French artist Claude Monet loved capturing the bright, airy beauty of Paris and the Normandy Coast, setting up his easel outdoors and often depicting the same scene again and again as the light shifted and seasons changed. As he aged, however, his paintings began to show a darker color spectrum.
He despaired, writing to a friend, “I was no longer capable of doing anything good…Now I’m almost blind and I’m having to abandon work altogether.”
Monet was referring to a widespread malady that affects people of a certain age—the dimming and distortion of vision due to a cataract in one or both eyes.
I, like millions of others, recently encountered this in my own life. For many of us these days, this is a curable condition—although it has not always been so.
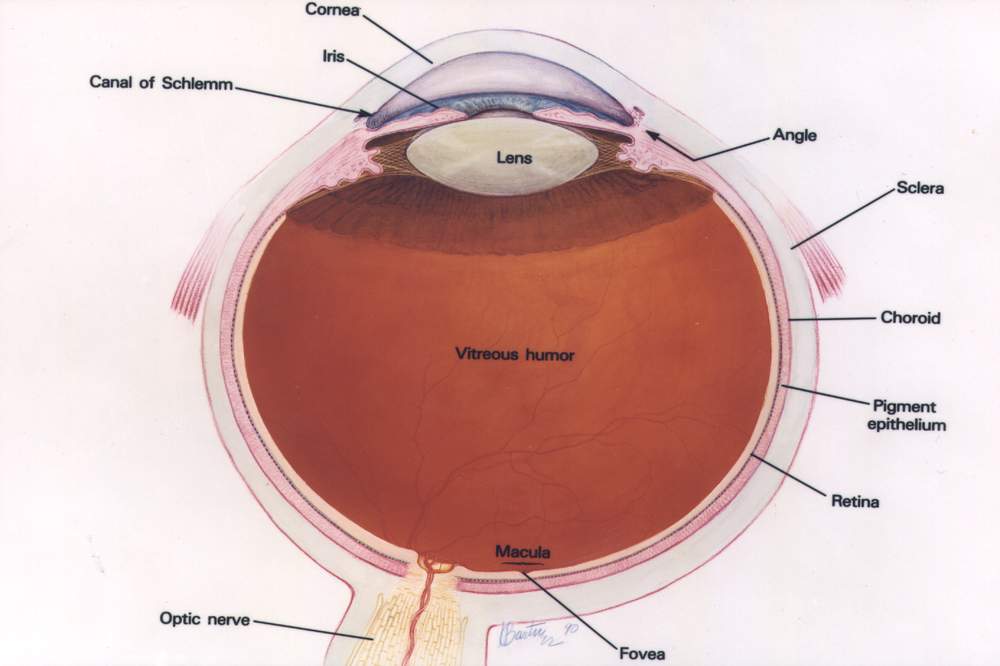
A cataract is a clouding of the normally clear lens of the eye. This diminishes and scatters the light that would ordinarily pass cleanly through the lens to the retina, generating nerve impulses the brain interprets as vision. The result is a darkened and blurred view of the world that can turn into blindness if the cataract becomes completely opaque.
Cataracts are most commonly associated with aging, affecting some 17% of people older than 40 and more than half of us by age 80. Cataracts, according to the World Health Organization, are the leading cause of blindness, which is on the increase as people live longer.
Known to medicine long before Monet’s time, the disease’s name has ancient origins: “Cataract” comes from Greek and Latin roots meaning “waterfall” or “portcullis,” a vertical grating that closes off an opening when lowered. This most likely alludes to the unclear appearance of the world seen through the cloudy eye, as if one is looking through a curtain of falling water or a screen, but it may also stem from an early belief that cataracts came from fluid traveling down inside the eye.
Modern medicine has shown that the cloudiness actually comes from clusters of proteins within the lens. The biochemical processes that cause cataracts, however, remain a mystery.
