the illness in a typical year, and hundreds of thousands are hospitalized with it, making it one of the costliest diseases affecting the developing world.
“There’s a reason that dengue is nicknamed ‘break-bone fever,’” Vazquez-Prokopec says. “It can be excruciating and you don’t want to get it.”
WHO classifies dengue as a “neglected tropical disease” because it generally affects the poor and has not received much attention relative to its toll.
The emergence of the Zika virus in 2016, however, put Aedes-borne diseases in the world spotlight. Zika swept through Brazil like a flash fire, leaving a trail of birth defects in its wake. The virus, it soon became clear, could penetrate the placenta of a pregnant woman and harm the brain of the fetus. Tragic images of newborns with smaller-than-normal heads riveted the world’s attention on the perils posed by the Aedes mosquito.
“There has always been a desperate need for better methods of mosquito surveillance and control, but the Zika outbreak clearly showed the current limits,” Vazquez-Prokopec says.
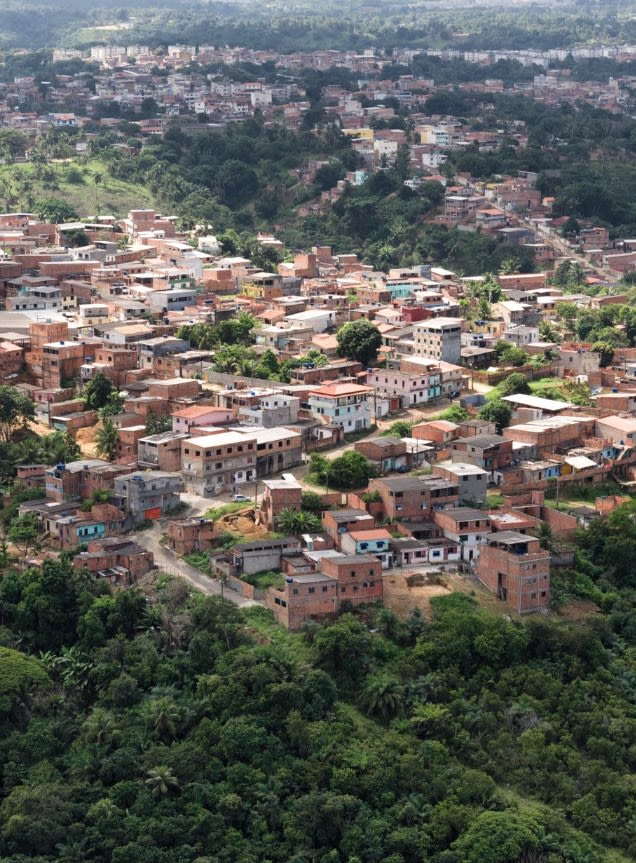
Salvador, Brazil, was hit hard by the Zika virus. Overcrowding and poor sanitation create ideal conditions for the Aedes aegypti mosquito that carries the virus. (Photo by Uiler Costa)
Mosquito control generally involves outdoor spraying of insecticides — by airplanes, trucks or hand-held foggers — to cover broad swaths of a city quickly. Outdoor spraying is not effective for the Aedes aegypti mosquito, however, since its preferred habitat is indoors.
Vazquez-Prokopec and colleagues began investigating different tactics, such as indoor residual spraying. “It’s a novel but rational approach, based on the behavior of this mosquito,” he says.

A public health technician in Cairns, Australia, gathers mosquito larvae from water pooled on a tarp, during a dengue fever outbreak.
A public health technician in Cairns, Australia, gathers mosquito larvae from water pooled on a tarp, during a dengue fever outbreak.
Their research shows that this method significantly knocks down the population of the mosquitoes by 70 percent or more for months. The drawback is that indoor spraying is time-consuming and labor-intensive — trained public health technicians must enter a home and apply a long-lasting, or residual, insecticide. And, as the global coronavirus pandemic made glaringly clear, public health is often underfunded and under-resourced.
One potential solution is targeted indoor residual spraying, or TIRS, focused just on the areas in the home where the mosquitoes tend to rest. The TIRS approach reduces the time needed to treat a home from about 45 minutes to 12 minutes.
