USING A PATIENT'S
IMMUNE SYSTEM
TO FIGHT CANCER

Immunotherapy success stories abound.
Vanishing tumor cells, enduring disease control, longer lives. But not all cancers respond, not all patients benefit, not all the time. NOT YET.
Winship is expanding its research and clinical infrastructure to improve immunotherapy’s power, enhancing outcomes for a greater number of patients. And the cancer world is taking notice.
At Winship Cancer Institute and other leading centers, immunotherapy has taken its place as one of the central pillars of cancer treatment, joining chemotherapy, surgery, radiation, and targeted therapy (drugs that target specific molecular changes driving cancer cell growth and spread). But many questions about immunotherapy call for more research. Why do some cancers — lymphoma, leukemia, melanoma, lung, kidney, or urothelial cancers, for example — benefit while others, like pancreatic, brain, or prostate cancers, are less likely to do so? Why do only subsets of patients have a strong response? Why do some patients experience durable remissions while others quickly develop resistance and the return of their cancer?

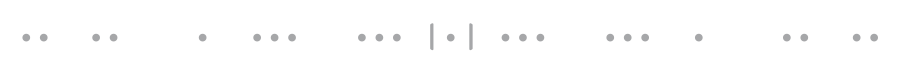
Madhav Dhodapkar
Madhav Dhodapkar
Madhav Dhodapkar, director of the new Winship Center for Cancer Immunology, holder of the Anise McDaniel Brock Chair of Hematology and Medical Oncology, and Georgia Research Alliance Eminent Scholar in Cancer Innovation, says Winship has one of the strongest, best situated research groups tackling these puzzling questions. And it’s getting stronger.
EXPANDED INFRASTRUCTURE. In 2018, Madhav Dhodapkar, a world-renowned expert in cancer immunology and translational immunotherapy, was recruited from a leadership position at Yale as part of Winship’s commitment to expanding its immunotherapy footprint. As head of Winship’s new immunotherapy center, he created a five-year plan. It moved forward at warp speed, most of its to-do list checked off in half that time, including a greatly increased research infrastructure.

Kavita Dhodapkar
Kavita Dhodapkar
Kavita Dhodapkar, a physician-scientist also from Yale (and married to Madhav Dhodapkar) was recruited to be director of pediatric immuno-oncology at Children’s Healthcare of Atlanta. She has played an essential role in building this infrastructure. Today a wide range of new technologies, including those to measure and analyze the immune system, are enhancing already strong research collaborations between Emory and Georgia Institute of Technology. The expanded infrastructure has resulted in an explosion of clinical trials and studies. IT ALSO GOT NOTICED — BIG TIME— IN THE CANCER WORLD.
THE NCI GIVES ANOTHER BIG THUMBS UP. The National Cancer Institute knows Winship well, having named it as Georgia’s only NCI-designated comprehensive cancer center. This year, the NCI formally recognized Winship’s cancer immunology research program as having enough investigators, clinical trials, experience, grants, and other resources to be designated as an independent research program. The research program’s co-leaders, Madhav Dhodapkar and Rafi Ahmed, director of the Emory Vaccine Center and Georgia Research Alliance Eminent Scholar in Vaccine Research, reflect Winship’s successes across the growing field of immunotherapy. Winship now officially has four recognized independent research programs: cancer immunology, developmental therapeutics, cancer prevention, and cell and molecular biology.
BUILDING ON SUCCESS

Cancer develops when the immune system fails to recognize or sufficiently attack mutated cells. Immunotherapy is designed to harness and strengthen the immune system’s ability to get the job done.
Winship gets its power and potential, says Dhodapkar, from its extensive track record in understanding the immune response and in developing, testing, and providing clinical care in the two basic approaches active in immunotherapy today: checkpoint inhibitor therapies, sometimes called checkpoint blockade therapies, and adoptive cellular therapies.
Rafi Ahmed
Rafi Ahmed
In fact, the first of those areas— checkpoint inhibitors — is based in part on findings by Rafi Ahmed and his colleagues in the Emory Vaccine Center, who showed that T cells become functionally exhausted due to inhibitory proteins, like PD-1, that put the brakes on the immune response. Their fundamental discoveries led directly to development of drugs to block those inhibitory proteins, taking the brakes off the immune system and letting it get back to doing its job. Ahmed’s original work focused on chronic viral diseases like HIV or hepatitis, but once scientists realized cancer cells also developed inhibitory proteins, a new era of cancer immunotherapy sprang into being. New checkpoint drugs produced dramatic and often long-lasting responses in some cancer patients. For example, the vast numbers of patients with advanced melanoma who responded to one of the first PD-1 blockade drugs — including former President Jimmy Carter, who was treated at Winship — are alive today. Today, Ahmed and his lab focus half their efforts on cancer.
Increasingly that means designing and testing combinations of the original blockade drugs with other drugs or therapies, such as the combination that changed William Avera’s life.

TAKING AIM AT MULTIPLE TARGETS

Avera had spent years as a painter, most recently in the Marine Corps Logistics Base in Albany, Georgia, where ground combat and support equipment is rebuilt and repaired. The diagnosis of advanced stage IV colon cancer slowed him down. Radiation and chemotherapy brought him to his knees. He lost half his weight. He couldn’t stand up. In 2016, he referred himself to Winship for a second opinion. He got something even better.
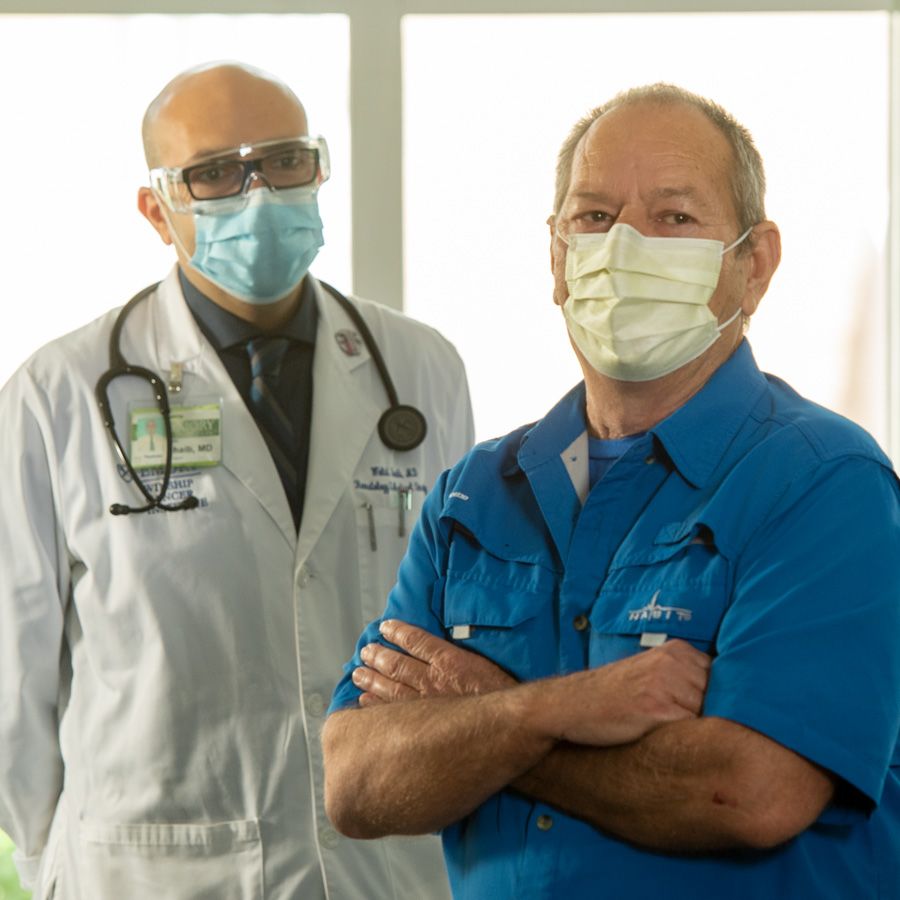
Walid Shaib with his patient, William Avera
Walid Shaib with his patient, William Avera
Walid Shaib, a specialist in gastrointestinal malignancies and a member of Winship’s Discovery and Developmental Therapeutics Research Program, believed the 64-year-old was an excellent candidate for a clinical trial combining two immunotherapy drugs. Genetic testing at Winship showed that Avera’s cancer was high in micro-satellite instability (MSI), breaks in repeating stretches of mismatched DNA, a feature found in 10 percent to 20 percent of colorectal cancers. MSI-high tumors have an inability to repair the genetic material (DNA), which leads to a high mutation rate, making these tumors especially susceptible to immunotherapy.
The trial in which Avera was enrolled combined nivolumab (Opdivo) and ipilimumab (Yervoy). Both drugs block proteins that keep immune cells from properly recognizing and killing cancer cells. Nivolumab targets PD-1. Ipilimumab targets CTLA-4. Blocking CTLA-4 activates T cells specifically aimed at cancer cells.
Almost from the beginning, Avera called the treatment “magic.” His tumors began to shrink. He felt better. And better. He had what doctors call a complete response. It’s been four years now since his treatment ended, and there are no signs of cancer in his body. His weight, down to 95 pounds, is back to his usual 195. He is again able to take care of his 95-year old mother, spend time with family, and do once impossible activities like replacing a blown motor in his truck. He calls Shaib his hero.
When Avera first arrived at Winship, fearing he was out of options, the FDA had approved double-targeting points in the immune pathway for patients with melanoma and kidney cancer, both immune sensitive cancers. But the combination therapy Avera received was only available to colon cancer patients through clinical trials at centers like Winship.
Since then, thanks to the trial’s good results, it has been approved for advanced stage MSI-high colon cancer. Shaib and his colleagues also use it for stomach, liver and other types of cancers, and clinical trials are studying its use in some cancers that are not immune sensitive, such as pancreatic, other types of colon, and bile duct cancers. Winship recently completed a trial of a combination approach in liver cancer.
The results make Shaib optimistic.
“As we better understand cancer pathways and develop and test new drugs targeting points in them,“ he says, “a cure for cancer no longer seems so far from reality.”