We do know that conditions like diabetes make cataracts more likely, as does long-term exposure to ultraviolet light (another reason to stay out of the sun—or to wear a good pair of sunglasses!) Researchers are studying these issues, but do not yet know how to reverse the progress of a cataract. Surgical removal remains the only option, as it has been for centuries.
Cataract surgery is one of the oldest known surgical procedures, first documented in a Sanskrit medical compendium at least 2,500 years ago, and in the Western world in a Roman work from 29 C.E. Early procedures were brutally direct. In a method called couching, still used in some countries, a sharp tool was inserted into the eye to cut the opaque lens free from its supports. The lens would fall to the bottom of the eye, which allowed light to reach the retina. The technique became more refined in 1747, when a French surgeon first removed an entire opaque lens from an eye. This required a relatively large incision, made without benefit of anesthesia. The aftermath was difficult for the patient as well, who had to lie immobilized for days while the wound healed.
Unsurprisingly, these methods often led to complications. And, although light could now reach the retina, it was unfocused, resulting in extreme far-sightedness. To restore a degree of overall good vision, subjects had to wear enormously thick eyeglasses. The breakthrough needed to make cataract surgery fully successful was to find a way to replace the natural lens.
The answer came from an unexpected source—observations made during WWII by Harold Ridley, an English ophthalmologist. Ridley wrote, “Extraction alone is but half the cure for cataract,” and he sought to make a synthetic replacement lens. But what material to use? It had to be biocompatible so it could reside in the eye for the long term while possessing the correct optical qualities to focus light as needed.
Glass was a possibility. Experience had shown that small pieces of it could remain inert in the eye for years. But Ridley found a better choice when he examined pilots such as Gordon Cleaver, an English air ace whose “Hurricane” fighter plane had been shot down during the Battle of Britain in 1940. Cleaver bailed out and survived, but his eyes were severely injured by embedded fragments from his shattered cockpit canopy made of the plastic Perspex, or Plexiglas, technically, polymethylmethacrylate (PMMA). After tracking Cleaver’s condition, Ridley concluded that PMMA was biocompatible with the eye and could be formed into a suitable lens at half the weight of glass. He enlisted the plastics industry to make such a lens and in 1949 used his surgical skills to install the first synthetic lens in a patient.
Ridley had invented the intraocular lens, but other ophthalmologists objected to the idea of deliberately putting a foreign object into the eye. Despite intense opposition, Ridley’s lens became widely accepted and saved tens of millions of people from blindness.
It is now standard outpatient procedure to extract the clouded lens and insert a synthetic lens. The type of lens can be chosen for monofocal or bifocal vision and to correct astigmatism. Other advances have reduced the size of the incision for faster healing and fewer complications. Rather than remove the organic, clouded lens in one piece through a large incision, an ultrasound technique breaks it into pieces that are suctioned out through a small opening. Then the surgeon inserts a folded plastic lens that fits through the small opening and unfolds into its proper shape. Accurate measurements of the eye to determine the new lens parameters and the use of a laser for precise incisions have also contributed to the procedure’s high success rate.
My Emory optometrist, Kenneth Rosengren, told me for several years that my eyes showed beginning cataracts and to watch for signs of their growth. This gradually appeared—not significantly in daylight, but my night vision became dimmer and I saw distractingly bright auras around streetlamps and car headlights that made it hard to drive in the dark, especially on unfamiliar roads. It was clearly time to get my cataracts fixed.
My Emory surgeon, Maria Aaron, was highly experienced, having performed some 8,000 cataract surgeries over two decades. I chose a monofocal lens to correct my life-long extreme near-sightedness, though not my middle-aged far-sightedness—I would still have to use reading glasses. I underwent an extensive eye evaluation, was issued eye drops to prepare for the surgery at home, and went in for the operation on my right eye. Then, a month later, my left eye.
