The morning of Jan. 2, 2013, dawned unremarkably across Atlanta—cool and overcast, with a leaden sky that hinted of rain.
Weak winter light threaded through the treetops that tower over Clifton Road as Sylvia Ennis wound her way to work along a woodsy route just south of the Emory campus, past vintage brick homes, tidy lawns, and dense foliage that changed with the seasons.
Normally, Ennis wouldn’t have been heading back so soon after the holidays. But it was the start day for a new hire, and they had arranged to meet at the Neonatology Division of the Department of Pediatrics at Emory School of Medicine, where Ennis was a clinical business manager.
As her Toyota Corolla spun along Clifton Road, Ennis mentally primed herself for the work week. Wearing a new gray suit and earrings, a pretty blue blouse, and her favorite boots, she felt ready to meet the day. Despite the gloomy weather, her thoughts spooled happily among tasks that lay ahead and an upcoming trip, a long-awaited Caribbean cruise with friends in early February to celebrate her 50th birthday.
Altogether a routine morning—until, abruptly, it wasn’t.
Ennis never heard the tree coming down, only its deafening arrival atop her sedan, an instantaneous explosion of crushed steel, shattered glass, and sudden, enveloping darkness.
The loblolly pine was more than 100 feet tall, a towering reminder of a time when dense woodlands rose over much of North Georgia. Its stout trunk would have taken the arms of two people to encircle it.
Falling from the opposite side of the street, the tree landed diagonally upon her car, stretching from the left bumper across the front passenger’s seat, where it fully collapsed that side of the roof.
Through a haze, Ennis struggled to absorb a landscape suddenly turned bizarre and nonsensical. She saw the damage around her before she fully understood it, and felt her senses awaken in staggered waves. The trunk had landed only inches to her right, trapping her in the one part of the car that hadn’t been flattened. Peering through a fractured windshield Ennis could make out a wall of dark, mossy bark and a dense tangle of pine needles and branches, which enveloped her like a prickly cocoon.
Glancing down, what she saw didn’t make sense—a tree limb the size of a fence post protruded from her abdomen. A good six inches in diameter, the jagged branch had speared through the windshield and steering wheel before striking Ennis. Oddly, she didn’t see a drop of blood.
Shivering and in shock, she knew only that she was cold, conscious, breathing, alive. Her thoughts flashed to her son, Dayvon, and grandson, Nasir. Ennis knew she wasn’t going to live through the day. Closing her eyes, she prayed that they would be able to find peace without her.
Through pine needles and dark branches, a man’s face appeared at her window. Ennis didn’t understand. Am I already in heaven? Is this an angel?
“Are you okay? Can I call somebody?” the passerby shouted.

Tree on vehicle. Possible entrapment. 1183 Clifton Road.
Seven minutes later, Engine One arrived to find the road blocked by a toppled pine. Upended, the tree's exposed root system stretched skyward, taller than a person.
Complicating the rescue, the falling tree had snapped a power pole. Electrical lines snaked atop Ennis’s car; no one knew if they were hot. As some responders began crawling between branches toward the vehicle, others grabbed chainsaws.
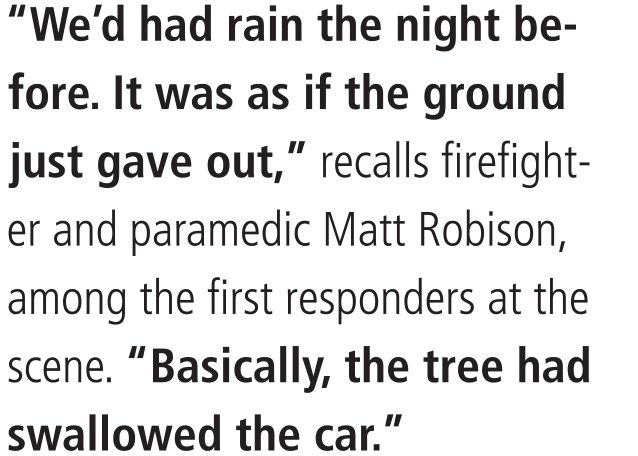
Captain Jeff Goins was already in the field that morning, wrapping up an earlier call a few blocks away when they heard the call and responded. Two employees from Georgia Power also in the area rushed to the scene to confirm that the downed line was dead—critical information that saved precious time, notes Goins, who began directing extrication.