An observational study by the researchers during a dengue outbreak in Cairns, Australia, traced recent contacts of people with a confirmed infection. Contact tracing is commonly used for directly transmitted pathogens like Ebola or HIV — and more recently, for COVID-19 — but rarely for outbreaks spread by mosquitoes. In the case of the Cairns outbreak, contact tracing combined with targeted indoor residual spraying was between 86 and 96 percent effective at reducing dengue cases.
That's more effective than the only vaccine currently available to treat dengue, and that vaccine comes with major restrictions.
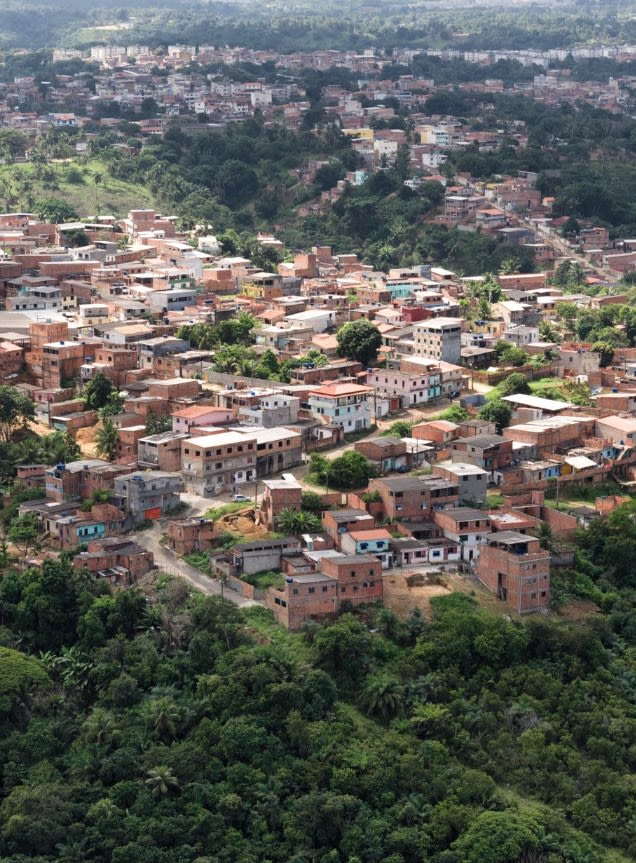
Salvador, Brazil, was hit hard by the Zika virus in 2016. Overcrowding and poor sanitation create ideal conditions for the Aedes aegypti mosquito that carries the virus. (Photo by Uiler Costa)
Salvador, Brazil, was hit hard by the Zika virus. Overcrowding and poor sanitation create ideal conditions for the Aedes aegypti mosquito that carries the virus. (Photo by Uiler Costa)

In 2016, Emory disease ecologist Uriel Kitron gathered Aedes aegypti larvae following the Zika outbreak in Salvador, Brazil. Kitron is a professor in Emory's Department of Environmental Sciences and in Rollins School of Public Health's Department of Environmental Health and Epidemiology. (Uiler Costa)
Emory disease ecologist Uriel Kitron gathered Aedes aegypti larvae following the Zika outbreak in Salvador, Brazil. Kitron is a professor in Emory's Department of Environmental Sciences and in Rollins Department of Environmental Health and Epidemiology. (Uiler Costa)

Aedes aegypti larvae collected in Salvador, Brazil, for study. (Uiler Costa)
Aedes aegypti larvae collected in Salvador, Brazil, for study. (Uiler Costa)

The randomized clinical trial in Merida will provide the gold standard test for the effects of combining TIRS mosquito treatment with data on infections. A city of nearly one million people, Merida regularly endures dengue outbreaks in the summer, and was also hit by chikungunya and Zika.
Vazquez-Prokopec and his collaborators had already mapped the high-risk neighborhoods over an eight-year period. Their data on symptomatic cases of dengue showed that nearly half of them were clustered in 27 percent of the city. And these dengue “hot spots” contained 100 percent of the first Zika cases reported during the Zika outbreak.
The team created a logo for the clinical trial, which is used on flyers, posters and on social media.