WHY DO COMBINATION THERAPIES WORK BETTER?

Our bodies are designed to have redundancies, explains Bassel El-Rayes, Winship associate director for clinical research and the John Kauffman Family Professor for Pancreatic Cancer Research. That’s good. Having more than one way to get things done — two eyes, lungs, lobes of the liver that work even if part is gone — protects us. Unfortunately, cancers also have redundancy. Not so good. Attack one cancer pathway and another redundant pathway keeps it going. Winship researchers are figuring out those pathways and how best to target them. In more than 50 clinical trials in the gastrointestinal cancer division alone, combinations are making a difference in the patients with cancers of the lung, stomach, intestine, liver, and pancreas.
The most established combination therapies combine a drug that inhibits PD-1 and a second drug targeting another immune checkpoint. Newer combinations add a targeted drug that alters the behavior of the cancer itself. For example, an accepted treatment for liver cancer combines a blockade drug with one that increases blood flow to the tumor, delivering oxygen and nutrients and creating a microenvironment more susceptible to the immune cells. El-Rayes heads a team of five physician researchers who are working to make this particular combination even stronger — and intently watching studies using this strategy for cancers of the stomach, colon, and pancreas. The Winship team is also focused on combinations that include immunotherapy with agents that combat cancer-related inflammation, such as interleukin IL-6. Other Winship studies focus on chimeric antigen receptor (CAR) T-cell therapy that re-engineers a patient's own immune cells to find and kill cancer cells. Winship investigators are involved in research evaluating such re-engineered cells alone or in combination with checkpoint inhibitors to make the re-engineered cells more active, and to target redundant pathways that may allow the cancer cells to escape from CAR T-cell therapy used alone.
“Combination therapy is the future of immunotherapy,” says El-Rayes. “Checkpoint inhibitors and approaches like CAR T-cell therapy used alone let us get our foot in the door. Combination approaches will push it wide open.”

