Reaching Ennis, rescue workers found her stunned but conscious, quietly studying the five-foot branch that appeared jammed against her abdomen, effectively pinning her to the seat. It wasn’t until Station One HazMat team member Samuel Payton Owens slid behind the driver’s seat that he fully realized what they were seeing. The branch had passed right through Ennis—entering her lower left abdomen, exiting her right buttock, and coming to rest on the floor of the backseat.
Owens asked Ennis for her name, and how she was feeling. “A tree just fell on my car,” she quietly reported.
“This is going to sound crazy,” he told her, “but you have a tree limb all the way through your body, and we’re going to take care of you.”
For fire and rescue crews, impalements aren’t uncommon. “You’ll occasionally see a pencil, a knife, a fencepost—things usually resulting from people being ejected from a car, jumping from a building, or running from the police,” Goins says. “This was different.”
As a frenzy of brush-cutting growled to life outside the car, Owens sat in the backseat with his arms wrapped around Ennis, an embrace intended to comfort and stabilize her.
Before Ennis could be removed, two cuts had to be made: One outside, to separate the branch from the tree trunk, and another inside the car, between Ennis and the steering wheel, to shorten the branch and permit extrication. She would need to be moved with the branch still within her.
With the car doors removed, the team assessed Ennis’s vital signs, which, surprisingly, were fairly stable.
Grabbing a Sawzall reciprocating saw, HazMat team member Carey Patton stood on the hood of the car and began cutting the branch from the tree trunk. When the vibrations caused Ennis to moan softly, they immediately switched to a smoother-running chainsaw.
Work inside the vehicle was trickier. First, they wedged cribbing—large plastic blocks—between Ennis and the steering wheel. If the chainsaw slipped, or the branch gave way, it would offer support and protection. Using a sheet to shield Ennis from flying sawdust, rescue workers began cutting into the branch just inches from her face.
It was delicate work. The airbag, which had not deployed, could go off at any moment.
For first responders, the goal of most trauma calls is straightforward: plug holes, start fluids, and get your patient on a surgeon’s table, fast. Since the tree branch had to remain in place, EMT Jeanine Fannell worked around it to insert an IV line in Ennis’s arm and begin pushing fluids, a routine protocol that would pay off down the line.
Ennis was eased from the car, branch intact, and carefully placed on her side onto a transfer board. In the ambulance, blankets were wedged to secure her position.

By 9:18 a.m., she was on her way to Grady Hospital’s Marcus Trauma Center, among the busiest Level 1 trauma centers in the country.
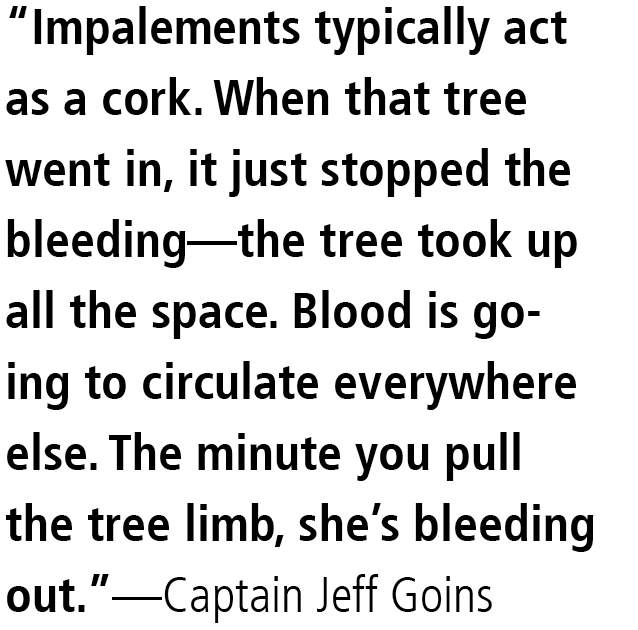
At Grady, trauma surgeon Omar Danner was completing morning rounds with nurse practitioner Lexi Frederick when he received a page: A 49-year-old woman impaled by a tree. Tachycardic heart rate. Falling blood pressure...
They both thought it had to be a trauma drill.
Reporting to the trauma bay, Danner found an ocean of blue and green scrubs—emergency medicine and surgical trauma team members, all awaiting Ennis.
When the EMTs rolled her in, Ennis lay on her side, the tree branch protruding almost as if she had been harpooned, thought Danner.
Her blood pressure was plummeting. When trauma nurses attempted to draw blood, there was nothing to extract—a sign of near-total circulatory collapse. Attaching a unit of blood to the existing field IV, they sped toward Trauma Room One, an operating room reserved for the most critically injured patients.