The team created a logo for the clinical trial, which is used on flyers, posters and on social media.
Planning for the clinical trial was underway for months. Then, just as the research team prepared to launch the project in the spring of 2020, the novel coronavirus started sweeping the globe.
Suddenly, the already ambitious clinical trial became even more challenging. Many plans went out the window — such as holding large, in-person meetings to familiarize the community with the project.
Instead, the researchers relied more on local radio broadcasts and social media. They established a Facebook page (Proyecto TIRS) where the team regularly posts project updates along with photos, videos and graphics that explain the science. They set up a 24-hour hotline so people could call in and ask any questions and express any concerns.
Gonzalo Vazquez-Prokopec is featured in this video made for the project's Facebook page.
Gonzalo Vazquez-Prokopec is featured in this video made for the project's Facebook page.
Working remotely over Zoom, Emory scientists trained a team of 80 people from the University of Yucatan — including nurses, anthropologists, social workers and others — to go into the field for the recruitment phase. This “ground crew” needed to become well versed in the disease ecology of Aedes-borne pathogens. They also had to adhere to strict safety protocol due to the COVID-19 pandemic.
“They worked from morning to night,” says Oscar David Kirstein, a post-doctoral fellow in Vazquez-Prokopec’s lab and project manager for the clinical trial. “They are an amazing group of professionals, extremely committed. They went house-to-house, knocking on doors, handing out brochures and explaining the project to people from outside their homes. You can imagine how difficult this was, to get people to open their doors and win their trust, during a pandemic."