CELLULAR THERAPIES: ADDING CAR T-CELL THERAPY TO THE FIGHT

Another type of immunotherapy — putting new or improved immune system cells into the body — is not really so new. Bone marrow and stem cell transplantation have been around since the 1970s, replacing a patient’s own weakened or damaged immune cells either with healthy cells from a donor or by returning a patient’s own cells that have been harvested before intense chemotherapy. From the beginning, Winship has been a leader in providing and improving these life-saving transplants.
Today, however, highly personalized adoptive cellular therapies are adding powerful new tools to the cancer-fighting armamentarium. Unlike bone marrow or stem cell transplants, adoptive cellular therapy takes a patient's immune cells and re-programs them to better recognize and attack the antigens on the patient’s own cancer cells. Personalized medicine at its best. The biggest name on the adoptive cell marquee is doubtless CAR T-cell therapy.
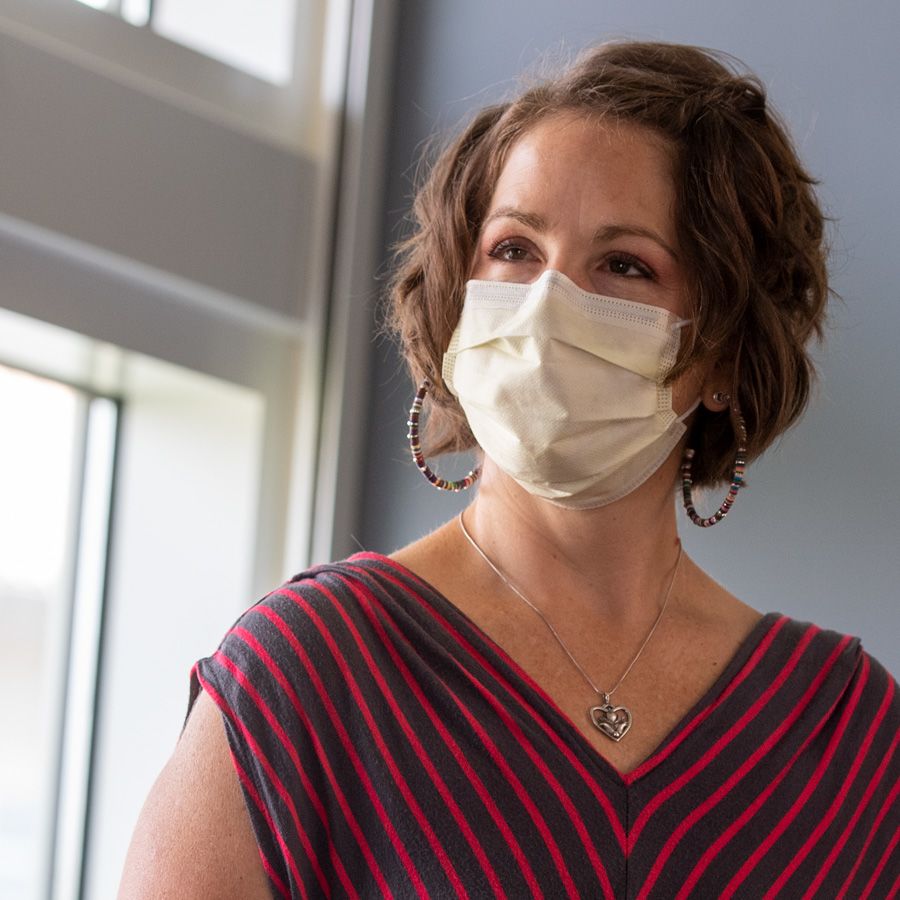
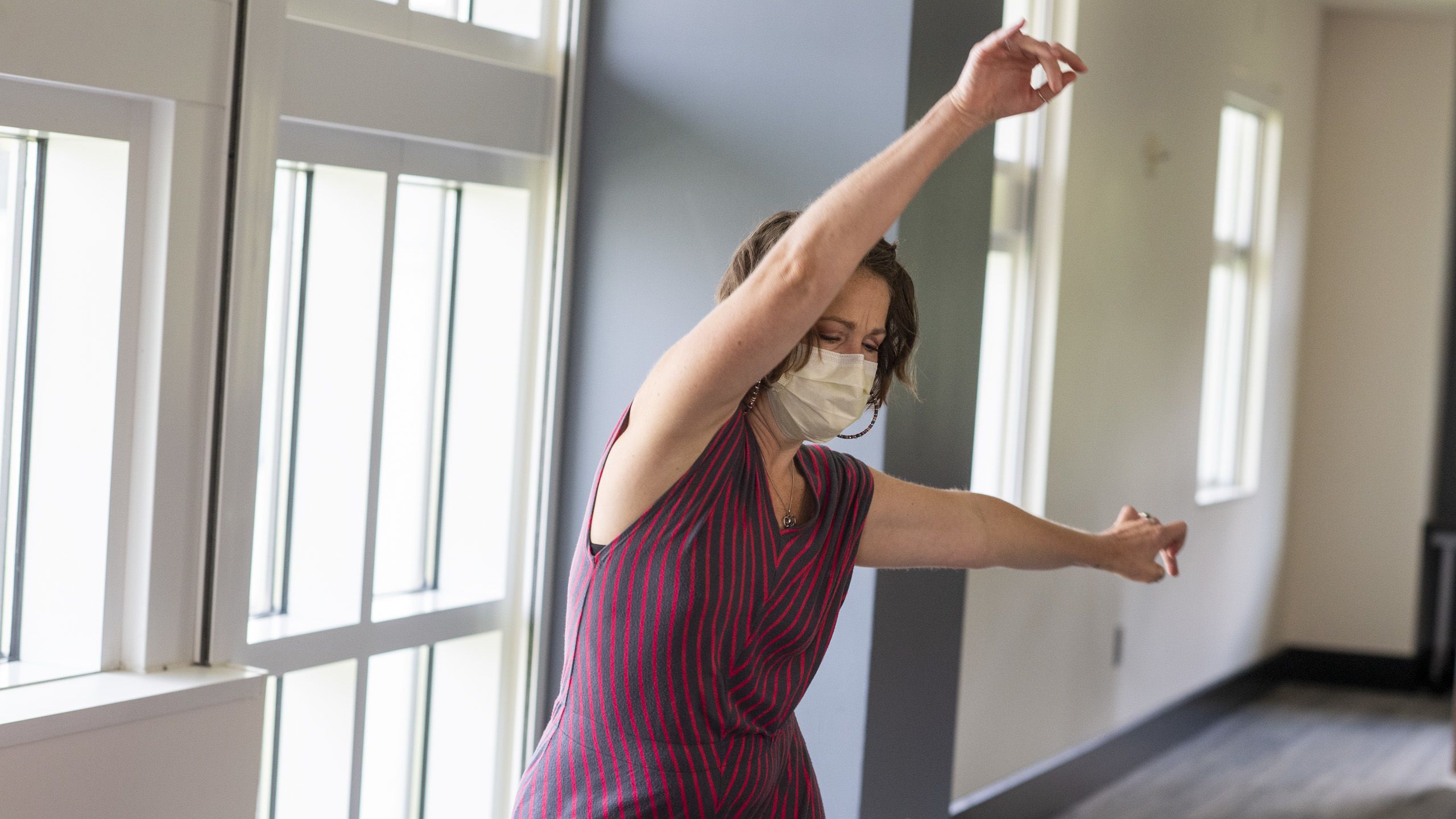
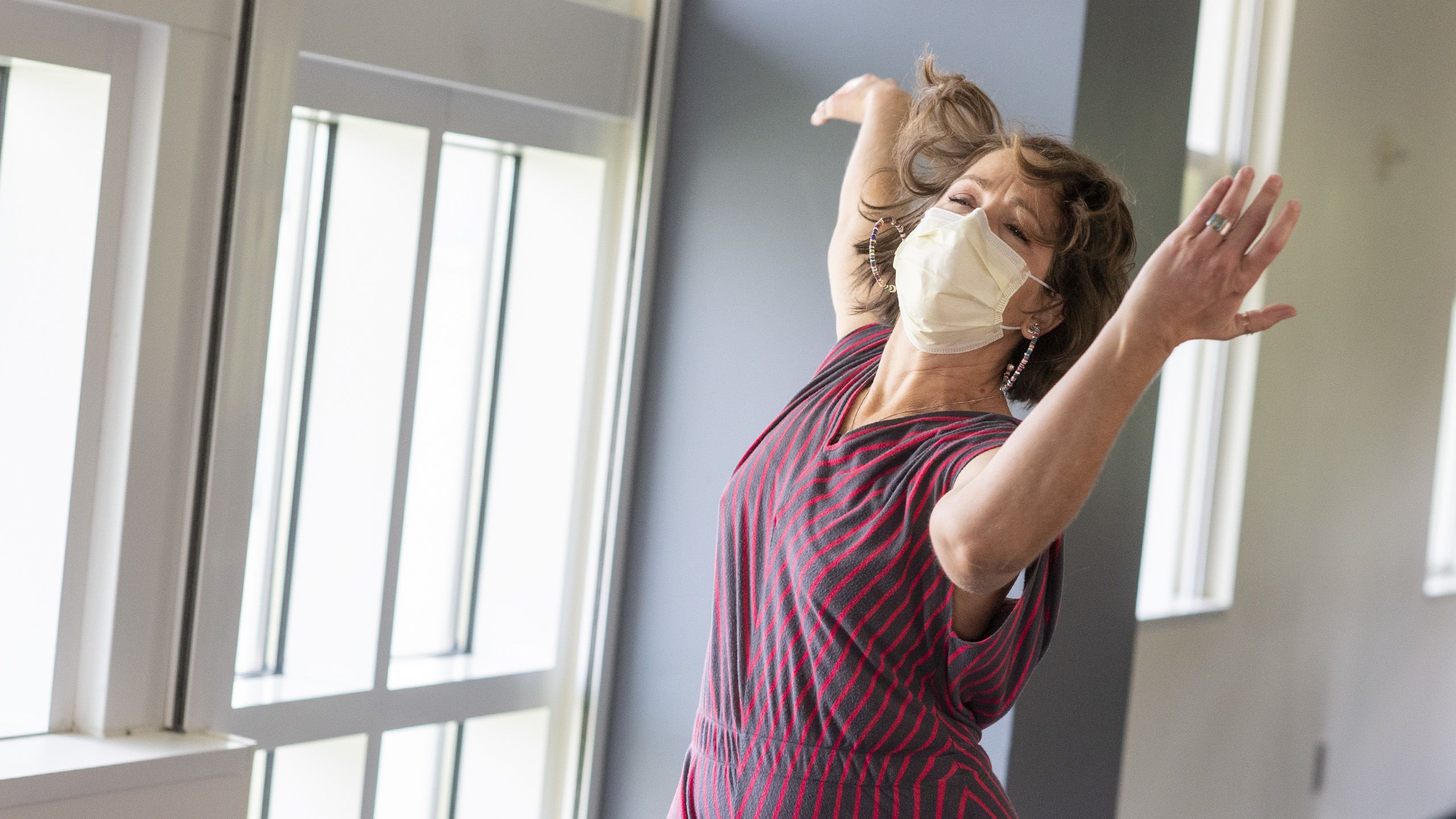
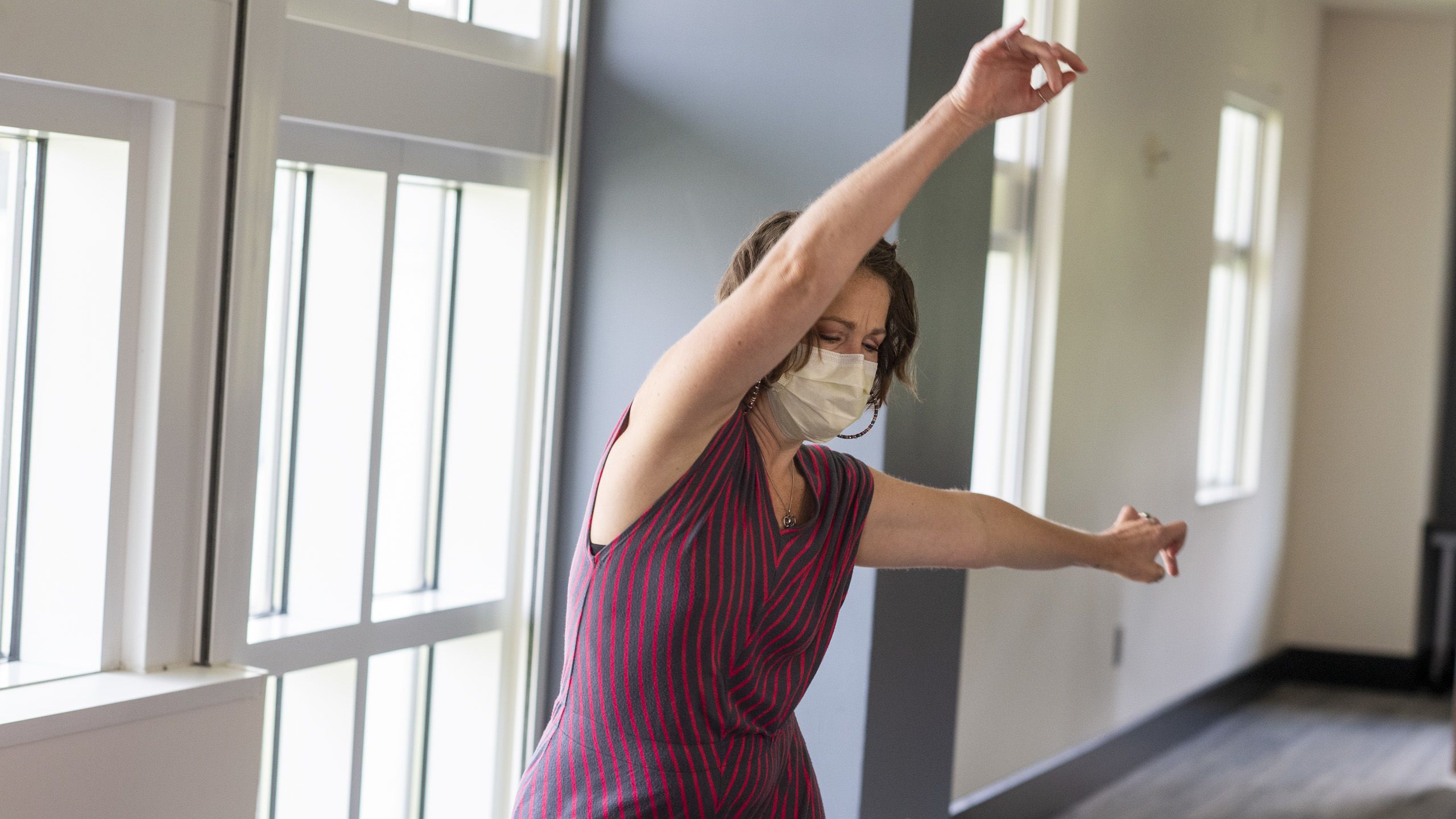
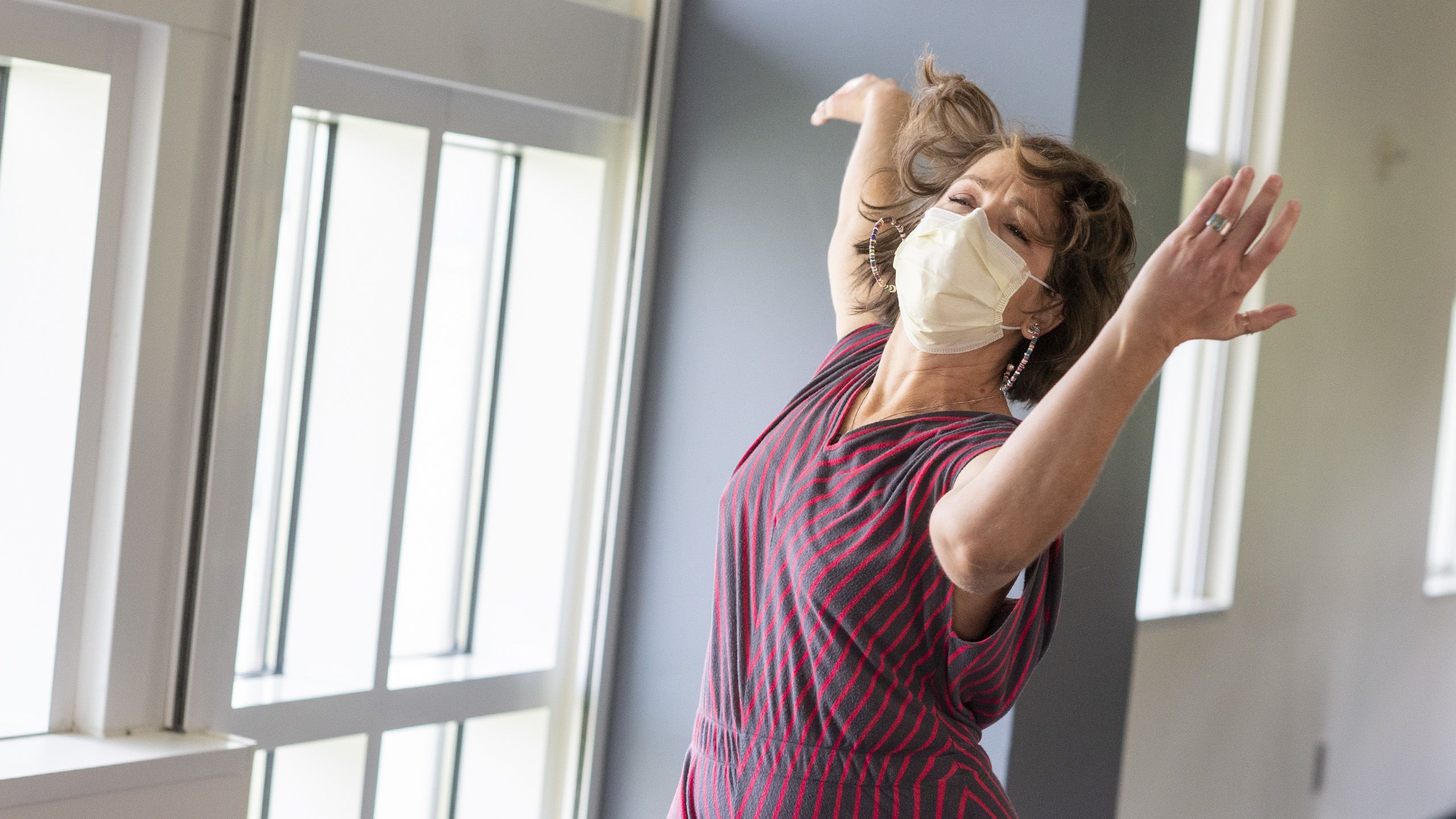
Erika Lundgren
Erika Lundgren
Erika Lundgren was 39 — an energetic dance teacher, volunteer, part-time graduate student — when she began having trouble standing up. Bone marrow biopsy diagnosed ALL (acute lymphoblastic leukemia), a rapidly progressing disease that causes bone marrow to produce faulty white blood cells, crowding out healthy ones. The next months were a blur: first chemotherapy, which failed, then an allogeneic (from a donor) stem cell transplant at the Medical University of South Carolina in Charleston. It wasn’t easy — she apologetically uses the word “hell” — but after almost a year, she returned to work and some semblance of normal life.