Without a detectable blood pressure, Ennis was clearly in extremis—deep shock—and likely about to die.
Danner, associate professor at Morehouse School of Medicine, recalls thinking that this was the moment when all of his years of medical school and residencies and emergency room experience would be put to the test.
Trauma surgeon Omar Danner and Chief of Urology Jeff Carney
News of the case traveled fast, from cardiovascular and orthopedic specialists to neurology, urology, anesthesiology, and emergency nursing staff.
Sheryl Gabram, Grady surgeon-in-chief and professor of surgery at Emory, and surgeon Ed Childs, chair and professor for trauma and critical care at Morehouse, were also notified of the unusual case, along with former Grady trauma medical director and fellow trauma surgeon Jeffrey Nichols.
“Needless to say, by the time we got there, she had an audience,” Danner says.
Level 1 trauma care is a team endeavor, each patient’s treatment a complicated choreography requiring many hands, from first responders to surgical specialists to critical care nurses.
Two beds were shoved together to accommodate both the patient and protruding branch, and Ennis was intubated and sedated. Ravi Rajani, assistant professor of vascular surgery at Emory and director of vascular and endovascular surgery at Grady, ordered an X-ray of the arteries of her pelvis and abdomen.
The arteriogram revealed vessels that were somehow intact, Danner says.
“We were relieved, to say the least,” he says. “There was hope.”
Her major blood vessels were spared. Had they been badly damaged, it would have changed everything. With improving hemodynamics due to the transfusion, focus turned to removing the branch and assessing internal injuries.
Ennis’s abdomen was prepped for surgery and a sterile plastic drape placed over the branch. As the team opened her with a midline incision from her xiphoid process to her pelvis, it became evident that the internal damage was extensive.
The tree limb had breached the abdominal wall and plunged through her pelvis, where it remained firmly lodged. The abdominal muscle and surrounding connective tissue across her lower left side “were basically obliterated,” Danner says.
Using surgical pads for traction, Danner directed chief resident Trey Walker to grasp the branch and pull on his count.
One. Two. Three…
Heaving and hoisting, twisting and turning, Walker pulled the branch forcefully from Ennis’s body, and Danner and Childs hurriedly packed the wound cavity with surgical pads to help control blood flow.
“Do we have blood pressure?” Walker asked.
With a nod from Emory anesthesiologist Gary Margolis, the dressings were removed and Danner began cataloging internal injuries.
Scooping up Ennis’s small intestine with his gloved hands, he found it torn into multiple pieces. He clamped the remaining ends together to control contamination, meticulously removing bark and debriding dead tissue; later, her small bowel would have to be resected.
Ennis’s colon was intact but badly bruised, turning black and blue before their eyes. Compressed by the branch, her bladder had burst—the entire top of it was missing—and would have to be repaired.
The ureter on the right side of her body, a tube about the diameter of a pencil, had been ripped from her bladder and severely crushed.
For Jeff Carney, Grady’s chief of urology and assistant professor at Emory, detached ureters are fairly routine, often the result of gunshot wounds or stabbings. But he had never encountered anything like this.
“At Grady, you never know what’s coming in the door. But this was a once-in-a-lifetime trauma,” says Carney, who would later learn the accident had occurred less than 200 yards from his own home on Clifton Road.
In all, Ennis had injuries to her ureter, colon and small intestine, stomach muscles and soft tissues, and right buttock. Though her pelvis was fractured, Emory orthopedist Chris Sadlack concluded that it could be managed without surgery.
Despite the deep, dirty wound (her medical team would spend weeks flushing out bits of wood and debris), there was good news. Beyond damage to her small intestine, Ennis was emerging with no major vascular injuries and no life-threatening organ damage.
Danner placed a temporary closure on Ennis’s abdomen, which would serve as something of a swinging door over the coming weeks, opening and closing for ongoing treatments. The exit wound in her right buttock would be sutured shut.
Finally, Ennis was taken to the ICU for a CT scan and what Danner describes as “aggressive resuscitation” throughout the night. With multiple surgeries anticipated, she would be kept in a medically induced coma for nearly three weeks battling sepsis, ventilator-associated pneumonia, and allergic reactions to several antibiotics.
During the month of January, Ennis returned to an operating room nearly a dozen times, where her wound was repeatedly washed out, her bladder repaired, and her small bowel assessed.
From the start, Danner knew that Ennis would need considerable reconstructive surgery on the jagged hole in her abdominal wall. But with so much damage, it was hard to predict how things would turn out.
