|  | |
 |
| IPE/CP as only the WHSC can accomplish | By now, I know that all of you have memorized the WHSC Priority Themes in the FY18-FY22 Strategic Plan. OK--maybe you don't have all of them saved to memory quite yet. One theme of great importance is Interprofessional Education and Collaborative Practice (IPE/CP). Teams and collaboration are what we do best in the Woodruff Health Sciences Center, and this theme will be of great significance as we advance our teaching, research, and clinical service missions.
As with all of our themes in the strategic plan, we are moving forward with dedicated teams and resources to achieve our goals. The IPE/CP Council has broad representation by physicians, nurses, and other health professionals from across the WHSC schools and Emory Healthcare. Our Woodruff Health Educators Academy (WHEA) is a great example of interprofessional education efforts. The inaugural WHEA Fellowship class includes representatives from the schools of Medicine, Nursing, and Public Health, along with representation from Emory Healthcare. The first annual WHEA Symposium was held last month and was a major success, attracting national attention. We are currently reviewing space options to support the success of IPE/CP at Emory.
There are many reasons to pursue an outstanding IPE/CP program. The educational experiences for our learners will be enriched, and our joy-in-practice goals will be strengthened. Perhaps most important, our interprofessional models of care for our patients and their families will be strengthened.
I appreciate all of those who are leading and supporting our IPE/CP efforts. The pace is rigorous and the goals are high. We would not have it any other way in the Woodruff Health Sciences Center.
Please direct questions and comments to evphafeedback@emory.edu.
Jonathan S. Lewin, MD, FACR
Executive Vice President for Health Affairs, Emory University
Executive Director, Woodruff Health Sciences Center
CEO, President, and Chairman of the Board, Emory Healthcare | |
| |
| 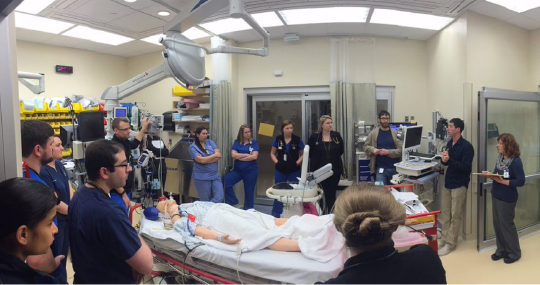 | | Interdisciplinary simulation in the cardiac ICU at EUH Midtown | Growing team practice | In one of Aesop's Fables, different parts of the body go on strike to protest doing all the work while the stomach gets all the food. The hands refuse to take up food, and the mouth and teeth are left with nothing to do. The arms and legs grow weak, and the body dies.
Doug Ander, assistant dean for medical education, used the age-old story to make a point in his lecture to first-year health professions students on Interprofessional Team Training Day on September 17.
"The moral of the story is why you are here today," he told them. "You are training in different disciplines, clinics, and parts of the world. What it comes down to, whether you are taking care of a patient or a community, is working together and having respect for each other in your different roles. Otherwise, your patient or community may die."
This year's team training day came on the heels of the first-ever symposium hosted by the Woodruff Health Educators Academy (WHEA). Held September 12, the symposium drew 135 participants eager to learn how Emory can support and expand interprofessional education and collaborative practice.
The team training day was among the initiatives highlighted. As symposium panelist Beth Davis noted, team training has expanded since it began in 2007. Originally an exercise for medical and nursing students, it now also includes students in public health and in the physician assistant, physical therapist, anesthesia assistant, and genetic counseling programs.
This fall, public health students participated for the first time, raising total attendance from 500 to 1,200 students. The presence of public health students at team training day illustrates the growing importance of interprofessional education, both at Emory and nationwide.
"Interprofessional education is now part of the accreditation criteria for schools of public health, as it is for other schools in the health field," said Davis, assistant professor of rehabilitation medicine and a team training day planning committee member.