Each surgery took about two hours. There was no pain during surgery under local anesthetic or afterward, except for temporary discomfort from eye dryness. An initial sensitivity to light and some cloudiness in my vision soon faded, and I felt fully recovered within a week for each eye. My vision became noticeably brighter even during the day and my visual acuity tested as excellent, 20/15 and 20/20 in the right and left eye, respectively. My final test has been driving at night, which now feels completely safe.
Operations improved my eyesight while saving me from the worst that cataracts can do. But I learned that, even before reaching that level, cataracts can alter vision in subtle ways.
The human eye and brain can distinguish among some 10 million different colors. Cataracts can severely hamper this remarkable discrimination, as they did for Monet.
After my right eye had been operated on, but while the left still had a cataract, I noticed that my eyes registered colors differently. What looked like a white wall or sheet of paper to my clear eye looked yellow or tan to the other.
Many removed lenses show a yellow or brown tinge, which occurs in nuclear cataracts that arise in the center of the eye. This tinting reduces the amount of blue light reaching the retina, changing the color spectrum a person senses.
For artists, photographers, and others who need fine visual perception, this distortion of color, along with the other changes, can be devastating.
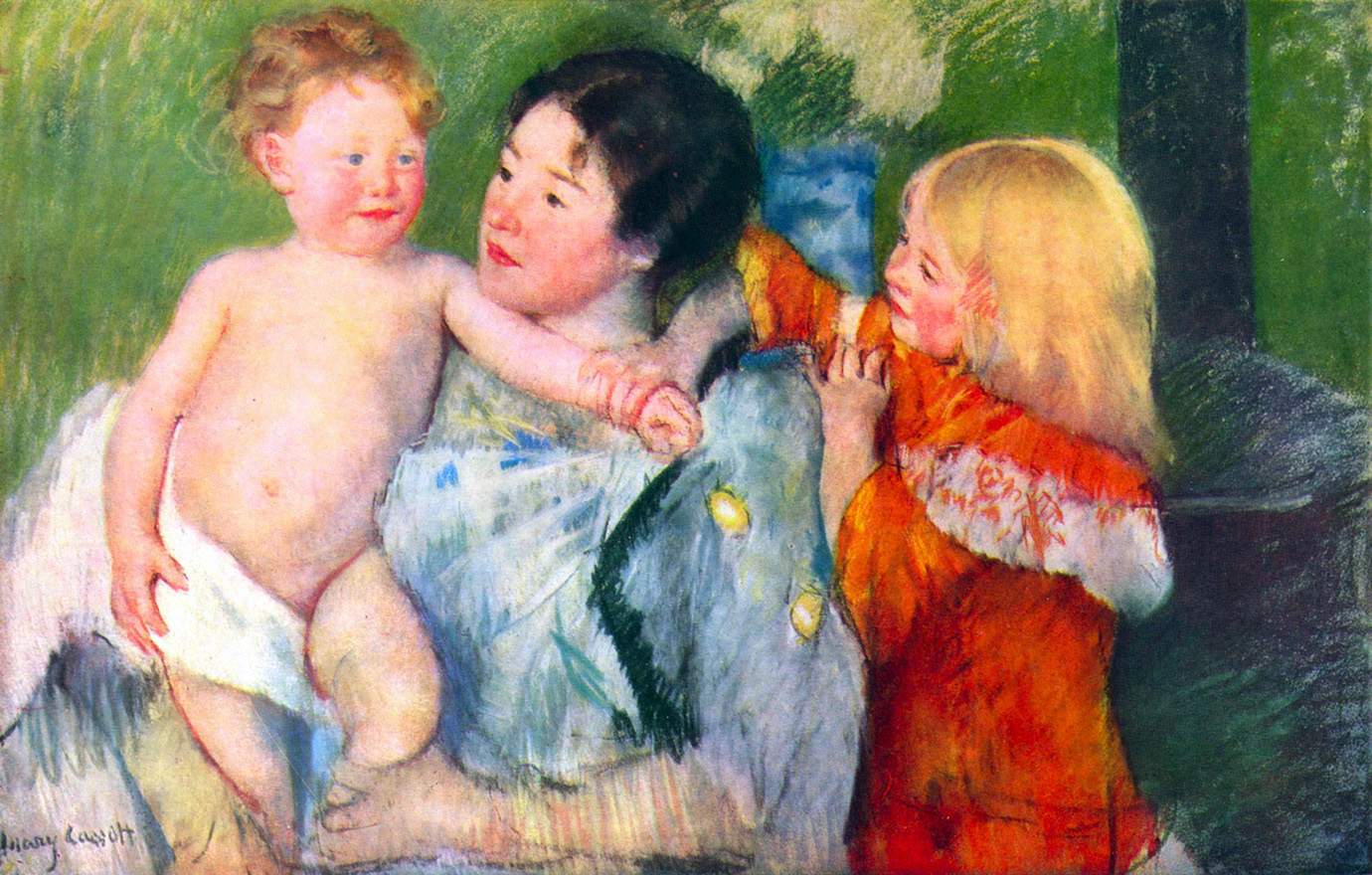
The stories of Monet, a founder of Impressionism in 1874 and its best-loved practitioner, and his contemporary, the American artist Mary Cassatt, known for her sensitive paintings of mothers and children, vividly illustrate how the treatment of cataracts has changed in the past century.
Cassatt had to give up painting after cataracts seriously affected her vision. Surgical efforts failed, and she died blind in 1926. Her case was complicated by diabetes, which was treated with radium—a radioactive element considered, at the time, a wonder cure, which was used to treat cataracts as well. We now know that exposure to radium can cause cataracts as well as other serious side effects, including cancer and death.
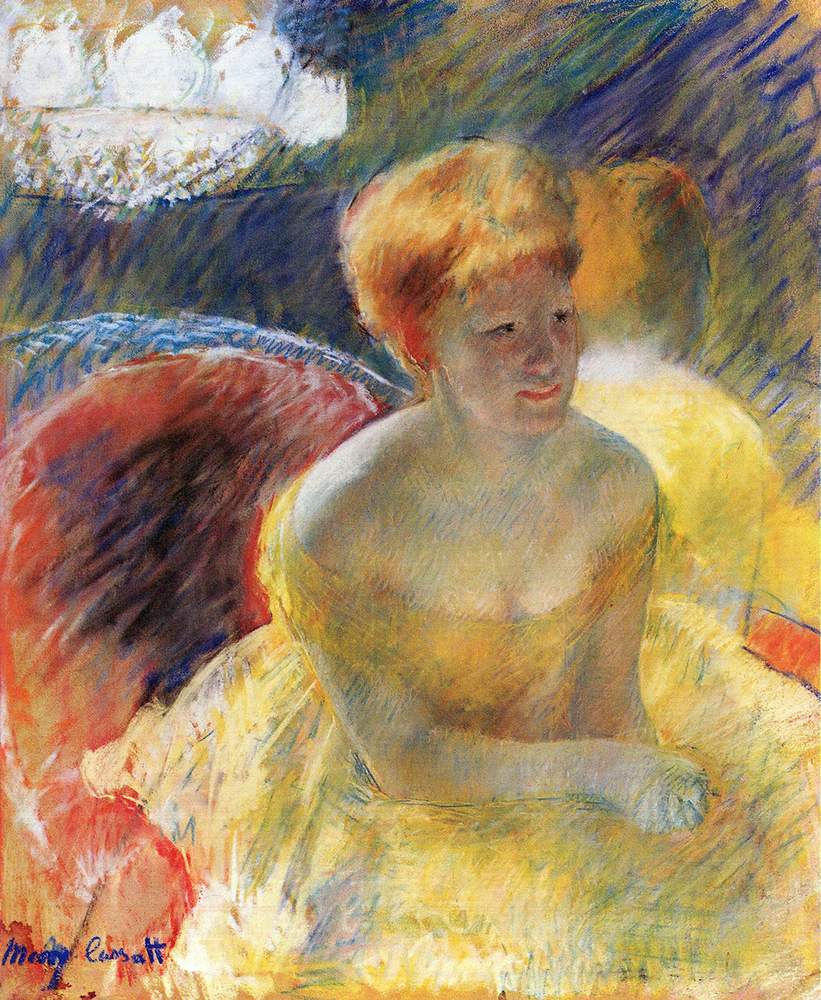
Claude Monet had years of difficulty with his color sense and his general vision due to cataracts, starting in his 60s. Though surgery was recommended, he resisted the idea, partly because Mary Cassatt’s surgery had not gone well.