Plastic and reconstructive surgeon Angela Cheng had seen her share of impalements during her time at Memorial Hermann Hospital in Houston—patients gored by bulls and stabbed with samurai swords, ranchers run through by fence posts.
Ennis’s impalement, an utterly random act of nature, hit home for Cheng, now an assistant professor of surgery at Emory, in a way previous cases hadn't.
“A lot of us work at Emory and drive on Clifton Road," Cheng says. “That could have been me.”

Plastic surgeon Angela Cheng
When Cheng was brought in for a consult the morning after Ennis arrived at Grady, the priority was clear: Stabilize her and address the most critical injuries.
Cheng’s treatment plan would arise from three initial questions: What’s missing? How do we replace or reconstruct it? When is the best—and safest—time to do that?
It was clear that Ennis’s abdominal muscle was completely blown out. Though her pelvic fracture would not require surgery, her crushed ureter would eventually need to be reconnected.
It could have been worse. Being impaled by a large, blunt branch, as opposed to a thin, sharp implement, had shoved critical organs aside rather than pierce through them.
Due to multiple resuscitations, Cheng knew that Ennis’s abdomen would be profoundly swollen and distended— the result of receiving massive amounts of blood and fluids, which is typical for trauma patients.
Two weeks after the accident, Cheng operated on Ennis, sewing about $50,000 of Strattice, a biological mesh derived from pigskin, in place across her open abdomen.
Complete closure of the gaping wound left by the branch would take time.
Three weeks after the accident, Ennis was taken off the ventilator. Waking from her coma, nurses began to talk with her, assessing possible memory loss or brain damage. At first, Ennis was deeply disoriented. Her right leg was ablaze with pain. She didn’t understand.
“I couldn’t do anything,” she recalls. “I couldn’t walk, I couldn’t move, I had to learn everything all over again.”
As her family helped piece things together, Ennis learned that she’d lost a great deal of blood and had very likely cheated death.
As her abdominal swelling receded, Ennis's skin gradually loosened. But Cheng knew that despite a small skin graft, there wasn’t going to be enough abdominal skin to cover the wound. So she decided to insert tissue expanders—essentially, balloons filled with salt water—beneath her skin. “Luckily, our abdominal skin is designed for lots of stretching,” Cheng says.
The balloons also help encourage regrowth of skin cells. After the skin on Ennis's stomach had expanded an additional 25 to 30 centimeters, Cheng performed another operation to remove the expanders and close the wound. Ongoing physical therapy focused on strengthening Ennis’s abdominal wall.
“For the patient, it’s not a lot of fun,” says Cheng. “But Sylvia had a lot going for her. She was very healthy, no pre-existing medical problems, no heart disease or diabetes, a good wound healer, educated and compliant and very motivated.
“And always a fantastic attitude—even when she could only wear big, ugly mumus, she made it fun.”
Word of Ennis’s accident spread quickly at Emory, leaving friends, co-workers, and colleagues in stunned disbelief.
They sprang into action, ferrying food to Ennis’s extended family in the waiting room, placing her name on church prayer chains, coming to visit by the dozens, and establishing a fund to help with medical bills.
“We knew it was almost unheard of, to recover from an injury like that,” says David Carlton, director for the Division of Neonatology in Emory’s Department of Pediatrics, where Ennis had worked. “But Sylvia is a very engaging individual who wants to do things the right way. When she’s in, she’s all in. Maybe that’s a quality that allows you to prevail.”
For Ennis, those points of connection made all the difference. “If it wasn’t for the Emory community, I don’t know if I would have wanted to live,” she says.
After two months at Grady, Ennis was transferred to a long-term acute care facility in Emory University Hospital Midtown for four more months of rehabilitation. When she was cleared for her first brief trip home, her sister, Janet Mitchell, “did a happy dance around my room,” Ennis recalls, laughing.
After 18 months of intensive therapy, she was upright and moving with a walker. During the first 22 months of her recovery, Ennis had spent just 30 days outside of a hospital. The ongoing surgical treatments seemed to unfold like chapters in a long, complicated novel. No. 11 was a skin graft. No. 12 was an ileostomy reversal. She lost track after 15 surgeries.
More than a year after the accident, Cheng and Carney teamed up for a co-surgery. Cheng wanted to perform final repairs on Ennis’s ruptured stomach muscles; Carney was determined to reattach her crushed ureter, freeing her from life with a nephrostomy bag.