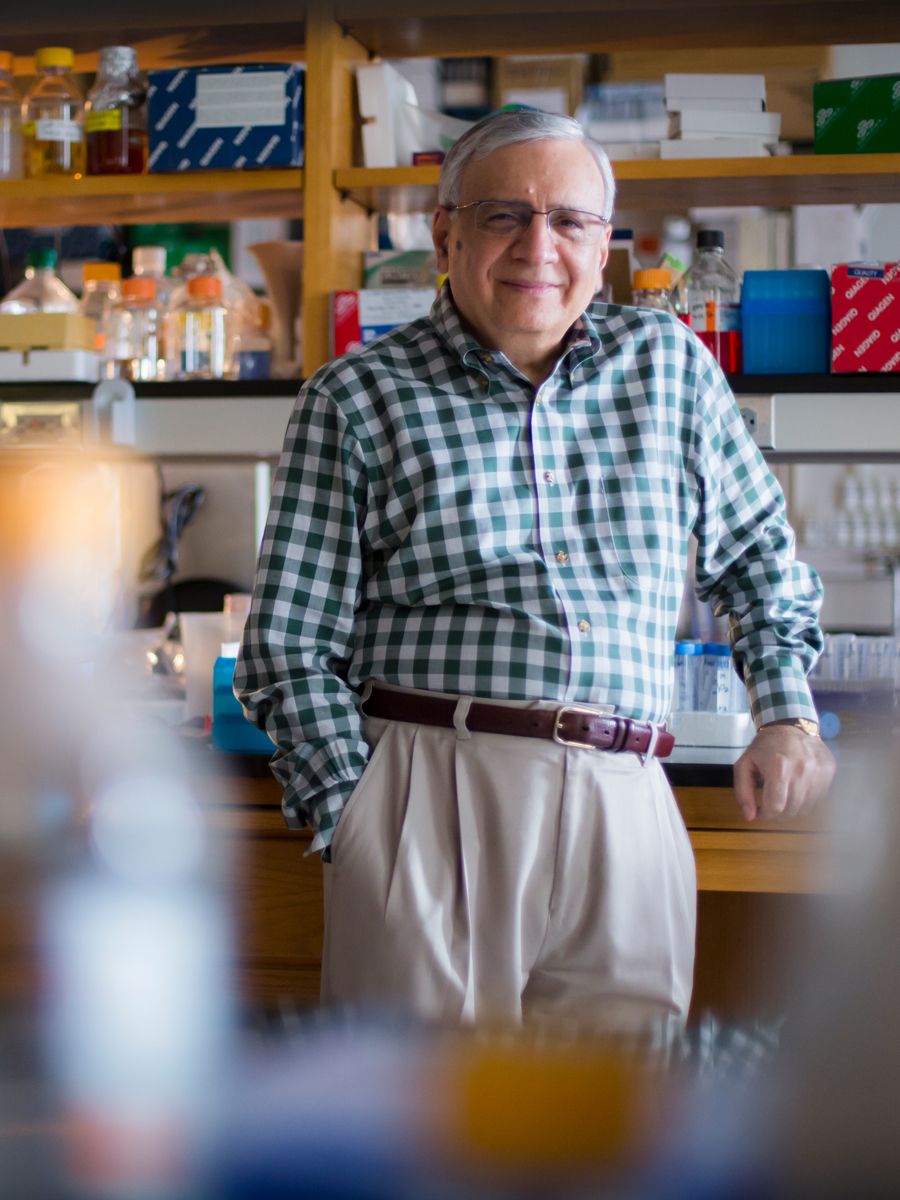
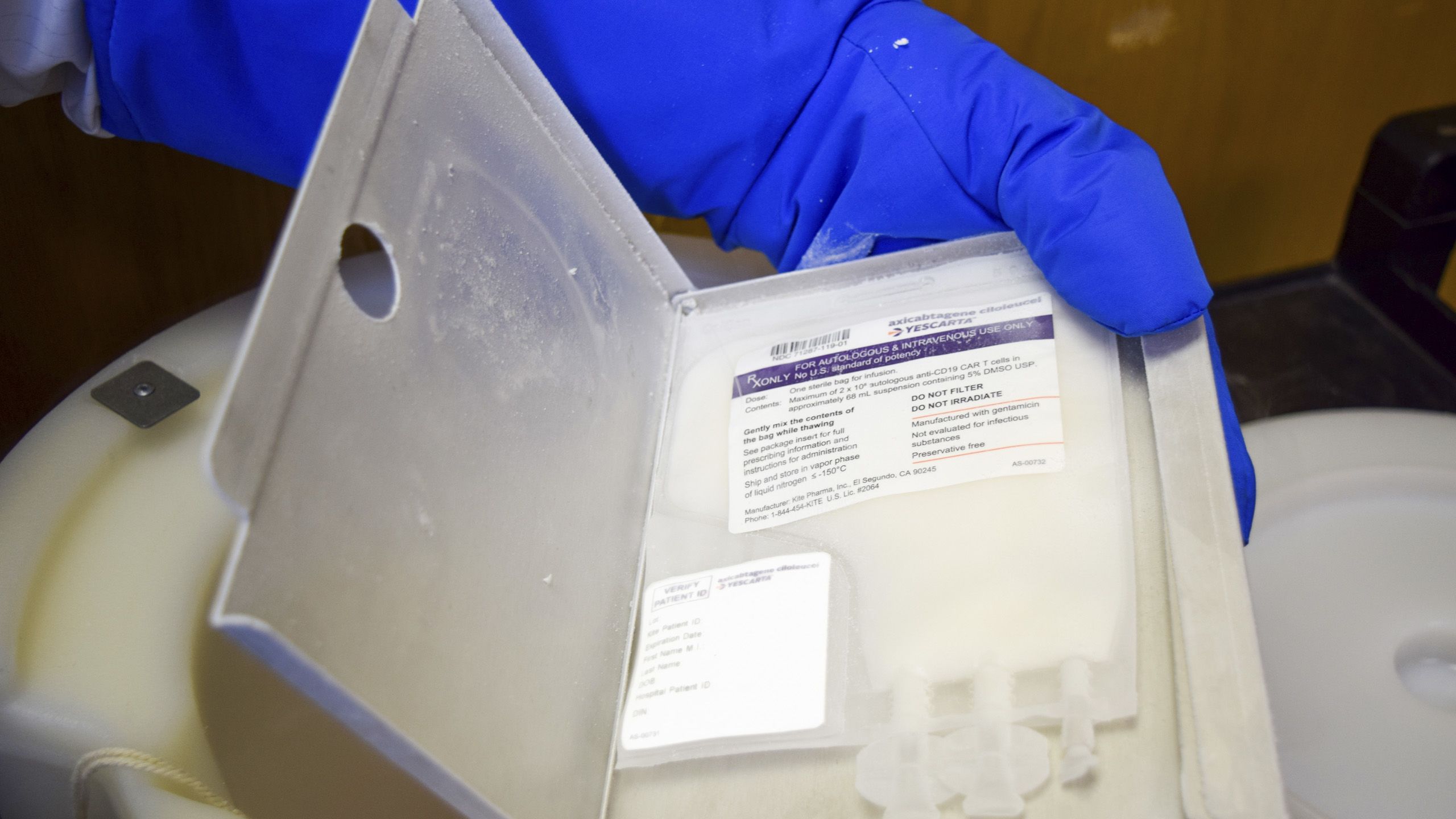
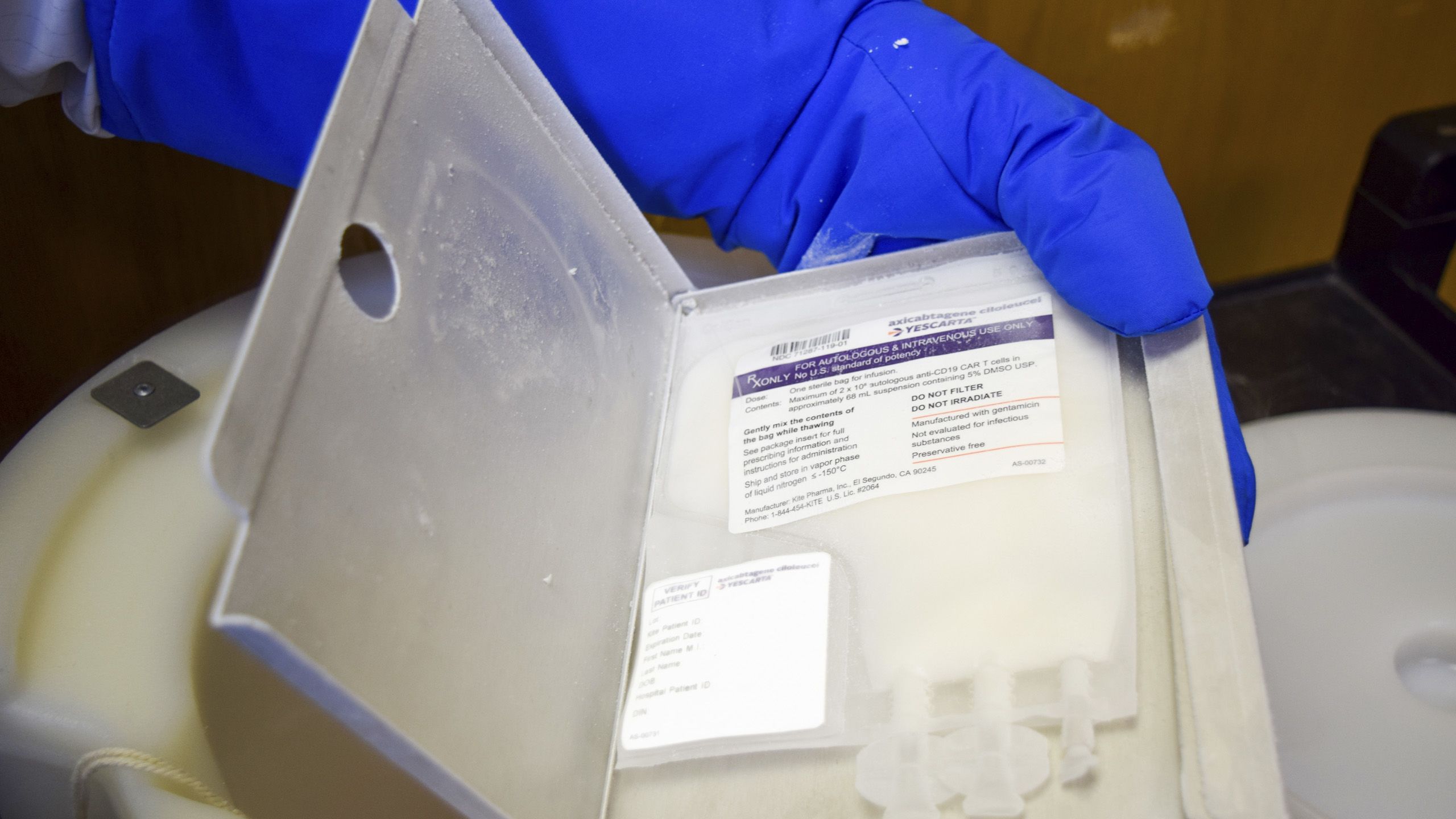
Three months later, in November 2018, she relapsed. Her doctors said her best chance of survival was a CAR T-cell clinical trial led by Winship hematologist Martha Arellano. Lundgren was referred to Arellano’s colleague, William G. Blum, head of Winship’s Leukemia Program. She and her parents moved near the Emory campus and in March, 2019, Blum’s team extracted Lundgren’s stem cells and sent them to Kite Pharma in California to be engineered into powerful CAR T-cells. They were infused in her blood on April 1. Lundgren felt good, but Blum was both encouraging and forthright about potential complications. On day five, they arrived. Big time.
Her immune system went into overdrive, creating a dangerous “cytokine storm.” Overproduction of immune cells and the immunoregulatory cytokine proteins that activate them caused her heart rate to shoot up, her blood pressure to plummet. Doctors had to restart her heart, like re-booting a computer. Then came the drooping face, inability to respond to questions, confusion. Going to wash her hands, she scrubbed her face instead, soaping the glasses she forgot to remove. She was calm but her parents panicked, even though they had been warned such complications were fairly common. Blum began the high wire act of giving enough steroids to treat the neurotoxicity, but not enough to kill her nascent T cells.
And it worked. Her re-engineered T cells began conquering the leukemia. In May, she and her parents went home. More than a year later, she is dancing again, director of the adult tap crew at Dance Lab Charleston. She finished her master’s degree in clinical nutrition. She is proud of having been part of a clinical trial. “CAR T-cell therapy saved me,” she says. “I wanted to help make it available to more people.”