The curriculum for team training day is based on TeamSTEPPS, a training protocol that helps schools and programs meet standards set by the Interprofessional Education Collaborative (IPEC).
Deborah Trautman, president and CEO of the American Association of Colleges of Nursing (AACN), explained IPEC's purpose in her keynote address at the WHEA symposium. AACN is a member of IPEC, and Trautman serves as IPEC's secretary and treasurer.
"IPEC helps us looks at the similarities and differences in our health professions so that we can align our core competencies and speak with one voice," Trautman said. "Despite our best intentions, we still practice very much in silos. We are all facing important struggles in population health, an aging population, and a shortage of providers. We need to think how to maximize our skills."
"The future is not about what we know but how we think creatively and how we interact with others."
Teamwork is definitely paramount for Vanessa Moll, another WHEA symposium panelist, who runs workplace simulations in the cardiothoracic ICU at Emory University Hospital Midtown.
Using Hal, the medical school's simulation mannequin, she puts a team of nurses, respiratory therapists, residents, pharmacists, and others through their paces. As they practice, each patient scenario becomes more elaborate. During one exercise, she said, Hal went into hemorrhagic shock. The team didn't identify the bleeding in time, and their patient died. Team members were crushed.
"We talked over the scenario, and I gave the team a chance to do better," said Moll, assistant professor of anesthesiology. "That's important. The scenario became so real that the team took a hit when things didn't go well."
In her presentation, Moll showed a photo of the Hamburg Symphony Orchestra in its new concert hall in her native Germany. "That's what I want my team to look like," she said. "Everybody is an expert, but only when you combine skills do you have a symphony. That's what we are striving for."--Pam Auchmutey | |
| |
|  | A new, improved home for EeMR | Earlier this month, Emory Healthcare transferred the Emory electronic medical record (EeMR) from its home here at Emory to Cerner Corporation's remote hosting facilities in Kansas City, Missouri. The process came off smoothly, thanks to a level of planning and team coordination resembling something akin to a rocket launch.
The "flip" from one location to the other, which occurred on October 19, took about 18 hours and involved hundreds of people, both at Emory and Cerner, says Sheila Sanders, EHC chief information officer, who describes the elaborate and painstaking process culminating in the event.
It began a year ago, she says, with Cerner's construction of a comparable infrastructure to house the Emory data. EHC Information Systems then copied the EeMR database and installed two network circuits to allow any changes being made to the local EeMR to be transmitted simultaneously to the remote site. Over the summer, the Information Technology team and end users tested every aspect of the new system, including, she says, "more than 20 years of customization that had to be rebuilt, along with hundreds of interfaces to third-party vendor systems used by various departments."
After multiple rounds of testing and remediation, preparations began for the period when EeMR would be down, as the final transfer of data took place. "Nursing and clinical informatics staff worked with operational leaders from each site to make sure those working during downtime knew how to use paper processes while caring for our patients," says Sanders. "We established a detailed flip plan and practiced it multiple times leading up to the event. We also set up command centers at each hospital and held twice-daily debriefs on the day of the flip to report critical issues as well as status of operational recovery."
With the event behind her, Sanders can now concentrate on measuring the benefits of remote hosting. "The average transaction response time for clinicians using EeMR is now 0.37 seconds as opposed to 0.44 prior to the flip," she says.
But even more important than reducing response times is reducing unplanned down time, says Sanders. "There is a reason why EMR infrastructure is trending across the industry toward remote hosting. Cerner has a larger, more robust backup and disaster-capable infrastructure than we could possibly maintain ourselves." | |
| |
|  | | Last May, the team at Emory's Serious Communicable Diseases Unit and the Grady Hospital EMS Biosafety Transport team took part in a nationwide exercise testing the capacity of specialty units across the country to intake patients infected with special pathogens. | Sharing lessons learned after Ebola | The Serious Communicable Diseases Unit (SCDU) in Emory University Hospital, where four patients with Ebola virus disease (EVD) were treated in 2014, continues to be of keen interest to infectious disease and public health experts, scientists, military and government officials, and students from here and around the globe.