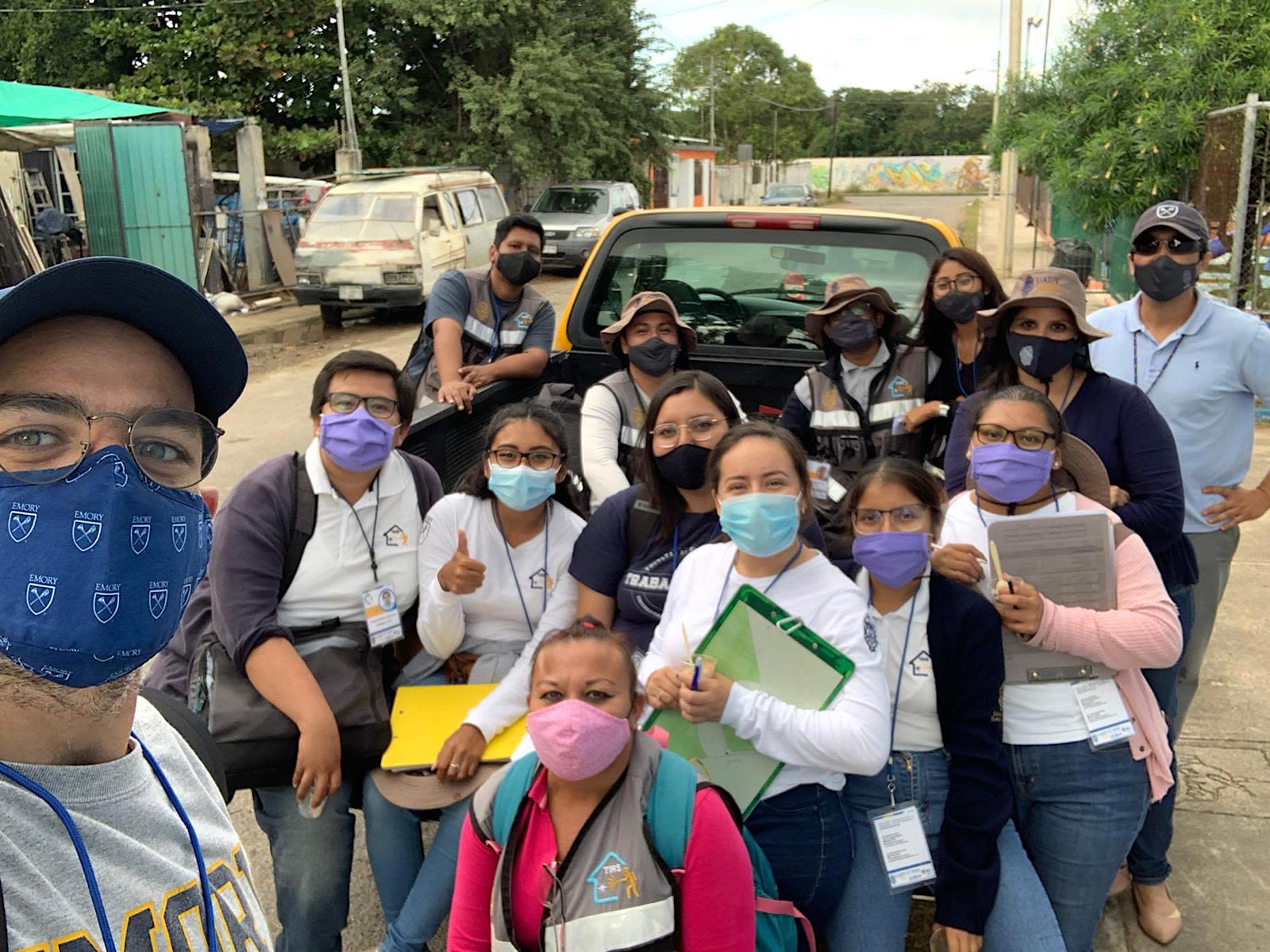


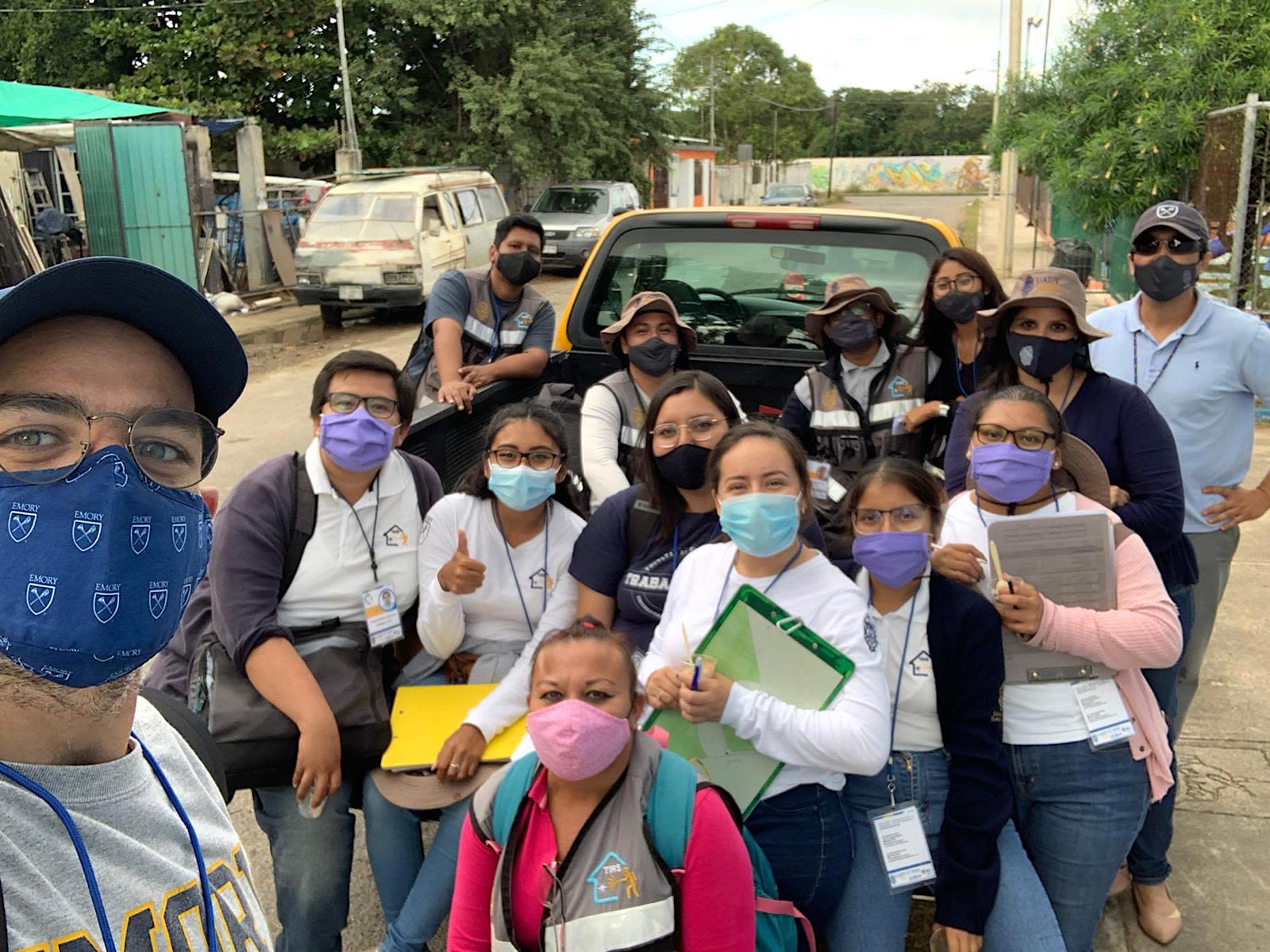
Project manager Oscar David Kirstein (left) takes a selfie with members of the Autonomous University of the Yucatan who worked tirelessly going door-to-door to enroll participants for the clinical trial.
Project manager Oscar Kirstein (left) takes a selfie with members of the Autonomous University of the Yucatan who worked tirelessly going door-to-door to enroll participants for the clinical trial.

"They are an amazing group of professionals, extremely committed," Oscar David Kirstein says of the local TIRS team.
"They are an amazing group of professionals, extremely committed," Oscar David Kirstein says of the local TIRS team.

Preparing to treat a home using the TIRS method.
Preparing to treat a home using the TIRS method.
By March 2021, the team managed to enroll the required 4,600 children, ages two to 15, for the trial, along with thousands more households.
The trial encompasses 33,000 homes within 50 clusters of city blocks that include hotspots for dengue fever. In April, TIRS insecticide treatment by the local health department began in some of these homes. Those houses not receiving the treatment will serve as controls.
Mosquito activity peaks in the warm months of summer through September. The families with children participating in the trial will be regularly contacted for medical monitoring of symptoms of an Aedes-borne disease. Blood draws over the course of the trial will confirm a child’s infection status.
“Many people in the community have been affected by dengue and other Aedes-borne diseases, so they understand the importance of the project,” Kirstein says. “We’re not only doing science. We’re trying to find the best ways to help protect people.”

