THE WAY FORWARD—Public Health
A ‘PRACADEMIC' APPROACH TO THE PANDEMIC
An epidemiology expert embedded with the Fulton County Board of Health, Emory faculty member and alumna Allison Chamberlain helped shape the local response to COVID-19 while giving public health students invaluable practical experience in fighting a pandemic.

Allison Chamberlain 15G calls herself a pracademic. That is, she splits her time between working as a research associate professor at Emory’s Rollins School of Public Health and as an epidemiology consultant for the Fulton County Board of Public Health. Three days a week at Emory, she’s teaching students about emergency preparedness and epidemiologic study design, as well as guiding critical research. The other two, she’s putting her expertise to practice by helping local and state government in its COVID-19 response—from conducting case investigations to analyzing key data.
Her close partnership with Fulton County, stemming back to 2017, helped Emory win a grant last June from the Robert W. Woodruff Foundation to create the Emory COVID-19 Response Collaborative (ECRC). Chamberlain serves as the collaborative’s director, and its mission is to place Rollins faculty, staff, and students into the service of public health departments throughout Georgia to help in the fight against the pandemic.
“It’s a scary but also an unbelievable time to be in public health,” Chamberlain says. “For many of our students, and our faculty, it’s a rare opportunity to participate directly in a major public health emergency. Students in particular are learning firsthand how to do contract tracing, case investigations, data analytics, outbreak response, and research. And they’re gaining invaluable lessons in community engagement—how to build rapport and trust with the public.”
Opening young minds to the fieldwork of public health, especially during a pandemic, bodes well for the future, she says. “It’s a potentially career-changing experience for them,” Chamberlain says. “Many may very well go on to work on the ground for local and state public health departments, armed with what they’ve learned from battling COVID-19.”
Emory Magazine found a break in Chamberlain’s busy schedule to ask her more about how she, her fellow faculty members, and her students have been making real, positive impacts in Georgia’s response to the COVID-19 pandemic.
“It became even more difficult as the pandemic raged on. We were under the assumption that people would want to talk to public health authorities and answer their phones when we called, but we didn’t factor in the stigma of contracting COVID-19 and the ramifications of having to be quarantined or isolated.”
Q: How did you first get involved with the Fulton County Board of Public Health?
Allison Chamberlain: I came on board as a faculty member at Rollins in 2015 after graduating from the doctoral program in epidemiology. However, something was missing in my work and I couldn’t quite put my finger on it right away. I knew it had something to do with the application of my research to broader communities or to direct practice. And there was an opportunity that arose, when Kathleen Toomey, who now serves as Georgia’s state commissioner of health, was the health district director for Fulton County. She was looking for some help to analyze some of their epidemiologic data that the county just didn’t have the time or the capacity to do. She also wanted to utilize some of the lessons learned from their data to improve their programming. And so I jumped on that opportunity. I had never worked in a state or local health department before and I thought it would be a great chance to apply my research skills while retaining my faculty position at Emory. I’ve been working there since 2017. I got to see how the Fulton County Board of Health operated before the pandemic and knew what its strengths and weaknesses would be when the news started coming about this coronavirus outbreak.
Q: What type of health issues did you help Fulton out with before the pandemic?
Chamberlain: I went in with the idea of learning how they operate, what they were already capable of doing, what type of projects they spend the majority of their time on, and what they would most need from someone like me. It was very clear to me from the beginning that they needed help analyzing data for the purposes of improving their health programs—things like HIV prevention and prevention of other sexually transmitted diseases. These were not my areas of expertise—vaccine promotion and public health emergency preparedness are my bread and butter—but I thought that I’d pivot to be of the greatest help. It was daunting but I learned a lot. I worked with their communicable diseases division to analyze data on risk factors for HIV seroconversion, and to look at risk factors for recurrent syphilis among Fulton County residents. I also helped them conduct their first Pride health surveys—of attendees at the 2018 and 2019 Atlanta Pride festivals—and successfully started getting my students involved with these local epidemiology efforts.

Allison Chamberlain (third from left) and Emory students recruited survey participants at the 2018 Atlanta Pride Festival.
Allison Chamberlain (third from left) and Emory students recruited survey participants at the 2018 Atlanta Pride Festival.
Q: And then the COVID-19 pandemic hit in early 2020.
Chamberlain: Yes. All of a sudden I got thrown right back into my original expertise—public health preparedness, outbreak response, and vaccine promotion. At the very beginning, when there were just a handful of COVID-19 cases in Fulton County, I conducted case investigations on behalf of the health department. I called people whose family members had died from the coronavirus. And that was really hard, but it was very eye-opening in terms of the data we collected—not only their demographics, but also the course of how the illness ran, and details on their pre-existing conditions. And at the time, it was kind of like seeing in advance the tsunami that was going to come to Georgia, to Atlanta. I felt compelled to help the Fulton County Board of Health get ready, as well as to leverage the expertise and capacity we had at Emory. I knew we weren’t going to quell the entire tide, but we would have capable, willing talent at Emory to fight COVID-19. That’s also when I started getting pretty concrete in my thinking about how we could operationalize that assistance from Emory’s faculty, staff, and students, and how the ECRC could get started with the Robert W. Woodruff Foundation’s generous funding.
Q: What have been some of the biggest successes of the ECRC in working with the county and state to build their pandemic responses?