About 60 groups have toured Emory's SCDU in the past two years, says Allison Klajbor, clinical research coordinator in infectious disease. "We've had ministers of health, members of the US Air Force, and nursing and biostatistics classes," she says. Visitors include delegations from Tokyo, Nigeria, Hungary, Thailand, Japan, England, Vietnam, China, and Canada.
In September, for instance, senior nurse Allison Sykes, of the Newcastle upon Tyne Hospitals NHS Foundation Trust, visited Emory's SCDU as part of a tour of biocontainment units across the US and Europe. "I was the infection prevention and control lead for the development of the high-level isolation unit at our trust during the 2014 Ebola outbreak," Sykes says. "I'm also visiting units at Bellevue, Johns Hopkins, Nebraska, Iowa City, Madrid, Rome, Hamburg, and Berlin." On completion, she said, her report and recommendations will be submitted to the Winston Churchill Memorial Trust, who funded the trip, and shared with other treatment centers in the UK and the national High Consequence Infectious Diseases programme.
Sykes did a walk-through of the SCDU's negative-pressure rooms, lab, and autoclave with SCDU senior administrator Sonia Bell, critical care nurse Jill Morgan, and SCDU medical director Bruce Ribner.
The SCDU has expanded since 2014, and changes have been incorporated in response to lessons learned since that time. For example, as the team told Sykes, as many surfaces as possible in a unit like this should be stainless steel, regular hospital floor tile will be eaten away by continual disinfection, and while patient rooms need to let in natural light, they should also be shielded from view.
"One of the things we didn't anticipate was the public interest," says Ribner. "There were literally helicopters flying overhead to take photos." Blinds couldn't be cleaned properly, so the team settled on opaque film on the outside of the window with enough of an opening at the top for the patients to see "a little sky, while protecting their privacy."
Sykes also was interested in how the unit dealt with patient transport, waste, personal protective equipment, and what medical procedures (such as mechanical ventilation and dialysis) could be performed in the SCDU's rooms.
In June, physician Ian Crozier accompanied a group from the American Society for Microbiology "Microbe 2018" conference as they toured the very unit where he spent 40 days recovering from EVD.
The sickest of the four patients treated at Emory, Crozier remembers only part of his time in the unit--but his successful treatment revolutionized patient care.
"Even after I awoke many weeks later, a few days after my 45th birthday, I wasn't fully aware of how closely I had looked death in the eye," he said. "As a physician, if you had told me during my first week of care that I would develop encephalopathy, respiratory failure, kidney failure, and cardiac arrhythmia, I would have expected my chances of survival to be almost zero. What happened inside those four walls changed the nature of how we treat Ebola patients."
The visitors lined up to take selfies with Crozier, shake his hand, and ask a volley of questions as Morgan, one of Crozier's nurses in the unit, demonstrated the protective PPE outfit, complete with powered air-purifying respirator, double gloves, and booties. "You have to dissect the implications of every action taken in the unit," said Morgan.
Emory's efforts to prepare for future outbreaks have continued through research, improved patient care protocols, and training health care workers and first responders around the country.
"The government has called on Emory to care for patients with special pathogens in the US," says infectious disease physician Colleen Kraft, a member of the original Ebola team. "We would like to take what we learned about preventing transmission of diseases in a biocontainment unit out into every health care interaction."--Mary Loftus | |
| |
|  | | Sterk named to National Academy of Medicine | The National Academy of Medicine has elected Emory President Claire E. Sterk to its 2018 class of 75 leading health scientists and 10 international members. Members are elected to the NAM by their peers from among candidates nominated for their accomplishments and contributions to the advancement of the medical sciences, health care and public health. Emory currently has 31 members in the NAM. Read more.