SUPERCHARGING A PATIENT’S OWN T CELLS
T cells, the workhorses of the immune system, are designed to track down and destroy abnormal cells, including cancerous ones. But sometimes they don’t recognize the enemy or are too few or weak to mount a strong attack. Adoptive cellular therapies, like CAR T-cell therapy, transform those Clark Kent T cells into Superman CAR T cells, able (sometimes, not always, not yet) to get the job done.
STEP 1 Blood is collected from a patient and T cells are separated out and sent to a highly specialized laboratory.
STEP 2 The laboratory uses a disarmed virus to engineer the T cells to sprout chimeric antigen receptors (CAR) on their surface. Note that these receptors don’t exist in nature. The word “chimeric” comes from the Greek myth of a creature with a lion’s head, goat’s body, and serpent’s tail.
These engineered CAR T-cells are made up of the patient’s old biological T cells and new synthetic receptors. That means CAR T-cell therapy is personalized for each patient, with new receptors that recognize the antigens on the patient’s own cancer cells.
STEP 3 The re-engineered CAR T-cells are expanded into hundreds of millions, still only a small volume that barely fills half an IV bag.
STEP 4 Back in the clinical setting, the patient undergoes a chemotherapy process to eliminate some of the old T cells, then is infused with the new CAR T-cells.
STEP 5 If all goes as planned, the supercharged cells immediately begin to recognize and destroy cancer cells with the antigen that fits their new receptors. They also continue to multiply in the patient’s body, creating an ongoing, ever larger army.
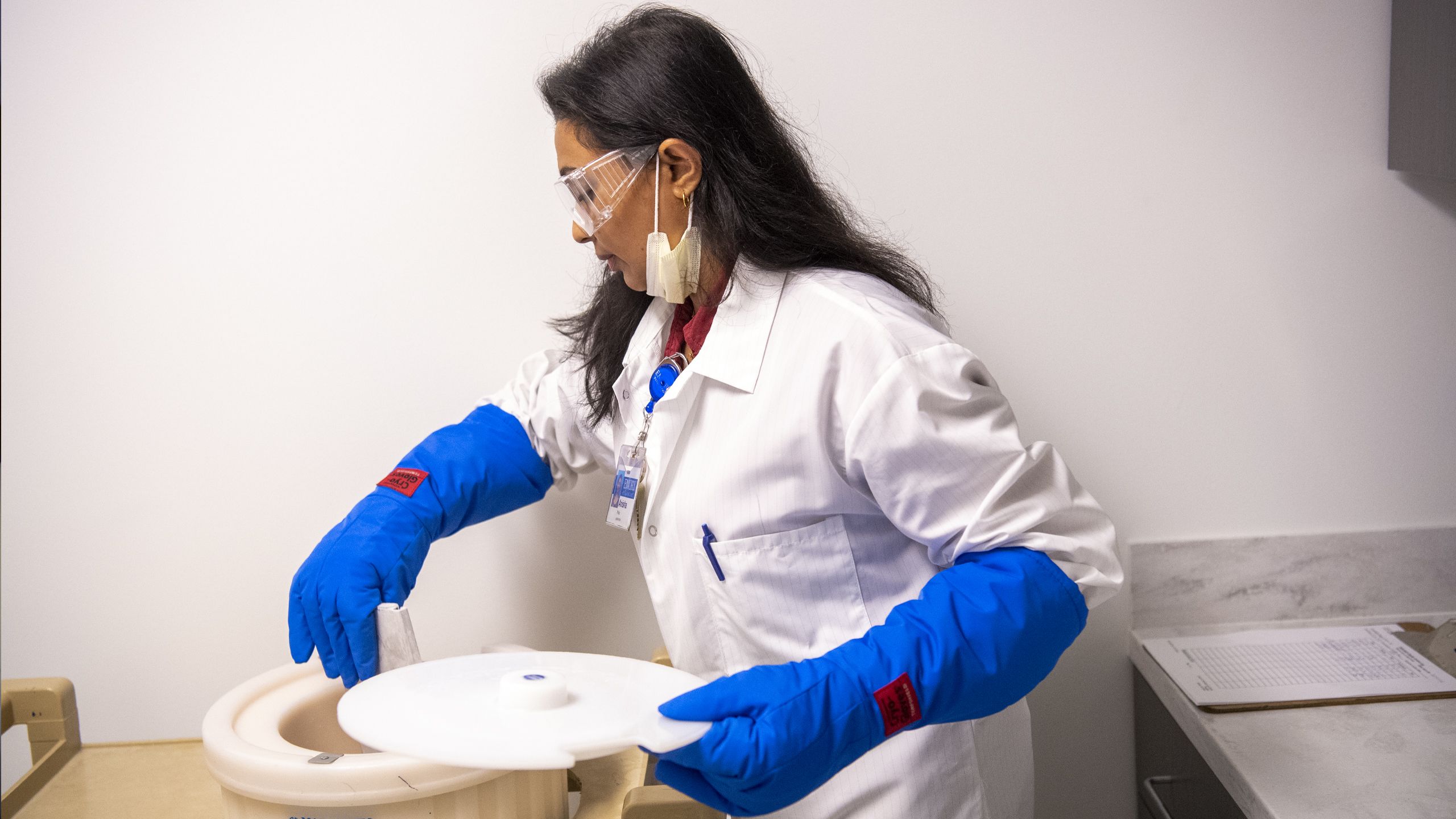
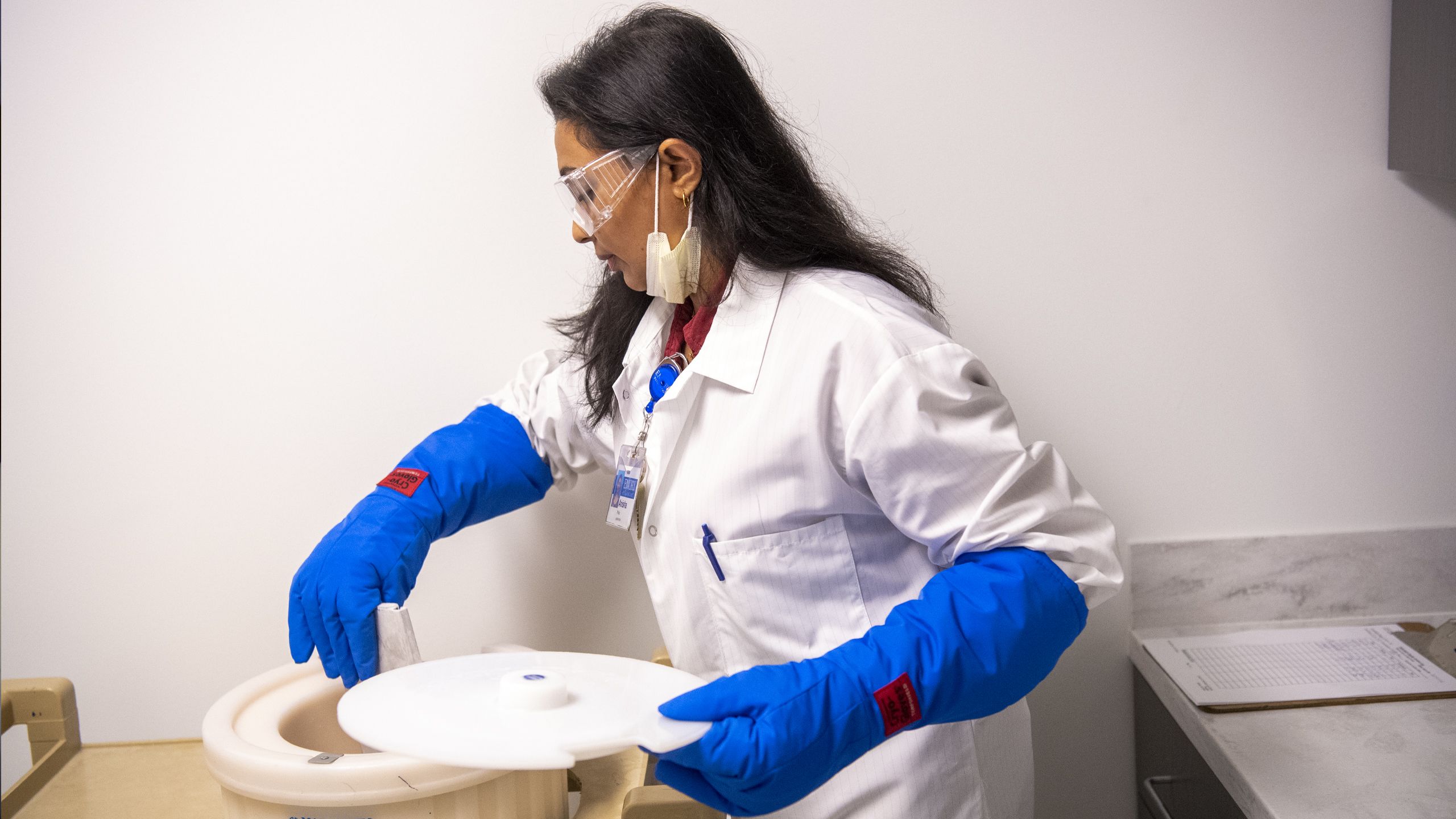
HOMEMADE CELLULAR THERAPY PRODUCTS COMING SOON. Lundgren’s T cells had to be packed and shipped across the country to one of the facilities capable of engineering CAR T-cells. That will soon change. A newly commissioned cellular therapy lab in the Emory University Hospital Tower, which is part of the Emory Cellular and Immunotherapy Core, will enable such cellular products to be produced on campus as early as 2021.
The new facility will be open to all scientists across Emory and partners like Georgia Tech, opening all types of research doors. For Winship, being able to produce the products at home will speed up the process, improve quality, lower costs, and provide flexibility in the design of clinical trials and other studies. In addition to CAR T-cells, the facility will be able to produce products including TIL, immune cells derived from lymphocytes that can be harnessed against tumors, and engineered T cell receptors (TCR), for therapy in which doctors target a specific tumor and add a new receptor to hit that target.
Medical technologist Andrew Auburn works in Lab C, one of the two ISO 7 clean rooms that will be used for clinical trials research and cell engineering. The environment, which must be kept sterile to prevent contamination of cells, is equipped with negative airflow and requires technicians to fully suit up. Lab C is equipped with an automated cell separation system for clinical-scale magnetic enrichment of target cells or depletion of unwanted cells; a Cellometer, for analysis of primary cells from peripheral blood, cord blood, bone marrow, and other complex samples; a CO2 incubator for cell cultures, and other equipment.