Chamberlain: First, we were able to add considerable epidemiologic expertise to the COVID-19 response by recruiting Emory faculty and students to help. Doing so not only had an impact in speeding up and optimizing how we dealt with COVID-19, but it also formed strong bonds between the university and these local and state public health departments—bonds that will be worthwhile long after the pandemic subsides. Perhaps even more important, we infused our health departments with new, fresh talent who had a desire to get practical experience. This includes 17 early-career epidemiologists who are part of our Rollins COVID-19 Epidemiology Fellows program. They are working in district health departments across our state and at the Georgia Department of Public Health to help with the immediate response and to build the workforce generally. Faculty and students alike also helped conduct analyses of everything from super-spreader events to health- equity issues to vaccine promotion and distribution.
Q: Were there any particular challenges in Emory faculty, staff, and students working with local and state government?
Chamberlain: Navigating the lines between public health practice and university research has been a definite challenge. We have to keep in mind that we’re coming in as a partner in service to them, not leading with a research endeavor. As a research institution, Emory loves to do research. But in a public health emergency like the COVID-19 pandemic, the research has to come second to the immediate needs of our public health partners and the well-being of the general public. But our faculty proved to be exceptional at putting service first. We’ve been able to establish a strong relationship built on trust both locally and statewide, and I think we’ll reap even more benefits of this partnership moving forward. As for other challenges, I’d also say there was definite tension because of how the pandemic response was so heavily politicized. I don’t think any of us in public health were prepared for how politics could play such a major role in dictating whether risk-mitigation strategies to prevent transmission of a highly transmissible infectious disease—like wearing masks—would impact our ability to do our jobs.
Q: What have been some of your biggest lessons learned of being involved so directly in the response to the pandemic?
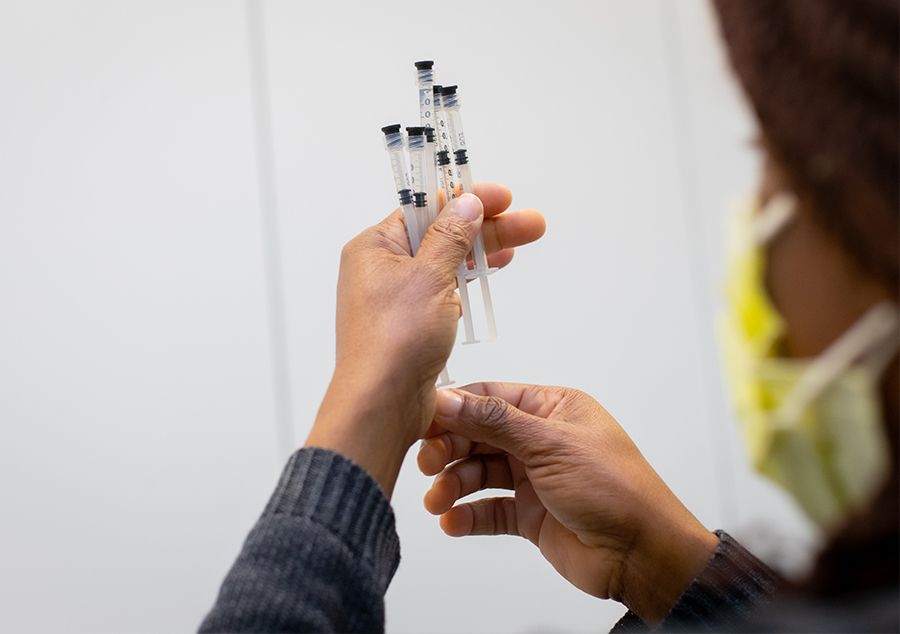
Chamberlain: What I learned is I want to continue exposing our students to the reality of public health practice. I want them to understand how fulfilling careers in state or local public health practice can be after graduating with an MPH or PhD degree. Public health workers—just like doctors and nurses and other medical personnel—have truly been on the frontlines of the pandemic. Collecting all the data of every single COVID-19 case has been a complex and difficult job. And it’s not just about the numbers. It’s about quickly building relationships and rapport—the soft skills you need to connect with other human beings. Asking people sensitive questions about their demographics, their backgrounds, their course of illness isn’t easy. Knowing how to gain trust and to get people to talk to you is a skill you have to build and we need those skills desperately in the field. It became even more difficult as the pandemic raged on. We were under the assumption that people would want to talk to public health authorities and answer their phones when we called, but we didn’t factor in the stigma of contracting COVID-19 and the ramifications of having to be quarantined or isolated. On top of that, the general public became fatigued by all the COVID-19 messaging and outreach. So I’m thankful at this point that vaccines are now widely available and are helping the epidemic curve come down. We need to now focus on getting as many vaccines in arms as possible.
Q: Besides vaccinations, what aspects of the pandemic response are you most optimistic about moving forward?
Chamberlain: I’m optimistic that, from a societal level, people have been forced to better understand what epidemiology is, as well as how the public health system works—and how complex both of them are. I think it will also inspire other foundations like the Woodruff Foundation to support institutions and universities that will work in tandem with our health departments to build up capacity and ability. I also think the pandemic will inspire more young people to come into this field for the right reasons, including never wanting to see their own communities having to suffer through the devastation of an infectious disease like COVID-19 again. Finally, I think continuing to lend the research, teaching, and mentorship talents of faculty from universities like Emory to our public health practitioner colleagues will make us a lot better off when facing any type of future public health threat.
Interview by Roger Slavens. Photos by Stephen Nowland. Art Director: Elizabeth Hautau Karp.