| | |
| | |  | | New core facility launched | Emory recently launched the new cross-disciplinary Translational Neuroscience Core (TNC), codirected by Nicholas Boulis and Thais Buchman. The TNC provides the following:
- Specialized neurosurgical instrumentation
- Technical assistance and experimental design
- Surgical execution in large animal models
- Assistance with work ranging from pilot experiments to preclinical testing
| | |
|
| |
|  | | Fund-raising goals shattered | Gifts, pledges, and planned gifts to Emory totaled $657.9 million for FY 2018, exceeding the $245 million goal for the year by 169%. The WHSC portion of this total, $589.6 million, more than tripled the WHSC goal of $181 million. Even without the historic Robert W. Woodruff Foundation gift of $400 million (the largest gift in Emory's history), the WHSC still exceeded its goal by more than $8.6 million.
| | |
| | |  | | Nursing school and Emory Healthcare co-launch scholarship program | The nursing school and Emory Healthcare have launched InEmory, a 15-month accelerated BSN program for second-degree students beginning in January 2019. Students will receive up to $10,000 in scholarships and will be hired by Emory Healthcare following graduation and successful completion of licensure exams.
| | |
|
| |
| 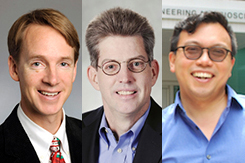 | | Funding for point-of-care diagnostics | A $7 million NIH grant will fund the Atlanta Center for Microsystems Engineered Point-of-Care (POC) Technologies (medical diagnostic tests performed outside the lab and close to where the patient is receiving care). The Atlanta Center will focus on cardiac, pulmonary, hematologic, and sleep applications. Principal investigators include Emory faculty Greg Martin (left) and Wilbur Lam (right) and Oliver Brand (center) from Georgia Tech.
| | |
| | |  | | 5K funds professorships | Larry Boise and Erwin Van Meir are inaugural recipients of two new endowed professorships funded through a portion of the proceeds from this year's Winship Win the Fight 5K Run/Walk. Boise develops novel approaches to multiple myeloma and other B cell malignancies. Van Meir is an expert in neuro-oncology research, including glioma and medulloblastoma and in eye melanoma and leads Winship's Cancer Cell Biology Research Program.
| | |
|
| |
| |  | | Brain imaging and analysis expert Vince Calhoun was named founding director of the Center for Translational Research in Neuroimaging and Data Science, which is supported by Georgia State University, Georgia Tech, and Emory. At Emory Calhoun will have appointments in neurology, psychiatry, and radiology.
C. Michael Cassidy joined Emory earlier this month as director of the new Emory Biomedical Catalyst, where he will lead efforts to enhance innovation, entrepreneurship, and development of intellectual property, as well as identify and develop areas of frontier research. For the past 18 years, Cassidy has been president and CEO of the Georgia Research Alliance.
Abigail Hankin-Wei received a Secretary of State Award for Outstanding Volunteerism Abroad from the Associates of the American Foreign Service Worldwide for her work volunteering as the only trained emergency medicine physician in Mozambique. The award also recognizes her role in working with a local medical school to start an emergency medicine training program in that country.
Dorian Lamis received a NARSAD Young Investigator grant from the Brain & Behavior Research Foundation to examine the roles of childhood abuse and gene modifications in suicidal behaviors among low-income African Americans with bipolar disorder.
David Stephens received the inaugural Lifetime Service and Leadership Award from the medical school at the recent conclusion of the school's Faculty Recognition Week. | |
| |
|  | Nov. 12: Veterans Day Ceremony. 10:45 a.m. Emory Quad.
| | |
| | | Feb. 28 - March 1, 2019: Georgia CTSA Science Conference, Callaway Resort and Gardens. Register.
March 27-28, 2019: Winship Scientific Symposium and Poster Session, HSRB 1st floor, Rollins Auditorium. Contact Judy Fortin.
| | |
|
| |
|