TACKLING THE TOUGH ONES

Every year, Winship clinicians see more than 2,000 patients with multiple myeloma, a blood cancer caused by malignant plasma cells (a type of white blood cell) that accumulate in the bone marrow. Multiple myeloma truly is a tough one. Although a number of drugs produce powerful effects, almost all patients eventually relapse, requiring repeat treatment. Winship’s goal is to end that cycle. New clinical trials are helping.

Tammy Strickland
Tammy Strickland
Tammy Strickland began the multiple myeloma treatment marathon in 2013, when the strong, once tireless contractor from north Georgia developed fatigue, muscle weakness, first-ever allergic reactions, and neck pain. Her diagnosis followed analysis of a tumor removed from her hip. Her sons insisted she see an expert.
As Interim Director of the Division of Hematology and Director of the Winship Cancer Institute Ambulatory Infusion Centers, Jonathan L. Kaufman coordinates the care for over 10,000 cancer patients served each year. Under his care, Strickland began a standard four-month course of drugs for multiple myeloma: lenalidomide, bortezomib and dexamethasone. It worked, then didn’t. An autologous stem cell transplant provided a longer-lasting remission — a happy 18 months — before relapse.
Working with Strickland’s local oncologist, Kaufman moved through the multiple myeloma menu — elotuzumab and lenalidomide, daratumumab and bortezomib, pomalidomide— each treatment providing a few months remission before another relapse.
In April 2018, she entered a clinical trial in which her T cells were removed, re-engineered into CAR T-cells, multiplied, and given back, 300 million strong. But after three months of feeling “vital, strong, balanced,” her symptoms returned, quickly escalating. A second treatment used 450 million cells. During that remission, Strickland built herself a new house. Then, relapse. CAR T-cell therapy was not turning out to be the one-shot lasting miracle it had been for Erika Lundgren. But, Strickland says, looking back, “just because a remission ends doesn’t mean you do. Dr. Kaufman always was looking for the next thing.”
He suggested a new clinical trial. Most combination therapies combine drugs. This one combined the immunotherapy drug pembrolizumab (Keytruda) with one session of radiation.
In November, 2018, Strickland painfully limped in to see Mohammad Khan, a Winship radiation oncologist specializing in radiation for lymphoma, multiple myeloma, and cancers of the skin. She received a single high dose of radiation to a tumor of myeloma (plasmacytoma) on her hip.
The tumor on her hip almost immediately began shrinking, taking the pain with it. She returned for her first Keytruda infusion and that week, she cooked Thanksgiving dinner for eleven.
Her remission lasted for almost two years. A relapse this summer brought her back in for the next new therapy being tested at Winship: a clinical trial using an immunotherapy drug with chemotherapy.
Strickland admits she used to distrust medicine. Before cancer, she wouldn’t even take a Tylenol. Today, she “thanks God every day for medicines and for the people smart enough to figure them out.” Especially clinical trials. “These trials — and Dr. Kaufman and Winship — gave me back my life.”
Sagar Lonial, Winship chief medical officer and internationally recognized expert in multiple myeloma, has been involved in the clinical trials of every immunotherapy drug ever approved for multiple myeloma. He believes new resources at Winship are going to further improve outcomes, particularly a $7.8 million gift from the Paula and Rodger Riney Foundation to fund fast-tracked multiple myeloma research projects. The gift, just announced this summer, will support fundamental research, translational research in the development of new treatments, and clinical research in understanding response rates and drug resistance.

QUICKER PATHS FROM BENCH TO BEDSIDE.
Winship was one of six cancer centers nationwide to receive NCI funding for a program designed to help quickly move new cellular therapies from the laboratory into clinical trials. The grant supports teams of Winship translational cancer immunologists and Georgia Tech biomedical engineers, helping research findings create new therapies or enhance emerging ones. Initial studies are focused on improving therapies for multiple myeloma. Dhodapkar is project leader; co-investigators are Max Cooper, in the Emory Department of Pathology & Laboratory Medicine and the Emory Vaccine Center, and Krishnendu Roy, director, Center for ImmunoEngineering at Georgia Tech.
Giving cellular therapies a boost through teamwork.
AAnother grant, a multi-million Specialized Center for Research (SCOR), made directly to the multiple myeloma team at Winship from The Leukemia & Lymphoma Society, is bringing together established investigators to develop a focused research program to improve adoptive cell therapies like CAR T-cell therapy. Headed by Dhodapkar, the grant illustrates the ever-stronger interdisciplinary, inter-institutional team science taking place at Winship. The new collaboration joins immunotherapy researchers from the Fred Hutchinson Cancer Research Center in Seattle and from Yale with Winship researchers Dhodapkar, Lonial, Lawrence Boise, vice chair of basic research in hematology and medical oncology, and Kavita Dhodapkar.
At the end of the day, all of us share the same goal, says Madhav Dhodapkar:
“We want our patients — all of them — to live the longest lives possible, as healthily and independently as possible. Immunotherapy — at first by itself, then in combinations — is a powerful weapon and Winship is committed to improving its ability, scope, ease and speed.”
Photography by Jack Kearse and Emory Photo Video. Editorial by Catherine Williams. Illustration by Carl Wiens. Infographic by Michael Konomos. Design by Stanis Kodman.