The recruitment team members for the clinical trial went to individual homes to explain the project, adhering to strict protocols for masks and distancing.
The recruitment team members for the clinical trial went to individual homes to explain the project, adhering to strict protocols for masks and distancing.
Like Vazquez-Prokopec, Kirstein is a native of Argentina. He was born in the northern part of the country where dengue fever is endemic. “An outbreak of dengue exploded there about 12 years ago,” he recalls. “I’m fascinated by mosquitoes and the pathogens they carry because the strategies they find to adapt and thrive are amazing. Every organism needs to be respected and understood in the way that we respect all of life. Outbreaks of infectious diseases are often linked to our own behaviors in upsetting the balance of the natural environment.”
Even more pathogens will keep popping up and turning into household names as the climate warms, humans keep expanding into wildlife habitats, and more places in the world undergo rapid urbanization.
“We’re going to need a battery of different weapons to control mosquitoes and fight existing and emerging Aedes-borne diseases,” Kirstein says. “Our clinical trial is an incredibly important step. It will provide a massive amount of data with the potential to not only benefit Merida, but to help people in many places in the world.”
“The time is right to embrace the full complexity of mosquito control and disease-transmission dynamics,” Vazquez-Prokopec adds. “We now have good baseline data, and the necessary computer power, to develop more complex models to help contain outbreaks.”
Story and design by Carol Clark
To learn more:
The Prokopec Lab, TIRS Project, Emory Department of Environmental Sciences, Rollins School of Public Health, Emory School of Medicine
Media inquiries: Carol Clark, 404-727-0501, carol.clark@emory.edu