By 1915, at age 75, he found that colors “no longer had the same intensity” and red shades looked muddy. He had to label his tubes of pigment and place paints in a particular order on his palette to make sure he could select what he wanted. He became sensitive to glare and wore a broad-brimmed hat to paint outdoors.
Finally, at 82, Monet agreed to have his right eye operated on. This did not go smoothly. He could barely tolerate lying immobilized between sandbags with bandaged eyes and told his surgeon it was “criminal to have put me in this position.”
But with new eyeglasses, he recovered his artistic vision sufficiently to finish eight mural versions of his famous Water Lilies paintings before he died in 1926.
While I don’t share Monet’s talent, I do have an equal appreciation for regaining my own full palette of colors with which to perceive the beauty of our world.
________________________________
Sidney Perkowitz, Charles Howard Candler Professor of Physics Emeritus at Emory, had cataract surgery at Emory Eye Center. He has written several books about scientific and biomedical topics and popular culture.
_________________________________________
ASK THE EYE DOCTORS: CATARACTS

Kenneth Rosengren, optometrist, Emory Eye Center
Q: Apart from regular eye checkups, what is the most important warning sign of cataract formation?
A: Increased glare at night when driving. A secondary symptom would be a blurring during daytime driving or reading that does not go away.
Q: If someone sees these signs, is immediate surgery necessary?
A: One of the nicer aspects of cataracts is that, even if they have become relatively severe, that does not usually affect the outcome of the surgery. Typically, there is no rush. As long as the patient can do most of what they need to, the surgery can wait.
Kenneth Rosengren, assistant professor of ophthalmology at Emory School of Medicine, specializes in primary eye care, glaucoma, and vision rehabilitation, using the latest technology to help low vision patients maximize their remaining vision. His research includes clinical trials of the implantable miniature telescope, contact lens solutions, and lenses.

Maria Aaron, cataract surgeon, Emory Eye Center
Q: Since you became a surgeon, what advance has contributed most to the success rate of cataract surgery?
A: Advances in phacoemulsification (more efficient use of ultrasound energy) have significantly reduced complication rates, improved efficiency, and shortened recovery time.
Q: Is there a new development in the wings?
A: Improvement in intraocular lenses (IOLs). The FDA has just approved the new “Symfony” IOL, which has an extended depth of focus and provides good distance vision and also some intermediate and near vision. Early results seem quite promising.
Q: Do you have a surgical ideal you would like to see become a reality?
A: It would be wonderful if we could completely eliminate the need for glasses after cataract surgery. This would likely be achieved with a flexible IOL that could focus at any distance, like a young, normal, and natural lens. It would likely need to be adjusted after surgery with a laser or other “office-based” technique. This will probably not occur in my lifetime but it’s fun to dream.
Maria Aaron,professor of ophthalmology at Emory School of Medicine and associate dean for Graduate Medical Education, specializes clinically in adult comprehensive ophthalmology, diabetic retinopathy, and cataract surgery. She has published extensively on resident education and lectured at national ophthalmic meetings on competency and accreditation. A recent focus is generational differences in academic medicine.