When Carney had first seen Ennis’s injuries in the trauma room, he decided repair of her ureter could be postponed. Because of the force of the trauma, between four to five inches of the tiny conduit was missing. Waiting could help Carney pinpoint what tissues were irreparably damaged and what he had left to work with.
To allow Ennis’s right kidney to drain in the meantime, Carney had inserted a nephrostomy tube directly into the organ, diverting urine into an external bag. Now, because of her shortened ureter, Carney would have to rearrange Ennis's internal plumbing, repositioning her bladder and right kidney to accommodate her truncated ureter. After a year, multiple abdominal surgeries had resulted in a profound build-up of scar tissue. “It was really difficult—as if her bladder was encased in gristle,” he says.
Reattaching the shortened ureter took three to four hours, one of his tougher cases. “To be honest, we just barely had enough of the ureter to reach her bladder,” Carney says. “If another inch was missing I’m not sure I would have been able to put it back together. It was close.” In time, her kidneys, bladder, and ureter began functioning normally again, as did her intestinal tract.
“Her success was a team effort, a great partnering between Emory and Morehouse,” reflects Carney. “To be a part of her story was easily one of the biggest thrills of my life.”
As her treatment continued, Emory neurologist Michael Silver was drawn into Ennis’s case. It had been two years since the accident, but the pain in her right leg was actually getting worse.
Her nerves had been badly traumatized. In fact, the
tree had come close to hitting Ennis’s spinal cord.
To mitigate the pain of her neuropathy, he prescribed gabapentin—a medicine originally developed to treat epilepsy and seizures that can also be used to “tone down the signal in the nerves.” He also prescribed tramadol, a pain reliever to help her sleep, and nortriptyline, a tricyclic antidepressant used to control the brain’s reaction to pain.
Her next stop will be the Emory Center for Pain Management, where she’ll be treated with a spinal cord stimulator, a device that uses an electrical current to stimulate spinal nerves at such a high frequency they can’t read pain.
Of all the injuries Ennis sustained, pain and fatigue may be the primary lingering effects. “To some degree, I suspect that she will deal with the numbness, weakness, and pain for the rest of her life,” Silver says.
It is a battle that Ennis accepts. “No matter how much pain that I still feel every day, I rejoice in that pain, because I am blessed to feel anything,” Ennis says. “It could have just as easily gone the other way.”
Cheng is still working with Ennis, transferring fat cells to make sitting more comfortable for her. Watching Ennis’s progress, she says, reminds her of why she went into plastic surgery.
“In trauma surgery, you save people’s lives,” she says. “In reconstructive surgery, I like to think I’m giving them their quality of life back, the ability to return to as-close-to-normal as possible.”

CARE TEAM | Neurologist Michael Silver is helping Ennis manage her lingering nerve pain, especially in her leg.
Ennis refuses to be defined by the horrendous accident, the winding roadmap of surgical scars, the years of rehabilitation and physical therapy.
She talks readily about her gratitude and hopes for healing. She says she's blessed to be alive to see her 2-year-old granddaughter, McKenzie, who was born during the ordeal.
Though much of what she carries forward is invisible, Ennis is changed. She’s never revisited the scene of the accident and can’t bring herself to drive that section of Clifton Road.
Ennis thought seriously about having every tree in her yard cut down, instead settling for the removal of only one dying specimen. To this day, if a news story comes on television about falling trees, she changes the channel.
She hasn’t returned to her job at Emory and knows that may never be possible. Just sitting remains a challenge. There are small cognitive stumbles, such as when she pays a bill twice or forgets to write down a phone number. For someone who used to be the “go-to” person in her department—and a bit of a perfectionist—that’s frustrating.
“Just understanding the impact a trauma like this can have on you has been a learning experience,” Ennis says.
In December, Ennis closed the loop on something that was supposed to happen three years ago, joining her sister and friends on her long-delayed Caribbean cruise.
There were lazy moments in the tropical sunshine, good food, and generous amounts of laughter. But there was also a walker and fatigue and lingering discomfort. It was not the trip, nor the life, she had once envisioned—something she accepts.
As she confronts her own limitations, Ennis’ eyes have opened to the barriers people with physical disabilities face, trying to navigate daily tasks. She is thinking of going back to school to become a psychotherapist.
Looking back on her ordeal, Ennis harbors only one regret. She is haunted by the face at her car window. That anonymous man who called for the help that would save her.
You see, Ennis never caught his name.
And she would very much like to say, “Thank you.”